The Cardiovascular System
The Cardiovascular System
•Your Heart and Stuff
The Cardiovascular System
includes the heart, blood vessels, and blood.
Cardiology- the study of the heart and the diseases associated with it.
1.
2.
3.
Functions to supply cells & tissues with oxygen to circulate substances & nutrients to remove wastes (CO
2
from cells and tissues.
& urea)
Heart Coverings
Pericardium – covers the heart, has 3 layers
Fibrous pericardium - outermost
Parietal pericardium - middle
(Pericardial cavity)
Visceral pericardium (continuous with epicardium) - innermost
The Heart Wall (3 layers):
1.
2.
3.
epicardium (visceral pericardium)
– reduces friction myocardium - cardiac muscle tissue (bulk of heart) endocardium – smooth inner lining of heart chambers and valves.
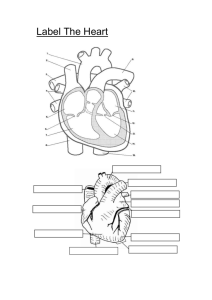
Heart Chambers
The upper chambers – atria (atrium) blood flows here
1 st . Pumps to ventricles
The lower chambers – ventricles, pump blood out to body or lungs.
The right side of your heart receives blood (deoxy) from the body and pumps it to the lungs.
The left side of the heart receives blood (oxy) from the lungs and pumps it out to the body
A solid wall-like septum separates the atrium and ventricle on the right from those on the left – so blood on one side never mixes with blood on the other side
Why is this the right side?
And this the left?
Heart Valves
Tricuspid Valve –btwn RA and RV
Pulmonary Valve –allows blood to leave
RV
– Pulmonary means lungs.
Bicuspid (mitral) Valve – btwn LA and LV
Aortic Valve – allows blood to leave LV
What color is blood?
Blood when oxygenated is red
However, deoxygenated is not blue as believed. It is actually a redish purple.
It appears blue because the color is diffused looking through the skin
This is also why veins typically appears almost green in African-Americans.
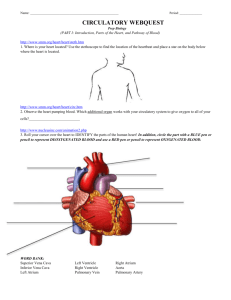
Blood Flow
Blood low on O
2
(deoxygenated) enters
Right Atrium through the superior and inferior venae cavae and coronary sinus
Right Atrium wall contracts, and blood passes thru tricuspid valve into Right
Ventricle (only adds 30% of vol. to RV)
Right Ventricle contracts, and blood is forced thru pulmonary valve into pulmonary trunk divides into pulmonary arteries(left & right) to lungs
Blood Flow cont.
pulmonary arteries take blood to lungs; gas exchange occurs between blood and air in alveoli
Carbon Dioxide is released. Oxygen is taken in. Blood goes from deoxygenated to oxygenated
Freshly oxygenated blood returns to heart thru the pulmonary veins that lead to Left Atrium
Blood Flow cont.
Left Atrium wall contracts, and blood moves thru bicuspid valve into Left Ventricle
Left Ventricle contracts, blood moves thru aortic valve and into the aorta aorta carries oxygenated blood to tissues
Oxygen to tissues, Carbon Dioxide made in tissues released into blood
Deoxygenated blood is sent back to heart thru superior and inferior vena cava
Heart Sounds
Heart sounds are produced by vibrations in the tissue associated with the closing of the valves.
The first part of the heart sound (lubb) is heard during ventricular contraction when the valves between the Atrium & Ventricles closes.
The closing causes the blood to stop flowing or back up causing a sound almost like waves crashing on a beach. They do not make a sound until they crash. Blood does not make a sound when flowing; only when it is stopped and crashes into heart valve.
Heart Sounds cont’d
The second part of the heart sound (dubb) happens during ventricular relaxation when the pulmonary and aortic valves snap shut
Heart sounds give doctors an indication of how well the valves are functioning (ex: murmurs)
Mitral Valve prolapse is usually identified by lubb-dubb-squish. The squish is the valve closing improperly and some blood still is leaking through.
National geographic website
Here the heart Hit next twice
Cardiac Muscle fibers
Cardiac fibers are highly branched, so when any part of the network is stimulated, the whole unit contracts (called a functional syncytium)
There are 2 syncytia – the atrial syncytium and the ventricular syncytium
Conduction of a cardiac impulse:
Starts at the sinoatrial (S-A) node located in the RA
The S-A node is self-exciting (no outside stimulation needed) and is rhythmic (initiates 70-80 impulses/min. in an adult)
Called the “pacemaker”
Conduction of a cardiac impulse:
impulse generated by the S-A node causes the atrial syncytium to contract
impulse then travels to the atrioventricular (A-V) node located in the septum that separates the atria
Conduction of a cardiac impulse:
impulse is delayed as it passes thru the A-V node, allowing time for the atria to empty and the ventricles to fill with blood
impulse then travels thru a bundle of fibers called the bundle of His located in the interventricular septum.
Conduction of a cardiac impulse:
The bundle of His gives rise to Purkinje fibers
The Purkinje fibers extend down into the apex of the heart and curve upward thru the walls of the ventricles
As impulse passes thru Purkinje fibers it stimulates the ventricular syncytium to contract
Ventricles squeeze up from the bottom of V to squeeze blood out of heart.
Blood vessels
Arteries
– carry blood away from heart; strong, thick; carry blood under high pressure; composed of mainly smooth muscle tissue
– Not always oxygenated blood . Pulmonary artery takes deoxygenated blood to lungs away from heart.
– Are typically deeper than veins
Arteries subdivide into smaller tubes called arterioles.
Blood vessels cont’d
Capillaries
– are the smallest blood vessels. They connect the arterioles with the venules.
– Capillary walls are thin enough to allow substances to pass through such as O2 & CO2
– Capillaries are microscopic and are only big enough for one red blood cell to go through at a time. If you can see it; it is not a capillary.
– 10-40 billion capillaries in your body
– No cell is 1/100 of cm from a capillary
Blood vessels cont’d
Veins
– Venules are small vessels that merge to form veins; parallel to arterioles
– these vessels carry blood back to heart and are not always deoxygenated.
– Venules and veins have thinner walls than arteries because the blood pressure is less.
The Cardiac Cycle
The series of events that constitute a heartbeat
– The atrial walls contract; the ventricle walls are relaxed
– The ventricle walls contract; the atrial walls relax
– Both the atria and the ventricles relax
– Ventricle contractions control blood pressure
– Contracting – systole
– Relaxation - diastole
Blood Pressure
The force blood exerts against the inner walls of blood vessels
Usually refers to the pressure in the arteries supplied by the aorta
When the ventricles contract blood moves into the aorta and pulmonary trunk, increasing pressure
maximum pressure during ventricular contraction is called the systolic pressure
Blood Pressure
When ventricles relax, arterial pressure drops
The lowest pressure before the next ventricular contraction is called the diastolic pressure
If there’s a drop in blood pressure, walls of veins constrict, helping to maintain blood pressure by returning more blood to heart.
(Less blood in veins if veins are smaller)
This ensures a nearly normal blood flow even when as much as 25% of blood volume is lost.
Taking Blood Pressure
Normal Blood Pressure 120/80.
Increase blood pressure until can not hear any flow because artery closed. Cuff pressure is greater than systole & diastole so blood vessels closed all the time. (Contraction & Relaxation)
Taking Blood Pressure
Let blood pressure come down until under
120. During Systole (contraction), pressure in arteries is greater than cuff, so artery open only during systole
But during diastole (relaxation) pressure of cuff is greater than pressure in blood vessels so blood vessels are closed.
Taking Blood Pressure
The walls of the blood vessels go in and out causing turbulent flow of blood.
Can hear turbulent flow because walls of arteries going in and out do to change in pressure.
Under 80 silent because cuff pressure less diastole pressure so arteries stay open.
Blood pressure always recorded as systolic = 120 diastolic 80
Pulse Rate
The pulse rate is equal to the rate at which the ventricles contract or equal to heart rate.
The pulse is the alternate expanding and recoiling of the artery walls.
Pulse
Blood vessel disorders
Arteriosclerosis- degenerative disease in which the arteries lose elasticity; the vessels become brittle and can rupture easily; associated with fatty diet, genetics, lack of exercise, cigarette smoking, etc.
Go to Heart Attack Then Blocking the
Artery to watch video
Arteriosclerosis
Blood vessel disorders
Aneurysm- a bulge in a blood vessel; this area of the blood vessel then weakens and may burst; can result from trauma, high blood pressure, infections, or genetic defects
Aneurysm
Blood vessel disorders cont’d
Varicose veinsirregular dilations in superficial veins, especially of the legs; associated with prolonged increased back pressure, also with crossing legs.
Blood vessel disorders cont’d
Hypertension – high b.p.; caused by kidney disease, high
Na + intake, obesity, stress, arteriosclerosis; left ventricle works overtime so myocardium thickens, enlarging heart coronary vessels can’t feed overgrowth so parts of heart die
Disorders, cont.
Anemia – condition in which the oxygen carrying capacity of the blood is reduced ; symptoms: fatigue, intolerance to cold, and paleness.
– Nutritional Anemia – inadequate diet, especially lacking in iron and vitamin
B12
– Sickle-Cell Anemia – abnormal kind of hemoglobin results in cells shaped like a sickle (bent); they can rupture easily and often get stuck together; (genetic)
Types of Anemia
Pericarditis
Inflammation of the pericardium and therefore an enlargement of the pericardial sac.
This causes an increase in pressure on the outside of the heart and causes the heart to have to work harder
Can cause heart attack
Treatment – typically the fluid is drained with a needle into the pericardial sac.
Pericarditis
1.
2.
Blood
Connective tissue with liquid matrix.
Carries oxygen, protects against infection, promotes clotting, and carries other vital substances
Plasma
clear, straw-colored (yellowish)
mixture of water (95%), amino acids, proteins, carbs, lipids, vitamins, hormones, electrolytes, and cellular wastes
Red Blood Cells (Erythrocytes)
contain hemoglobin (a protein that carries oxygen) made of Iron – loves oxygen – what causes blood to change colors. Red to purplish
Also the chemical when changed which causes urine to be yellow and feces to be brown.
formation of RBC (hematopoiesis) – in red marrow
Blood continued
3. White Blood Cells (Leukocytes)
Can squeeze through vessel walls and move through interstitial spaces via amoeboid movement
Many kinds of white blood cells; all have different jobs.
Protect against disease in 2 ways:
– Phagocytize bacteria (eat up bacteria like pacaman)
– Produce antibodies (proteins that destroy or disable foreign particles)
4. Platelets (Thrombocytes)
Cell fragments that help close breaks in vessels and initiate formation of blood clots - (coagulation)
Causes scabs and stops bleeding.
5 Types of
White Blood
Cells
Red Blood
Cells are erythrocytes
ABO Blood Types
Antigen- protein or carb on RBC surface
–Presence or absence of antigens is an inherited trait
2 major antigens: Antigen A and
Antigen B
4 possible antigen combinations: A only, B only, A and B, or neither A nor
B
ABO Blood Types
Antibodies- proteins in the plasma that destroy foreign substances
Antibodies develop about 2-8 months after birth
– If antigen A is absent – a person develops anti-A antibody
– If antigen B is absent – a person develops anti-B antibody
ABO Blood Types, cont
Blood Type
A
B
AB
O
Antigen
A
B
A and B
Antibody
Anti-B
Anti-A
Neither Anti-A nor Anti-B
ABO Blood Types, cont.
An antigen and an antibody of the same type react to clump RBC – so such combos must be avoided
Type AB – universal recipients (lacks antibodies anti-A and anti-B)
Type O – universal donors (lacks antigens
A and B)
However, the preferred donor is one with the matching blood type
Rh Blood Type
Blood type – a person is either positive or negative.
It takes only 1 gene to be positive. erythroblastosis fetalis – When a mother is RH – and her baby is RH +.
During their first pregnancy some blood is transferred from baby to mother. The mother then develops antibodies against
RH+ blood.
erythroblastosis fetalis
Next pregnancy some of the blood from the mom gets in the baby and the antibodies cause the blood to agglutinate.
Can cause fatality because of lack of oxygen (severe anemia)
Treated by massive transfusions of Rh+ blood for the baby and removal of blood containing Rh+ antibodies.