Sepsis Prevention in ICU Patients
advertisement

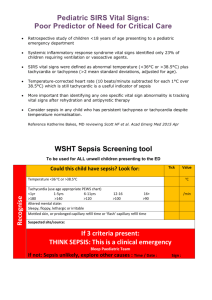
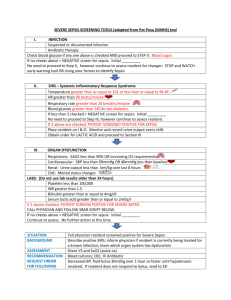
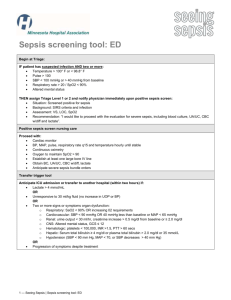
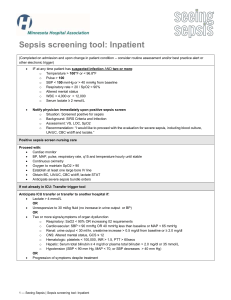
Sepsis Prevention in ICU Patients JESSICA WILBORN Data Reports 750,000 cases per year Sepsis is expected to increase by 1.5% per year and there will be a significant increase among the elderly Severe sepsis is the leading cause of morbidity and mortality worldwide The annual health costs is $24 billion Sepsis patients have a 75% longer hospital stay compared to patients with other conditions Patients hospitalized for septicemia are eight times more likely to die during the hospital stay Research indicates 36% improved odds of inpatient survival rate among Emergency Departments that see higher numbers of sepsis patients (depends on hospital location and teaching status) http://www.cdc.gov/sepsis/datareports/index.html Sepsis A life threatening condition where the body attacks its own tissues and organs in response to infection Severe sepsis is progression to cellular dysfunction, organ damage, hypoperfusion, Sepsis (infection + 2+ SIRS criteria) Severe sepsis (infection +SIRS criteria +organ dysfunction) Sepsis can occur in any setting and with any patient Systemic Inflammatory Response Syndrome (SIRS) SIRS typically precedes sepsis Characterized as: Temperature >38 or <36 Heart rate more than 90bpm Respiratory rate greater than 20 breaths/min WBC count greater than 12,000 cell/mm3 or greater than 10% immature bands Hyperglycemia Altered mental status Signs & Symptoms of Sepsis Fever Chills Tachycardia Tachypnea Abnormal lab values Low blood pressure SBP <90mmHg MAP < 70 mmHg Dehydration Altered mental status Reduced urine output Sepsis & the elderly Older patients may present with atypical symptoms or may be absent Atypical symptoms include delirium, falls, loss of appetite, weakness, malaise, and fever can be absent or subdued Often these patients experience a delay in treatment Poor nutrition and low immune system significantly increase the risk of sepsis Existing comorbidities metastatic neoplasms (43%), chronic liver disease (37%), and chronic renal disease (36%) significantly increase risk of sepsis related mortality Frequently gram negative bacilli is detected. However, gram positive bacilli becoming common due to broad spectrum antibiotic use Higher mortality among the elderly (40-50%) compared to individuals <65 Factors to predict prognosis in critically ill patients Pre-infectious status Gender Age Nosocomial events Comorbidities Severity of Illness Vulnerable Populations Young children Older people Long-term invasive devices Immunocompromised Nurse role in prevention According to the Nursing Times, “Nurses have a important role in detecting patients with a deteriorating condition and initiating life-saving treatments” (McClelland, H.,and Moxon, A., 2014, p.17) Recognize the symptoms and risk factors for sepsis pertaining to the patient Referral to physician and interdisciplinary team Initiate Surviving Sepsis Campaign Care Bundle Within 3 hours: measure lactate, obtain blood cultures, administer broad spectrum antibiotics, administer 30 ml/kg crystalloid for hypotension or lactate ≥ 4mmol/L Within 6 hours: apply vasopressors for hypotension, MAP ≥65 mmHg, CVP 812mmHg, ScvO2 of ≥70%, remeasure lactate levels Prevention Methods Identify risk factors increasing susceptibility: infections, open wounds, long term invasive devices, invasive procedures, chemotherapy and anti-cancer treatments, pneumonia, and skin or soft tissue inflammation Screening significantly increases prevention and decreases sepsis related mortality Inservice training-poster, pocket guide, or badge reference of sepsis protocol and incorporated in new employee orientation and recertification Implementing infection control practices Communication of nurse to interdisciplinary team Routine clinical assessments-vital signs and perfusion status SSC Bundle Care- improves delivery of adequate care across all clinical settings References Aitkin, L., Schorr, C., Kleinpell, R. Implications of the new international sepsis guidelines for nursing care. American Journal of Critical Care. 22, 3, 212-222, May 2013. ISSN: 10623264 Destarac, A.L., Ely, W.E. (2012). Sepsis in Older Patients: An Emerging Concern in Critical Care. Advances in Sepsis, 22(1), 15-22 CDC (2014). Data Reports. Retrieved from http://www.cdc.gov/sepsis/datareports/index.html Gaieski, D. F., Edwards, J. M., Kallan, M. J., Mikkelsen, M. E., Goyal, M., & Carr, B. G. (2014). The relationship between hospital volume and mortality in severe sepsis. American Journal of Respiratory and Critical Care Medicine, 190(6), 665-74. Retrieved from http://search.proquest.com/docview/1563097740?accountid=14589 Gille-Johnson, P., Hansson, K. E., & Gårdlund, B. (2013). Severe sepsis and systemic inflammatory response syndrome in emergency department patients with suspected severe infection. Scandinavian Journal Of Infectious Diseases, 45(3), 186-193. doi:10.3109/00365548.2012.720025 Lopez-Bushneil, K., Demaray, W. S., & Jaco, C. (2014). Reducing Sepsis Mortality. MEDSURG Nursing, 23(1), 9-14. McClelland, H., Moxon, A., (2014). Early identification and treatment of sepsis. Nursing Times. 110(4), 14-17 Miller,Russell R., I.,II, Dong, L., Nelson, N. C., Brown, S. M., Kuttler, K. G., Probst, D. R., . . . Clemmer, T. P. (2013). Multicenter implementation of a severe sepsis and septic shock treatment bundle. American Journal of Respiratory and Critical Care Medicine, 188(1), 77-82. Retrieved from http://search.proquest.com/docview/1439092853?accountid=14589