ARDS - WordPress.com
advertisement

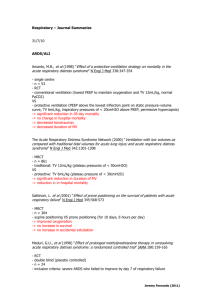
ARDS ARDS A specific Clinical Syndrome that causes respiratory failure Characterized by the acute onset of diffuse bilateral pulmonary infiltrates and severe hypoxemia without LV failure as the cause ARDS Definition Standardized definition developed in 1992 by the American-European Consensus Conference (AECC). Acute Bilateral Pulmonary Infiltrates PaO2 to FiO2 Ratio of less than 200. Pulmonary Artery Wedge Pressure less than 18 mmHg 3. Bernard GR, Artigas A, Brigham, Carlet J; et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994;149:81824. ARDS- Definition Modifiers Pulmonary artery wedge pressures-not routinely done in all patients. Definition has been modified to allow for any means of ruling out LV failure as the cause Acute Lung Injury (ALI) refers to the same clinical syndrome but with PaO2/FiO2 ratio between 201-300 Primarily a matter of semantics as the difference in these gas exchange deficits does not reliably predict the degree of underlying pathology. There is also no difference in mortality between the two groups Bernard GR, Artigas A, Brigham, Carlet J; et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994;149:818-24 ARDS Affects about 200,000 people per year in the United States alone Hospital Mortality rate is 41% Most patients tend to die from multi-organ failure as opposed to the lung disease itself. Our understanding of this disease over the last 40 years has increased dramatically with mortality rates significantly reduced from initial estimates of 70%. 5. Rubenfeld GD, Caldwell E, Peabody E, Weaver J. et al. Incidence and Outcomes of Acute Lung Injury. N Engl J Med 353:1685-93 6. Esteban, A, Anzueto, A, Frutos, F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 2002; 287:345. ARDS: A Clinical Syndrome Common endpoint of many different processes Sepsis is the most common cause Can be seen with trauma, pancreatitis, aspiration, certain medications, oxygen toxicity and the effects mechanical ventilation itself Most commonly the inciting injury begins in the lungs as with aspiration or PNA, but may result from an inflammatory reaction from any part of the body ARDS Imaging Radiographic imaging is an integral part of the diagnosis of ARDS Classic CXR is one of bilateral infiltrates, often with air bronchograms Main concern is to distinguish these infiltrates from those of other causes such as cardiogenic pulmonary edema ARDS Imaging- Typical CXR ARDS Imaging CT scan imaging has been used to better characterize the disease since the 1980s The fact that it is a very non homogeneous process became much more obvious with this imaging The dependent portions of the lung, usually the lower and posterior areas are generally more severely involved This coincides with the areas of the lungs that receive the greatest blood supply 7. Rommelsheim K, Lackner K, Westhofen P et al. [Respiratory distress syndrome of the adult in the computer tomograph] Anasth Intensivther Notfallmed. 1983 Apr;18(2):59-64. German. 9. Maunder RJ, Shuman WP, McHugh JW et al. Preservation of normal lung regions in the adult respiratory distress syndrome. Analysis by computed tomography. JAMA. 1986 May 9;255(18):2463-5. ARDS- Typical CT ARDS Pathophysiology ARDS results from an inflammatory injury to the alveoli and vasculature Lungs are particularly vulnerable as they receive 100% of the cardiac output, and thus filter any inflammatory cytokines that are released into the circulation Prominent proiinflammatory cytokines are: TNF-α, IL-6, and IL-8 14. Martin, TR. Lung cytokines and ARDS: Roger S. Mitchell Lecture. Chest 1999; 116:2S. 15. Colletti LM, Remick DG, Burtch GD, et al. Role of tumor necrosis factor-alpha in the pathophysiologic alterations after hepatic ischemia/reperfusion injury in the rat. J Clin Invest 1990; 85:1936 ARDS Pathophysiology The presence of these cytokines (TNF-α, IL-6, and IL-8) causes neutrophil recruitment to the lung, where they are then activated These activated neutrophils produce more inflammatory cytokines and proteases which ultimately damage the endothelial capillaries and alveoli This produces significant edema and further inflammation- creating a vicious inflammatory cycle 16. Windsor, AC, Mullen, PG, Fowler, AA, et al. Role of the neutrophil in adult respiratory distress syndrome. Br J Surg 1993; 80:10. 17. Hogg, JC. Felix Fleischner Lecture. The traffic of polymorphonuclear leukocytes through pulmonary microvessels in health and disease. AJR Am J Roentgenol 1994; 163:769. Pathological Phases The three sequential phases of ARDS pathology are: exudative, proliferative and then the fibrotic phase Exudative phase occurs over the first 2-7 days Characterized by pulmonary edema, and the formation of hyaline membrane (staining PASpositive). Hyaline membranes are composed of fibrin and cellular debris formed from the destruction of Type 1 pneumocytes Pathology described as DAD or diffuse alveolar damage 19. Ware LB, Matthay MA The acute respiratory distress syndrome. N Engl J Med 2000;342:1334. ARDS Pathological Phases Proliferative Phase usually seen during day 7 to 14 Driven by the ongoing inflammation as well as the damaging effects of mechanical ventilation, oxygen toxicity and physical barotrauma Characterized by the repair and remodeling of the injured lung cells with proliferation of Type II alveolar cells Fibroblasts also begin to proliferate This lays the groundwork for the ensuing fibrotic phase 20. Tomashefski JF Jr. Pulmonary pathology of acute respiratory distress syndrome. Clin Chest Med. 2000;21(3):435-66. 21. Meyrick B. Pathology of the adult respiratory distress syndrome. Crit Care Clin. 1986;2(3):405-28. 22. Ingbar DH. Mechanisms of repair and remodeling following acute lung injury.Clin Chest Med. 2000;21(3):589-616. ARDS Pathological Phases Fibrotic phase generally develops around day 14 Deposition of proteoglycans and collagen can be seen Fibroblasts now extensively proliferate and incorporate the hyaline membranes This leaves a fibrotic, acellular connective tissue skeleton Traction bronchiectasis may develop and small cystic areas can often be seen 20. Tomashefski JF Jr. Pulmonary pathology of acute respiratory distress syndrome. Clin Chest Med. 2000;21(3):435-66. 21. Meyrick B. Pathology of the adult respiratory distress syndrome. Crit Care Clin. 1986;2(3):405-28. 22. Ingbar DH. Mechanisms of repair and remodeling following acute lung injury.Clin Chest Med. 2000;21(3):589-616. ARDS Pathological Phases Mechanical Ventilation Most patients with ARDS require mechanical ventilation Necessary for survival, but also contributes to the lung disease itselfventilator induced lung injury (VILI) VILI can be subclassified into two broad categories- macrobarotrauma and microbaroutrauma VILI Macrobarotrauma refers to injuries such as pneumothorax, pneumomediastinum or any form of air leak These types of injuries are relatively uncommon with conventional ventilator management Microbarotrauma refers to injuries to the smaller airways and alveoli themselves. Microbarotrauma is felt to play a much larger role in the pathogenesis of ARDS 29. Eisner MD, Thompson T, Hudson LD, et al. Efficacy of low tidal volume ventilation in patients with different clinical risk factors for acute lung injury and the acute respiratory distress syndrome. Am J Respir Crit Care Med. 2001;164(2):231-6 30. Brower RG, Lanken PN, MacIntyre N et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004 Jul 22;351(4):327-36. VILI- How the lungs are damaged VILI occurs in three basic ways: Volutrauma, biotrauma and atelectrauma Volutrauma refers to injury due to insufflating large volumes of air during PPV This damages the alveoli walls by increasing the amount of stretch and tensile force on the alveoli This causes direct damage to the alveoli but also induces an inflammatory reaction perpetuating the ongoing injury Mechanical Ventilation in ARDS Low tidal volume strategy became the standard of care after the ARDSNet investigators completed a large randomized control trial Here they enrolled 861 patients with ARDS and randomized them to either 12cc/kg tidal volume vs 6cc/kg. Trial was stopped early due to a significant reduction in mortality from 40% to 31% as well as a decrease in days on the ventilator 44. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8. Mechanical Ventilation in ARDS The standard approach is now to start with a TV of 6cc/kg, and to follow peak and plateau pressures on the ventilator Adjustments can then be made with increases or decreases in the tidal volume with a goal of keeping the plateau pressures less than 30cm H2O Permissive hypercapnea, (accepting a respiratory acidosis) is frequently required. PEEP Several studies have shown that using higher levels of PEEP improve oxygenation Varying levels of PEEP however have not been shown to impact on survival The ARDSNet investigators addressed this in a study called ALVEOLI ALVEOLI Study A follow up study to compare high PEEP vs. low PEEP Used low TV strategy in all patients Higher PEEP group had better oxygenation, increased PaO2/FiO2 ratios, and improved lung compliance Clinical outcomes of the two groups were same and mortality was not affected 45. Brower RG, Lanken PN, MacIntyre N, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351(4):327-36. ARDSNet standard PEEP guide Practical PEEP Balance between PEEP’s beneficial effects and deleterious side effects Barotrauma Increased complication risk with procedures ie. central lines Increased intrathoracic pressure- causes decrease preload and decreased cardiac output Ultimately decreased renal blood flow, stimulating RAS adding to more fluid retention and edema Increased intracranial pressures Recruitment Maneuvers Usually entails giving a ventilated patient a sustained level of high PEEP 30-40 cm H2O for 30 to 40 seconds Some evidence of sustained improved oxygenation in animal models Response in humans is unreliable ARDSNet addressed this on the first 80 enrolled patients in the ALVEOLI study, as well as in a separate clinical trial Both studies found only transient rises in oxygenation which quickly return to baseline 46. Rimensberger PC, Cox PN, Frndova H, et al. The open lung during small tidal volume ventilation: Concepts of recruitment and “optimal” positive end-expiratory pressure. Crit Care Med 1999; 27: 1946–1952 47. Verbrugge S, Lachman B. Mechanisms of ventilation-induced lung injury and its prevention: Role of surfactant. Appl Cardiopulm Pathophysiol 1998; 7: 173–198 48. Brower RG, Morris A, MacIntyre N, et al. Effects of recruitment maneuvers in patients with acute lung injury and acute respiratory distress syndrome ventilated with high positive end-expiratory pressure. Crit Care Med. 2003;31(11):2592-7. Prone Position First used in the 1970s with two case series published Demonstrated improved oxygenation in most, but not all patients Takes advantage of the heterogeneity of ARDS, and that the oxygen deficit is secondary to the amount of consolidated and collapsed lung not being inflated Majority of non-inflated lung is at the dependent areas- typically posterior lung bases 50. Douglas WW, Rehder K, Beynen FM, et al. Improved oxygenation in patients with acute respiratory failure: The prone position. Am Rev Respir Dis 1977; 115:559. 51. Piehl MA, Brown RS. Use of extreme position changes in acute respiratory failure. Crit Care Med 1976; 4:13. Prone Position By placing a patient in the prone position perfusion is increased to the dorsal areas of the lung which are generally less affected. Improves ventilation/perfusion ratio Reduces shunt fraction Improves oxygenation Oxygen improvement may also be secondary to decreasing pleural pressures in the dependent portions of the lung and decreasing the amount of lung compressed by the weight of the heart 52. Albert RK, Hubmayr RD. The prone position eliminates compression of the lungs by the heart. Am J Respir Crit Care Med 2000;161:1660-5 Prone Position Some studies demonstrate sustained improvement in the oxygenation with using the prone position No documented mortality benefit Associated morbidity with complications of repositioning Pressure sores, selective intubation, ETT obstruction, catheter removals, facial edema Labor intensive CPR problematic 53. Vollman KM, Bander JJ. Improved oxygenation utilizing a prone positioner in patients with acute respiratory distress syndrome. Intensive Care Med 1996; 22:1105. 54. Curley MA. Prone positioning of patients with acute respiratory distress syndrome: a systematic review. Am J Crit Care 1999; 8:397. 55. Fridrich P, Krafft P, Hochleuthner H, Mauritz W. The effects of long-term prone positioning in patients with trauma-induced Prone Position General Suggestions Select patients properly Newer commercial beds make this somewhat easier Recent abdominal/thoracic surgery considerations- towel rolls, inner tubes, abdominal binders Spinal instability- contraindication Volume Status Increasing data also now favors a conservative fluid management strategy Simmons- retrospective 113 pts. Survivors have lower fluid balance Humphrey- Improved survival seen in patients with decreased wedge pressures Ferguson- Persistently elevated PAOP was predictor of mortality 65. Simmons RS, Berdine GG, Seidenfeld JJ, et al. Fluid balance and the adult respiratory distress syndrome. Am Rev Respir Dis 1987;135:924-929. 66. Humphrey H, Hall J, Sznajder I, et al. Improved survival in ARDS patients associated with a reduction in pulmonary capillary wedge pressure. Chest 1990;97:1176-1180. 68. Ferguson ND, Meade MO, Hallett DC, et al. High values of the pulmonary artery wedge pressure in patients with acute lung injury and acute respiratory distress syndrome. Intensive Care Med 2002;28:1073-1077. Volume Status/ PA catheters PA Catheters less frequently used, and not necessary in most patients Early studies demonstrated conflicting evidence regarding benefit FACTT trial performed by ARDSNet investigators 1001 patients randomized to a fluid management strategy using PAC vs CVC. FACTT trial demonstrated no difference in primary outcomes of mortality or organ function between the two groups- but PAC group had a higher complication rate 66. Humphrey H, Hall J, Sznajder I, et al. Improved survival in ARDS patients associated with a reduction in pulmonary capillary wedge pressure. Chest 1990;97:1176-1180. 67. Marinelli WA, Weinert CR, Gross CR, et al. Right heart catheterization in acute lung injury: an observational study. Am J Respir Crit Care Med 1999;160:69-76.74. The Acute Respiratory Distress Syndrome Network. 74. Pulmonary artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med 2006;354;22132224. Volume Status ARDSNet investigators using same patient data as FACTT trial performed a large randomized control trial comparing a conservative vs. a liberal fluid management strategy. 1001 patients enrolled Primary endpoint: Mortality. Secondary Endpoints: ventilator free days, organ dysfunction, lung function No difference in 60 day mortality Conservative management group had significantly less ventilator days, and improved pulmonary function, without affecting organ dysfunction 75. The Acute Respiratory Distress Syndrome Network. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 2006;354:2564-75. Pharmacologic Treatments: Steroids The use of steroids in ARDS has been controversial and dates back to the 1970s and early eighties when their use was fairly routine In the mid eighties data began to emerge regarding increased infection rates associated with their use There has been significant conflicting data since then Steroids Meduri et al (1991) used steroids in a small series of patients to treat pulmonary fibrosis secondary to ARDS in the late, fibrotic phase They demonstrated improved gas exchange and lower mortality rates in this population These results were unable to be repeated 79. Meduri GU, Belenchia JM, Estes RJ, et al. Fibroproliferative phase of ARDS. Clinical findings and effects of corticosteroids. Chest 1991;100:943-52. Steroids Meduri et al then studied a prolonged course of steroids (32 days) in ARDS using a RCT. They gave methylprednisolone 2mg/kg per day, and performed extensive infection surveys They were able to demonstrate a decrease in mortality as well as improvement in lung injury and MODS scores. Small study with 24 patients Meduri GU, Headley AS, Golden E, et al. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA 1998;280:159-165 Steroids ARDSNet investigators studied 180 patients with ARDS of at least seven days duration termed “persistent ARDS” Steroids were administered in a similar manner to Meduri et al but with a more rapid taper Primary outcome was 60 day mortality No mortality benefit was shown 80. Steinberg KP, Hudson LD, Goodman RB, et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med 2006;354:1671-84. Steroids: Clinical Guidelines May be useful in select cases If use, consider infectious risks Intensive infection surveillance may be necessary as was done in the Meduri trial. This may include bronchoscopy with BAL to watch closely for development of pneumonia in these susceptible patients Other Pharmacologic Treatments Antioxidants Surfactant No clear benefits shown Alternate Ventilator Strategies HFOV- High frequency Oscillatory ventilation IRV- Inverse ratio ventilation APRV-Airway pressure release ventilation Overall few clinical trials and no mortality benefits have been shown Further studies ongoing