Celiac Disease Case Study
advertisement

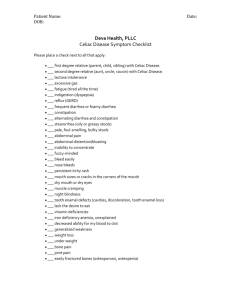
CELIAC DISEASE CASE STUDY Erin McNamara What is Celiac Disease? • Inherited autoimmune disease • Once onset occurs, affects individuals for life • Symptoms can appear at any time • Present at birth • Can be triggered by stress, surgery, infection, pregnancy or childbirth • 1 out of 133 people in the U.S. is affected Source: http://www.webmd.com What is Celiac Disease • Immune response to the wheat protein, gluten • Causes atrophy and damage to the mucosal villi of small intestine • If left untreated, damage can be chronic and life threatening • Increased risk of other immune and nutritional disorders Source: http://www.celiac.nih.gov/ Gluten • • • Found in wheat, rye, barley, and any foods containing these ingredients • Many processed foods contain gluten Also found in medicines, vitamins and lip balms Reading food labels is essential Source: http://www.noglutennaturalgirlproducts.com/ Source: http://www.eatright.org Source: http://thesavvyceliac.com Signs & Symptoms • Multi-symptom, multi-system disorder Direct Symptoms • abdominal cramping • gas • distention of stomach • chronic diarrhea • chronic constipation • fatty/foul-smelling stools • unexplained weight loss with large appetite Indirect Symptoms • osteopenia or osteoporosis • infertility • fatigue, lack of energy • depression • anemia • tingling or numbness in hands or feet • migraine headaches Treatment • Life-long adherence to a gluten- free diet • Many foods are naturally gluten- free • Fruits, vegetables, beef, poultry, fish, nuts, eggs • Source: http://glutenfreeoatmeal.net Wide variety of delicious and nutritious gluten-free options available Source: glutenfreeforlifeexpo1 Gluten-free Foods: • Amaranth • Corn • Quinoa • Millet • Rice • Lentils • Potato • Buckwheat • Soy • Wild Rice Case Study • Patient: Rachel • Gender: female • Ethnicity: Caucasian • Age: 33 • Height: 62” • Current weight: 105# • Usual weight: 125# • % UBW : 80% • BMI: 18.3 Source: http://www.eatright.org Case Study • Patient’s Symptoms • Rachel complains of extreme fatigue and weakness. She contributes these symptoms to stress and says she has been feeling depressed lately because she has been unable to get pregnant. She reports that she experiences intermittent bouts of diarrhea that smell very bad. Her chief concern is that she seems to be hungry all the time but keeps losing weight. Lately, she has noticed that everything she normally eats tends to make her feel bad. She says is tired of feeling bad all the time. Source: http://www.eatright.org Case Study • Patient History • Rachel states that she has been trying to get pregnant for a long time with no success. She says she’s always thought of herself as an energetic person, but thinks that the inability to get pregnant is taking a toll on her and that’s why she is so tired all the time. She has been a relatively healthy person but has a history of diarrhea episodes and occasional constipation. Reports her mom has always had GI issues and had trouble maintaining her weight. Rachel’s niece (her sister’s daughter) was just diagnosed with celiac disease. Case Study • Typical Daily Intake • Breakfast • 1 English muffin or 2 slices whole wheat toast, 1 tbp. peanut butter, 1 sm. apple • • • • • or orange, 1 c. skim milk, 1 c. coffee, 1tbp. half & half Snack • handful of pretzels or cut up vegetables & ranch dip Lunch • ½ c. barley mushroom soup or chicken noodle soup , 2 slices whole wheat bread, 2 oz. roast beef, 1 tsp. light mayo, romaine lettuce, 1 bag of potato chips Snack • whole wheat pita with hummus or crackers and cheese Dinner • 1c. regular or whole wheat pasta, 1 turkey sausage link. 1c. canned tomato sauce, 2 oz. italian bread, 1c. steamed broccoli Dessert • 1 chocolate chip cookie or ½ c. ice cream, 1tbp. chocolate sauce **Diet has consisted of chicken soup and crackers the past few days because of not feeling well. Case Study Lab Values of Concern Recommendations Recommendations Recommendations Recommendations Recommendations Recommendations ADIME Note A: Pt. appears thin and moderately concerned because of weight loss despite being hungry all the time. States that she is extremely tired and weak and reports bouts of foul-smelling diarrhea with occasional constipation. She has been unsuccessful at getting pregnant and reports feeling depressed over the situation. Family Hx: Mother - GI issues (possible celiac), Niece (sister’s daughter) celiac disease Current diet order: 100 g fat for 3 days prior to fecal fat test Medications: kaopectate on occasion Admit Dx: celiac disease, mild malnutrition, malabsorption & anemia Gender: Female Age: 33 y/o Height: 62” Current Wt: 100# BMI: 18.3 (underweight, mild malnutrition) Usual Wt: 125# UBW%: 80% Labs: Albumin = 2.8, Prealbumin = 5.4, tTG = positive, HgB = 9.4, HCT = 34, Ferritin = 13, Fecal fat - 17g D: Unintentional weight loss (NC - 3.2) RT newly diagnosed celiac disease AEB current weight 100#, usual weight 125#, 80% of UBW and BMI of 18.3. Altered GI function (NC -1.4) RT new diagnosis of celiac disease AEB Albumin = 2.8, Prealbumin = 5.4, HCT = 34, Ferritin = 13 and Fecal fat = 17, and tTG = positive. I: Purpose of nutrition education (E - 1.1) Provide knowledge of adapting a gluten-free diet to manage symptoms of celiac disease to pt. & husband. Mineral (ND - 3.2.4) Iron supplement intake to treat anemia. M: Modified diet (FH - 2.1.1.2) Follow-up on adherence to gluten-free diet. Pt. & husband will follow a gluten-free diet. E: Weight (AD - 1.1.2), Fecal fat (BD - 4.12), Ferritin, serum (BD.10.10), Albumin (BD - 1.11.1), Prealbumin (BD 1.11.2) Treatment Plan • Rachel’s lab results confirm a diagnosis of celiac disease. To relieve her symptoms, I would recommend she follow a gluten-free diet. Strong, imperative evidence from EAL reports that a life-long adherence of a gluten-free diet improves gastrointestinal issues, iron deficiency and quality of life. Due to Rachel’s anemia related to iron deficiency, a strong, conditional recommendation for these individuals includes a diet supplemented with a gluten-free multivitamin containing iron. • It is important to teach Rachel and her husband that many products contain gluten. To ensure complete integration of a gluten-free diet, consensus, imperative EAL evidence recommends educating individuals on labelreading of foods and supplements. This education is to help identify sources of gluten in products to assist with the overall management of celiac disease. Source: http://www.gluten.net/ Treatment Plan • Changing to a gluten-free diet may be challenging at first for Rachel. It is important to show Rachel that eating gluten-free does not mean that she can enjoy foods that she loves. I would recommend accompanying her to the grocery store to show her the variety of gluten-free foods available. There are many glutenfree alternatives available for the foods that Rachel likes to enjoy. Source: http://www.webmd.com Treatment Plan • It would also be beneficial for her to have cooking lessons to help teach her how to use the gluten-free alternatives in her cooking. Learning how to use the glutenfree products to make the foods she loves will help strengthen her adherence to a gluten-free lifestyle. • Once Rachel has been educated on a gluten-free diet and adapted to eating this way, a follow-up evaluation will be scheduled. Biochemical lab value testing and a fecal fat test will be administered to evaluate her adherence to a glutenfree diet. What I learned • The Evidence Analysis Library is a very useful reference tool. Prior to this class, I did not know how to use the information given in the EAL. Now I know how to navigate through the topics, read and understand the recommendations. I find the way the recommendations are rated make it easy to understand which recommendations would be applicable to each individual case. This made it easy for me to identify which recommendations. I could use for my case study. I also learned how each topic undergoes much research to ensure the information is adequate and valid. • The EAL is a tool that I will continue to use now and in the future. There are many resources available for anyone to see, but it is important for the dietetics profession to have accurate, specific information that can be used in practice. The EAL is a great reliable source and feel fortunate to have learned how to use it and have access to it. References • Academy of Nutrition and Dietetics. (2009). “Evidence-based Nutrition Practice Guideline on Celiac Disease.” Academy of Nutrition and Dietetics Evidence Analysis Library. Retrieved from http://andevidencelibrary.com/topic.cfm?cat=3726. • American Association for Clinical Chemistry. (2012). Celiac disease: Tests. Lab Tests Online. Retrieved from http://labtestsonline.org/understanding/conditions/celiac/start/2 • National Digestive Diseases Information Clearinghouse. (2012). Celiac disease. National Digestive Diseases Information Clearinghouse. Retrieved from • http://digestive.niddk.nih.gov/ddiseases/pubs/celiac/ • Mahan, L.K., Escott-Stump, S., Raymond, J.L. (2012). Medical nutrition therapy for lower gastrointestinal tract disorders. Krause’s Food and the Nutrition Care Process (pp.618-622). St. Louis, MO: Elsevier. • Ruiz, A.R. (2012). Celiac disease: Malabsorption Syndrome. The Merck Manual. Retrieved from http://www.merckmanuals.com/professional/gastrointestinal_disorders/malabsorpti on_syndromes/celiac_disease.html