Adult Echocardiography. Lecture 3 Cardiac
advertisement

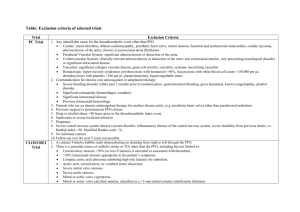
Adult Echocardiography Lecture Three Cardiac Physiology Harry H. Holdorf Electrophysiology • Normal Electrical Activation – SA node (Special Neuromyocardial Cells-pacemaker – AV node (electrical impulse pauses to prevent simultaneous contraction of the atria and ventricles – Bundle of His – Bundle branches (right and left) – Purkinje fibers • HINT: which is the fastest intrinsic rate? SA NODE Action Potential • What is the absolute refractory state? – That period when a muscle cell is not excitable • From phase one until into phase 3 • The relative refractory period is during phase 3 and the muscle cell might contract if the stimulus is strong. • See next slide for chart. Electro-cardiogram • Normal complex – P wave-atrial systole – P-R interval – includes P-R segment (from atrial to ventricular depolarization) – T wave – ventricular diastole (repolarization) – HINT: Know what P wave, PR interval, and T wave represent 1 small box = 0.04 seconds 1 big box = 0.2 seconds 5 big boxes = 1 second • What is the normal duration for the QRS complex? – 0.10 seconds – Normal values • R-R interval = 3 to 5 big boxes (60-100 beats/minute • QRS complex = less than 3 little boxes (less than 0.12 seconds) • PR interval = Less than 1 big box (less than 0.2 seconds) Mechanical Events • Frank-Starling Law (Length – Tension Relationship) – Increased volume (preload) = increased contractility (to a physiologic limit). – Increased myocardial fiber length = increased tension (rubber band theory) Know Frank-Starling Law As the ventricles become overfilled (to the right on the curve beyond EDV = ~250 mL), the heart becomes inefficient and stroke volume levels off. • Acute AI is hyper-contractile because we shift up the Starling curve. • Chronic AI is failure when we drop off the end. PRELOAD Load (volume) exerted on the ventricle at END DIASTOLE. Determines force of contraction. The greater the load the greater the force of contraction (Frank-Starling Law). PRELOAD cont… • Increased preload: Mitral regurgitation Tricuspid regurgitation Pulmonic regurgitation Aortic regurgitation Ventricular and atrial septal defects Fluid Overload HINT: Echo findings for Preload vs. afterload: Preload = dilatation Afterload = hypertrophy Afterload • Resistance against which the ventricle must pump. • Determines the tension the myocardium must generate. • INCREASE AFTERLOAD – Hypertension – Aortic Stenosis – Pulmonic stenosis Which test does not allow for the calculation of ejection fraction? A. 2D echo B. Cardiac angio C. Chest X-ray D. Cardiac Nuclear study LV Function Indicators • Stroke Volume (SV) SV = end diastolic volume (EDV) – end systolic volume (ESV) Normal varies with end diastolic volume, heart rate, size (normal: 70110 ml). Ejection Fraction (EF) EF = SV/EDV x 100 Normal is > 55% Cardiac Output (CO) CO = SV x heart rate (HR) Normal is 4-8 L/min Calculate CO from SV and HR Bernoulli Equation Aliasing • Occurs when the Doppler shift exceed the Nyquist Limit • Nyquist Limit = ½ of the PRF (Pulse Repetition Frequency) • A problem with higher velocities in pulsed Doppler (spectral & Color flow) • Occurs sooner with higher frequency transducers NOTE: How does switching to a lower frequency transducer affect aliasing? Aliasing will occur at higher velocities Doppler Stroke Volume SV = VTI (FVI) x CSA – VTI is the velocity time integral as calculated by tracing the Doppler spectral display (sometimes called the “flow velocity integral or FI”). It represents how far the blood travels in centimeters with each ejection. Normally, 12 cm for the mitral valve and 20 cm for the aortic valve. Doppler signal in the left ventricular outflow tract: Velocity Time Integral (VTI) • CSA is the cross-sectional area • NOTE: What does VTI x CSA equal? – Doppler stroke volume Maneuvers Altering Cardiac Physiology SV, CO, IHSS, AS, MR, HR, BP, AR • Breathing: – Inspiration: Increases venous return – Expiration: Decreases venous return • Standing – Decreases venous return, SV • Squatting – Increases venous return, SV and CO. (Increases AR, Decreases IHSS) • Handgrip – Increases HR, CO, arterial pressure. (Decreases AS, increases MR) • Valsalva – 2 main phases-strain and release. – During strain-decreases venous return, SV and CO – Most murmurs decrease during straining, IHSS increases – During release-increase venous return, CO, and BP • Sit-ups – Increases HR, CO and SV • Amyl nitrate inhalation: Vasodilator-decreases peripheral resistance- increases HR, CO, and SV (increases forward murmurs, decreases AR/MR. NOTE: Does venous return increase or decrease with inspiration? Increases • Inhalation of amyl nitrite causes: – Decreased afterload Vasodilator drops BP Tachycardia response • Increases stroke volume • Increases heart rate • Mitral valve velocity during inspiration: – decreases A Wiggers diagram is a standard diagram used in cardiac physiology named after Dr. Carl J. Wiggers. • • • • • • • The X axis is used to plot time, while the Y axis contains all of the following on a single grid: Blood pressure – Aortic pressure – Ventricular pressure – Atrial pressure Ventricular volume Electrocardiogram Arterial flow Heart sounds By illustrating the coordinated variation of these values, it becomes easier to illustrate the relationship between these values in the cardiac cycle. Cardiac Cycle (Wiggers Diagram) b. Mitral valve closure C. Aortic valve opens e. Aortic valve closure f. Mitral valve opens • Know isovolumetric timing with the ECG – After R wave = isovolumic contraction – After T wave = isovolumic relaxation • Know the duration of IVRT and IVCT – 70 msec • The duration of isovolumetric relaxation time will be increased with: – Bradycardia • Between which heart sounds will the murmur of aortic stenosis be heard? – S1 –S2 • During the cardiac cycle, this event NEVER happens: – Ao valve is open & mitral valve is open – Both are closed during ISO-V The truth about the cardiac cycle 1. Normal arterial pressure is approx. 120/80 mmHg. Thus, the aortic pressure lives high 2. Normal left arterial pressure is approximately 10 mmHg. Thus, the atrial pressure lives low. 3. The left ventricular pressure bounces between aortic and atrial. High and low. 4. The valve that lives between the left ventricle and the aorta is the aortic valve. The aortic valve lives high. 5. The valve that lives between the atrium and the left ventricle is the mitral valve. The mitral valve lives low. 6. The magic word is “COCO’. Close, open, close, open. 7. When a normal valve is open, there is very little pressure difference between the chambers on either side of the valve. So, when the aortic valve is open, the LV and aortic pressures are nearly identical. When the mitral valve is open ,the atrial and LV pressures are nearly identical. HEMODYNAMICS • Pulmonary – Low pressure – Low resistance – RV wall is thin – Low O2 content in artery • Systemic – High pressure – High resistance – LV wall is thick – High O2 content in artery Hemodynamics continued Components • Pulmonary – Pulmonary artery – Arteries – Capillaries – Veins • Systemic – Aorta – Arteries – Arterioles – Veinules – Veins – Vena Cava • Arteries – Elastic, thick walled blood vessels – Expand during systole, then recoil during diastole to keep blood moving forward • Veins – Thin walled blood vessels that collapse easily – Able to expand rapidly to accommodate large volumes of blood – Contain the majority of circulating blood Blood • 54% of blood volume is plasma • 45% of blood volume is red blood cells (erythrocytes) • 1% of blood volume is white blood cells (leukocytes) and platelets (thrombocytes) Normal pressures More normal pressure ranges • • • • • • • RA = 8/5 Ao = 120/80 PA = 25/10 RV= 25/0 LV = 120/0/12 LA = 10/12 PCW = 10 Normal atrial pressures are about 6 mm Hg in the right atrium and 10 mm Hg in the left atrium. Other than that, the right – sided pressures are approx. 1/5th of the left sided pressures. • Think Tank: – What are normal pressures in the pulmonary artery? • 25/10 Normal O2 Saturations • Oxygenated blood, 95% saturated (pink blood) starts in the pulmonary veins and continues to the end of the systemic arteries. • Deoxygenated blood, 75% saturated (blue blood) starts in the systemic veins and continues to the pulmonary arteries. • Where is the O2 saturation the lowest? – Coronary sinus • Know O2 saturation in pulmonary veins is 95% and Pulmonary arteries is 75% Cardiac Catheterization • Angiography – Contrast medium injected while cineangiography film records results (vessel narrowing, regurgitation, shunts, ejection fraction). – LV angiogram also called ventriculography, selective angiography, or angiocardiography. • NOTE: Best cath technique for LV function? – LV angiogram Cardiac Output • Fick method measures O2 consumption divided by the difference in O2 content between arterial and pulmonary system. • Angiography technique multiples the stroke volume by the heart rate. • Oximetry – Measures O2 saturation in various chambers (able to detect shunts by changes in O2 saturation). – Shunt size is calculated by the difference between pulmonary and systemic blood flow. Cath Gradients • Pressure waveforms for Aortic Stenosis, Mitral Stenosis, Mitral regurgitation • What is PWC (Pulmonary Capillary Wedge) measuring? – Left atrial pressure SEP = Systolic Ejection Period DFP = Diastolic Filling Period PCW = Pulmonary Capillary Wedge (from a Swan-Ganz Catheter Aortic Stenosis • To determine AS, where are catheters placed? • One in the LV and one in the Ao or one in the LV and Pulled Back across the AoV or one catheter with two separate sensors. • See LV and Ao tracings. • The aortic valve lives between the LV and Ao. • If LV pressure is higher than Ao pressure in systole (they should track together), this is Aortic Stenosis. End Lecture Three NEXT LECTURE TECHNIQUE & PATIENT CARE