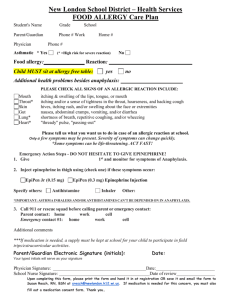
L_Food-Allergies
advertisement

Serving up Safety: Educating Students with Food Allergies in Compliance with State Law and Section 504 Janet Little Horton Thompson & Horton LLP 3200 Southwest Freeway, Suite 2000 Houston, Texas 77027 jhorton@thompsonhorton.com 713-554-6746 What is a food allergy? • Abnormal response to a food. • Triggered by the body’s immune system. • Symptoms may be mild to life- threatening. • Reactions vary from person to person • Severity of the allergic reaction is not predictable. • 18% increase 1997 to 2007 (Centers for Disease Control and Prevention). • Current estimate: 1/13 to 1/25 children • • • • • now affected. And 40% report history of severe reaction. No cure for food allergies. Reaction within a few minutes to a few hours. 90% of reactions caused by milk, eggs, peanuts, tree nuts, fish, shellfish, soy, and/or wheat. But any food has the potential to cause a reaction. Food allergy v. food intolerance • Food allergy – medical history, lab work, and other diagnostic tests = medical diagnosis by a licensed health care provider. vs. • Food intolerance – does not involve immune system; not life-threatening. Concerns in the school context • Concerns with food served. • Concerns with food brought by others. • Concerns with school supplies. • Concerns with cross contamination. • Strict avoidance and early recognition and management of symptoms are critical. What is anaphylaxis? • Serious allergic reaction. • Rapid in onset (several minutes to a few hours). • Wide range of symptoms. • May cause death. • Treatment – epinephrine. • May involve mouth, throat, nose, ears, eyes, lungs, stomach, skin, heart. • Resources on anaphylaxis in children available from the Food Allergy and Anaphylaxis Network (FAAN): http://www.foodallergy.org/page/how-a-childmight-describe-a-reaction1 • After epinephrine administration, transport to hospital. What does Texas law require concerning the management of food allergies in the school setting? TEC § 38.0151 – Policies for Care of Certain Students at Risk for Anaphylaxis Requires each school district and open-enrollment charter school to adopt and administer a policy for the care of students with a diagnosed food allergy at risk for anaphylaxis based on guidelines developed by the commissioner of state health services in consultation with an ad hoc committee appointed by the commissioner of state health services. Guidelines may not: Require school to purchase prescription medication. Require expenditure that would result in negative fiscal impact. Require personnel to administer anaphylaxis medication unless it is prescribed for the student. TEC § 38.0151 does not: Waive any liability or immunity of district or its officers or employees. Create liability or a cause of action against district, its officers or employees. Guidelines for the Care of Students with Food Allergies At-Risk for Anaphylaxis To Implement Senate Bill 27 published here: http://www.dshs.state.tx.us/WorkArea/Dow nloadAsset.aspx?id=8589966589. The guidelines include sample forms. Requirements of the Guidelines 1. Identification of students with food allergies at-risk for anaphylaxis. 2. Development, implementation, communication and monitoring of emergency care plans and/or individualized health care plans. 3. Reducing the risk of exposure through environmental controls. 4. Training for school staff on food allergies, anaphylaxis and emergency response. 5. Post anaphylaxis reaction review of policy and procedures. District-wide coordination: • Appointment of Superintendent designee • • • • (“May”). Central point of contact. Convene multi-disciplinary team. Receive ongoing training on food allergy management and the administration of epinephrine. Work with the School Health Advisory Council (TEC § 28.004). Campus coordination: • Food Allergy Management Team (“May”). • Implement, coordinate, and monitor food allergy management on campus. 1. Identification: Upon enrollment of a child in public school, the district shall request that the parent disclose whether the child has a food allergy or a severe food allergy, specify the food(s) to which the child is allergic, and the nature of the reaction. Tex. Educ. Code § 25.0022 2. Development, implementation, communication and monitoring of emergency care plans and/or individualized health care plans. When there is a medical diagnosis of a food allergy, a Food Allergy Action Plan and Emergency Action Plan (FAAP/EAP) may be developed by health care provider and parent. The student’s FAAP/EAP plan should include: Student’s name. Date of birth. Grade level. Photograph. List of foods to which child is allergic. Indication of whether student has asthma. Description of past allergic reactions. Clear instructions on what symptoms require use of epinephrine immediately. Clear instructions on how to administer epinephrine, what to do once epinephrine is administered, and specifics on any other emergency medication for the child. Contact information for parents and other emergency contacts. Signature and date for parent, healthcare provider, and school representative. Student, parents, school nurse, campus food allergy management team meet to review, get all consents signed – prior to the student attending school. School nurse may develop Individual Health Plan (IHP). 3. Reducing the risk of exposure through environmental controls. The Guidelines include a list of considerations, including: Identifying high-risk areas. Limiting or eliminating food from learning environments. Notifying and educating the school community. Developing procedures for parent-provided snacks. • Cleaning protocols. • Training to food service. • Educate students – no swapping or sharing • FAAN has a good curriculum developed for this • • • • • purpose (http://www.foodallergy.org/section/bea-pal-program). Hand washing. Staff trained to administer epinephrine. Ready access to epinephrine. Risk reduction – bus, extracurriculars. No bullying. 4. Training for school staff on food allergies, anaphylaxis and emergency response. Training needs to include school staff responsible for the care of individual students, the food allergy management team, and substitute staff. Training needs to be comprehensive and is one of the areas where OCR has been the most critical of schools. • Under state law, this training needs to include staff training on food allergies, signs and symptoms of anaphylaxis, and emergency response. 5. Post anaphylaxis reaction review of policy and procedures. Review of the policies and procedures should happen at least annually. Review should also happen after a student experiences an allergic reaction at school (even if the reaction is not anaphylaxis) in order to promote the student’s safe return to school – are changes needed? Education Code § 22.052 makes it clear that school district employees are immune from liability for administering medication if the school district has received a written request to administer the medication from the parent; and the medication is in its properly labeled original container – the only exception is gross negligence. Other Texas Laws Involved in the Education of Students with Food Allergies A student who meets certain criteria is allowed to possess and self-administer medication for asthma or anaphylaxis. Must possess the skill and knowledge to selfadminister (school staff should still be trained to administer epinephrine in an emergency). Must have a written authorization from parent. Must have a written authorization from physician. Tex. Educ. Code § 38.015 Student health records must be kept confidential. Tex. Educ. Code § 38.009. (a) A school administrator, nurse, or teacher is entitled to access to a student's medical records maintained by the school district for reasons determined by district policy. (b) A school administrator, nurse, or teacher who views medical records under this section shall maintain the confidentiality of those medical records. (c) This section does not authorize a school administrator, nurse, or teacher to require a student to be tested to determine the student's medical condition or status. Are students with food allergies, including those at-risk for anaphylaxis, covered by Section 504? Does the student have a physical or mental impairment that substantially limits a major life activity? Section 504 Rules of Construction: 1. Construe eligibility broadly – more inclusive. 2. “Substantially limits” is not a high standard. 3. Episodic conditions or those in remission – consider as if full-blown. 4. Mitigating measures may not be considered (except eyeglasses and contacts). • Mitigating measures include medication, assistive technology, reasonable accommodations, auxiliary aids and services. 5. A person need only be impaired in 1 major life activity to be covered by Section 504. Substantial impairment in learning is not required. Major Life Activities (include, but are not limited to) • Caring for one’s self, performing manual tasks, seeing, hearing, speaking, breathing, learning, working, eating, sleeping, walking, standing, lifting, bending, reading, concentrating, thinking, and communicating. Major Life Activities also include Major Bodily Functions • Immune system, normal cell growth, digestive, bowel function, bladder function, neurological, brain, respiratory, circulatory, endocrine, and reproductive functions. Student with a food allergy at-risk for anaphylaxis • Physical impairment. • Substantially limits immune system. • Consider as if full-blown. • May implicate digestion, breathing, etc. • Disregard mitigating measures such as epinephrine, IHP, FAAP/EAP. Evaluation for 504 Eligibility • District cannot refuse Section 504 evaluation because food allergy does not affect major life activity of learning. • North Royalton (OH) City School District, 52 IDELR 203 (OCR 2009) (student with food allergy). • Tyler ISD, 56 IDELR 24 (OCR 2010) (student with diabetes). • Prevail Academy, 109 LRP 32521 (OCR 2009) (student with food allergy). Evaluation must meet Section 504 Requirements Evaluation materials validated and tailored to assess specific areas of educational need. Information from a variety of sources. Information is documented and carefully considered. Placement decisions made by persons knowledgeable about student, meaning of evaluation data and placement options. Saluda (SC) School District One 47 IDELR 22 (OCR 2006) – OCR describes what should be in written plans to respond to food allergy: 1. Adequate policies, procedures and/or protocols governing the student’s allergy risk management in each type of school program and activity, including the student’s classroom and common use rooms (e.g. the cafeteria, library, computer labs, gymnasium, and art and music rooms), and during recess periods, bus transportation, field trips, and extracurricular, school-sponsored activities. 2. Sufficient emergency response policies, procedures and/or protocols covering all school programs and activities to address instances in which the student is suspected of having an allergic reaction. These procedures should address the proper handling and administration of epinephrine in the event of anaphylactic or other serious allergy-related reaction, and will identify the staff responsible for emergency responses. 3. A provision that all district staff responsible for the immediate custodial supervision or care of the student (including substitutes) will receive comprehensive training on the student’s allergy and the implementation of the student’s plan. The plan should establish when, how often, for how long, and by whom the training is conducted, as well as the content of this training. 4. A provision requiring that at least one staff person fully trained in the student’s allergy be at the school during all regular school hours and at all school-related activities attended by the student who can administer epinephrine consistent with the district’s allergy-related policies, etc. 5. Provisions setting out all of the allergyrelated responsibilities of parents and students in all school programs and activities and an effective process for communicating their allergy-related responsibilities to them, and what sanctions are applicable to individuals who harass students with allergies because of those allergies. FAPE under 504 Provision of regular or special education and related aids and services designed to meet unique needs of student with a disability as adequately as the needs of non-disabled students are met “As the vast majority of District students without disabilities do not face a significant possibility of experiencing serious and life-threatening reactions to their environment while they attend District schools, Section 504 and Title II require that the District provide the Student with an environment in which he also does not face such a significant possibility.” Saluda (SC) School District One, 47 IDELR 22 (OCR 2006). Dracut (MA) Public Schools, 110 LRP 48748 (OCR 2012) Does impairment substantially limit one or more major life activities? Does it limit student’s access to educational services and activities? If so, what services are needed to provide FAPE – access to classroom and all other school services and activities? Examples of accommodations/ modifications acceptable to OCR and based on the student’s individual needs: • An “allergen-free” or “food-free” classroom; • Cleaning areas potentially contaminated with allergen in a special way (e.g. mopping with water that is not used to mop other classrooms); • Appropriate training; • Sending a letter to parents of other students in the class explaining that there is a student in the class with a food allergy, and asking parents not to send foods containing the allergen; • Not using food as a reward in the class; alternate treats; • Offering educational seminars regarding food • • • • • allergies to the class or to the school’s parents; Providing an aide to monitor the student at school and on the bus trained to administer epinephrine, if needed; Allowing the student to keep a cell phone with him or her; Allowing the student to keep epinephrine; An allergen-safe area in the cafeteria, which is cleaned using special procedures; Allowing the student to sit separately in the lunchroom with a friend whose parents have agreed to avoid the student’s allergen; • The use of wipes to clean an area before the • • • • • student uses/sits in it in the classroom, cafeteria, bus, and on field trips; An adult-to-adult transfer plan to ensure that the student’s epinephrine is always close at hand, coupled with training for those adults; Daily vacuuming of the classroom carpet; daily washing of the desks in the classroom; Daily hand washing by everyone when they enter the classroom for the first time and after snack, recess, and lunch break; Newsletters at holiday times reminding other students’ parents of the classroom’s food policies; Notifying the student’s parents before birthday parties and celebrations involving food. Cutoosa County (GA) School District, 57 IDELR 141 (OCR 2011) Student’s parents explained severity of student’s allergy to peanuts. Sale of peanut products from vending machines continued for 9 more months. Principal tried to eliminate products – finally removed vending machines. Failure to remove products earlier was harassment. It was sufficiently severe, pervasive or persistent to create a hostile environment. Actions to correct the problem were neither prompt nor effective. Plumas (CA) Unified School Dist., 55 IDELR 265 (OCR 2010) • District denied parent’s request for peanutfree school. • District did not make a record of any of the information gathered, nor did they discuss with the parents at the 504 meeting the reasons behind denying the parent’s request for a peanut-free school. • A request for such an accommodation cannot be categorically rejected. The parents were also not provided the appropriate notice of Section 504 procedural safeguards, including “notice of the action, an opportunity to examine relevant records, an impartial hearing with opportunity for participation by parents or guardians and representation by counsel, and a review procedure.” • The parents must be able to challenge the plan and must be given, by the District, the information on how to challenge the Plan with which they disagree. Does the District have to provide special food for students with food allergies? • Maybe. • For students eligible for free or reduced lunch, the USDA says, “U.S. Department of Agriculture's (USDA) nondiscrimination regulation (7 CFR 15b), as well as the regulations governing the National School Lunch Program and School Breakfast Program, make it clear that substitutions to the regular meal must be made for children who are unable to eat school meals because of their disabilities, when that need is certified by a licensed physician.” See FNS Instruction 783-2, Revision 2, Meal Substitutions for Medical or Other Special Dietary Reasons; see also http://www.fns.usda.gov/cnd/guidance/special _dietary_needs.pdf This publication also discusses potential funding sources in the event the meal preparation for a particular student is much more costly. • For a student with life-threatening, “severe” food allergies who receives free or reduced lunch, the District should plan to make substitutions and other changes. • For other students who require dietaryrelated accommodations, whether the student should be provided with special food or given a place to store special food is based on the student’s needs and the determination of the appropriate personnel (Food Allergy Management Team, 504 Committee, ARD Committee, etc.). Training of School Staff Under 504 Saluda (SC) School District One, 47 IDELR 22 (OCR 2006) - training for District staff regarding a student with a peanut/tree nut allergy (PTA) should include “topics such as the following:” 1. Recognizing the symptoms of a PTA emergency; 2. Common causes of PTA emergencies; 3. Understanding and properly implementing food allergy plans; 4. The contents of the food allergy plans of the students with PTAs for whom each district staff person has immediate custodial or care responsibilities; 5. Properly and safely handling, administering and storing antihistamines and epinephrine; and 6. Detailed instruction on district PTA policy, procedures, protocols, and practices. • Presumably, these requirements can be generalized to all students with food allergies, and adjusted based on the student’s individual needs. • Districts must be careful that even substitutes receive this training. State guidelines only add to this that staff should also be trained in: • Identifying students at-risk and planning • • • • for students who do not have epinephrine at school. Development of IHPs/504 Plans. Environmental controls. Working with local EMS. Post anaphylaxis debriefing and monitoring of food allergy management plans. Pine-Richard (PA) School District, 53 IDELR 200 (OCR 2009) • OCR found problems where a school nurse had a 2nd grader with life-threatening food allergies stand up in front of her class and discuss her allergies. • The nurse had not obtained parental consent. • The discussion involved language such as “she could die.” Homebound instruction – for a food allergy General Education - EEH (Local) • Student confined a minimum of 4 weeks to • • • • home/hospital. For medical reasons. Documented by a licensed physician. Transitory – meant to facilitate the student’s return to school. Done by campus placement committee. Can a student with a food allergy at-risk for anaphylaxis qualify under IDEA? Maybe . . . • Other Health Impairment (OHI) – limited strength, vitality or alertness that is due to a chronic or acute health problem and that adversely affects the student’s educational performance and who, because of the condition, needs special education and related services. Reg. 300.8(c)(9) • Any decision would be made on a case- by-case basis by the ARD Committee based on a full individual evaluation. If the student with a severe food allergy qualifies as an IDEA student: • Full continuum of alternative placements must be available (Reg. 300.115). • Home instruction would be a possibility if the risk of exposure at school could not be reduced to an acceptable level. Homebound placement based solely on parent preference is not appropriate: • Gwinnett County Sch. Dist., 56 IDELR 118 (SEA GA 2010) (parent wanted homebound to administer nonprescription nutritional supplements during the school day). • Poway Unified School District, 53 IDELR 208 (SEA CA 2009) (parent wanted homebound, in part, because of “leaky gut syndrome” and fears about safety at school). Nothing in IDEA requires a district to provide a full day of instruction to homebound student, or to provide same amount of special education instruction student would have received at school. • Georgetown Indep. Sch. Dist., 45 IDELR 116 (SEA TX 2005); • Greenville Indep. Sch. Dist., 102 LRP 12471 (SEA TX 2002); • Renton Sch. Dist., 111 LRP 72136 (SEA WA 2011). But homebound is not “one size fits all.” If it is not individualized, it may fail to provide FAPE. • Trico County Unit. Sch. Dist. 176, 108 LRP 42817 (SEA IL 2008); • Torrance Unified Sch. Dist., 111 LRP 19380 (SEA CA 2011). To Sum Up…. 1. Districts must have policies and regulations in place to seek information from parents about food allergies and respond to food allergies with appropriate plans. 2. District policies and regulations should comply with the Guidelines. 3. Students with a food allergy at-risk for anaphylaxis will most likely be covered by Section 504, although IDEA eligibility may be appropriate in some cases. 4. All Section 504 procedures should be followed for evaluation, placement and the development of a Section 504 plan. 5. The FAAP/EAP/Individual Health Plan may be the only Section 504 plan the student requires. 6. Food allergy diagnoses are increasing. These conditions must be taken seriously by school staff. 7. Training of staff is important. Document the training. Janet Little Horton Thompson & Horton LLP 3200 Southwest Freeway, Suite 2000 Houston, Texas 77027 713-554-6746 jhorton@thompsonhorton.com www.thompsonhorton.com © 2012