Ativity 27, 28 - PCC - Portland Community College
advertisement

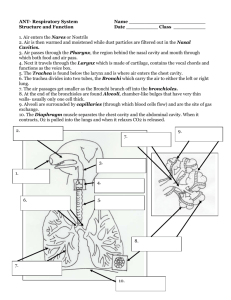
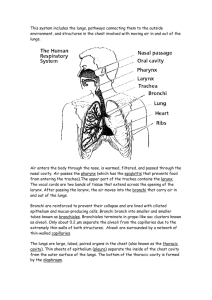
Lab Exercise 24 Anatomy of the Respiratory System Portland Community College BI 233 1 Upper & Lower Respiratory System Upper Respiratory System Nose Nasal cavity Paranasal sinuses Pharynx 2 Respiratory system Lower Respiratory System Larynx Trachea Bronchi Lungs 3 Nasal bones • Frontal and nasal bones for the nasal bridge and processes of the maxillae make up the lateral walls. • Nasal septum divides the nasal cavity into right and left halves formed by vomer and perpendicular plate of the ethmoid 4 Uvula • During swallowing, the soft palate elevates and the uvula closes off the internal nares, preventing food or fluids from entering the nasal cavity. 5 Nasal Cavity 6 Nasal Cavity Opening of Auditory Tube Superior Middle & Inferior Turbinates External Nares 7 Nasal Cavity The nasal epithelium covering the conchae serves to cleanse, warm and humidify the air • Nasal conchae increase the surface areas for the mucus epithelium The olfactory epithelium in the upper medial part of the nasal cavity is involved in the sense of smell. The nasal cavity serves as a resonating chamber as well as an avenue for escaping air. 8 Nasal Turbinates or Conchae • Ciliated pseudostratified columnar epithelium with . goblet cells pushes trapped dust toward the back of the throat to be swallowed. 9 10 Sinuses All the sinuses are continuous with the nasal cavity are lined by mucous membrane. Mucous secretions drain into the nasal cavities. 11 Pharynx • Connects the nasal and oral cavities to the larynx and esophagus • Anatomically divided into 3 sections: • Nasopharynx • Oropharynx • Laryngopharynx 12 (pseudostratified epithelium) (stratified squamous epithelium) (stratified squamous epithelium) 13 Tonsils Pharyngeal Tonsils (Adenoids) Palatine Tonsils Lingual Tonsils 14 Tonsils Pharyngeal tonsils • Tonsils: lymphoid tissue. Palatine tonsils 15 Larynx: aka Voice Box • Made of 9 pieces of cartilage, the most important are: • Thyroid cartilage (Adam’s Apple) • Thyrohyoid membrane • Cricoid Cartilage • Cricothroid ligament • Epiglottis 16 Hyoid Bone Larynx Epiglottis Thyrohyoid Membrane Thyroid Cartilage Cricoid Cartilage Cricothyroid Ligament Tracheal Cartilage 17 Inside the Larynx • Vestibular Folds: • Also called false vocal cords, ventricular band of larynx, ventricular folds, and upper folds • Vocal Cords, or vocal folds • Lower, “true” vocal cords • Attach to the arytenoid cartilages by the vocal ligaments (internal) • Glottis: The vocal cords and the space (rima glottidis) between them. 18 Inside the Larynx 19 Inside the Larynx Rima Glottis True Vocal Cords Corniculate cartilage Cuneiform cartilage Glottis Epiglottis Tongue 20 Glottis: True cords plus opening Rima Glottis: The opening 21 Larynx Airways Trachea The carina is the last cartilage which separates the entrances to the left and right primary bronchi Right Mainstem Bronchi Left Mainstem Bronchi Secondary Bronchi Carina Secondary Bronchi 22 Bronchi • The carina of the last tracheal cartilage marks the end of the trachea and the beginning of the right and left bronchi • Left main stem bronchus • Right main stem bronchus • Bronchi subdivide into secondary bronchi, each supplying a lobe of the lungs 23 Respiratory Tree 24 Branching of Bronchial Tree Trachea Primary Bronchi Secondary Bronchi Tertiary Bronchi Bronchioles Terminal/Respiratory Bronchioles 25 Lungs • • • • Apex: the part under the clavicle Base: the part touching the diaphragm Costal Surface: the part touching the ribs Hilus: indentation containing pulmonary and systemic blood vessels • Left Lung has 2 lobes and a cardiac notch • Left upper lobe • Left lower lobe • Right Lung has 3 lobes • Right upper lobe, middle lobe, lower lobe 26 Apex Lungs LUL RUL Hilus RML LLL RLL Base 27 Lungs: Medial View 28 Lung Lobes 29 Pleura • Pleura is the double-layered sac of serous membrane • Parietal Pleura is the outer layer and is attached to the thoracic walls • Visceral Pleura is the inner layer covering the lung tissue • The layers are only touching, they are not fused together • The potential space is called the pleural cavity • There is serous fluid between the layers which allows them to slide against each other during breathing 30 Pleural cavity is in between the two layers 31 Mediastinum • The area between the lungs. • Posterior to the sternum • Anterior to the vertebrae • Contains the heart, great vessels, esophagus and thymus 32 Trachea Histology • Composed of three layers • Mucosa: made up of goblet cells and ciliated pseudostratified columnar epithelium • Submucosa: connective tissue deep to the mucosa • Adventitia: outermost layer, has C-shaped rings of hyaline cartilage 33 Trachea 34 Trachea Histology 35 Trachea Histology 36 Seromucous Glands (Trachea) 37 Trachea Pseudostratified Columnar Epithelium Submucosa with seromucous glands Hyaline Cartilage 38 Bronchi Bronchioles • Tissue walls of bronchi mimic that of the trachea • As conducting tubes become smaller, structural changes occur and eventually they become bronchioles • Cartilage support structures change • Bronchioles differ from bronchi in that they lack cartilage • Epithelium types change • Amount of smooth muscle increases 39 Bronchi Histology 40 Bronchioles Respiratory Bronchioles • Respiratory Bronchioles : Continued branching leads to the area where gas exchange occurs by simple diffusion 41 Bronchiole Histology Notice the lack of cartilage Simple columnar epithelium 42 Respiratory Bronchioles Alveolar Ducts Alveolar sacs 43 Alveolar sacs Alveoli • Alveolar sacs look like clusters of grapes • The “individual grapes” are Alveoli 44 Alveoli Histology 45 Type II Pneumocytes are cuboidal and produce surfactant Type 1 Pneumocytes are flattened for gas exchange 46 47 Respiratory Membrane • The area where gas exchange between air and blood occurs • It is the fused alveolar and capillary walls (3 layers) 1. Squamous type 1 alveolar epithelium 2. Fused basal laminae 3. Squamous endothelial cells in pulmonary capillaries 48 Respiratory Membrane 49 Lab Exercise 25 Respiratory System Physiology 50 Terminology Pulmonary Ventilation: aka breathing, is the movement of air into and out of the lungs External Respiration: The gas exchange between the blood and alveoli (Partial pressure of oxygen in the alveoli is greater than in the blood) Transport of gases: which is how oxygen and carbon dioxide are carried by the blood between the lungs and all tissues Internal Respiration: Exchange of gases between systemic blood and tissue cells (pressures are opposite from external respiration) 51 Dalton’s law • The total pressure of a gas mixture is equal to the partial pressures of all the individual gases in the compound • During respiration, oxygen and carbon dioxide will move along a pressure gradient from high conc. To low conc. 52 Gas Exchange • Almost all oxygen (98%) is transported by binding to hemoglobin in RBCs. • The remainder simply dissolves in the blood plasma. • Most carbon dioxide (68% to 78%) diffuses into RBCs where it is converted to carbonic acid (H2CO3) • Carbonic acid quickly dissociates into bicarbonate ions and hydrogen ions 53 Acid Base Balance in Blood • In the RBC and minimally in the plasma, this reaction takes place • CO2 + H2O H2CO3 HCO3- + H+ • The bicarbonate ions (HCO3- ) help buffer the blood by combining with extra H+ in the blood. • Carbonic acid (H2CO3) releases H+ when the blood becomes too basic. • This way, the balance of H+ remains steady and the pH is doesn’t fluctuate. 54 Carbonic Acid Buffer System: Dealing with Acids • CO2 + H2O H2CO3 HCO3- + H+ (Add an acid) + H+ • The H+ will combine with HCO3- to create H2CO3 • H2CO3 will then dissociate into CO2 + H2O • Breathing will increase to rid the body of the extra CO2 55 Carbonic Acid Buffer System: Dealing with Bases • CO2 + H2O H2CO3 HCO3- + H+ (Add a base) + OH• The OH- will combine with H+ to create H2O • H2CO3 will dissociate into HCO3- + H+ to restore the H+ concentration 56 57 Boyle’s Law • The pressure of a gas is inversely proportional to its volume. • If the volume of the thoracic cavity increases, the air pressure in the airways decreases This results in a pressure gradient that forms between the atmosphere (high) and the air ways (low) forces air to move into the lungs 58 Pulmonary Ventilation • During inspiration, the ribs are elevated and the sternum moves outward. • During expiration, the ribs are depressed and the sternum moves inward. • The diaphragm is the primary inspiratory muscle 59 Inspiration/Expiration • Inspiration: Increase in thoracic cavity size • Inspiratory muscles • External intercostals (lift the rib cage) • Diaphragm (Becomes flat) • Expiration :Decrease in thoracic cavity size • Expiratory muscles • For the most part it is just the relaxation of the inspiratory muscles (passive process) • Internal intercostals & abdominal muscles used only for forced expiration 60 Muscles of Respiration 61 Muscles: Inspiration 62 Muscles: Expiration 63 Spirometry • Diagnostic technique used to measure respiratory volumes • The instrument used is a spirometer. • It cannot measure the amount of air in the lung, only the amount entering or leaving. 64 Respiratory Volumes • Tidal Volume TV • Volume of air moved in or out of the lungs during quiet breathing about 500 mL. • Inspiratory Reserve Volume IRV • Volume that can be inhaled during forced breathing in addition to tidal volume 3100mL. • Expiratory Reserve Volume ERV • Volume that can be exhaled during forced breathing after a normal tidal volume 1200 mL. 65 Respiratory Volumes • Residual Volume RV * Can not be measured using spirometry* • Volume that remains in the lungs at all times 1200 mL. • The sum of two or more of these volumes is known as a pulmonary capacity. The five pulmonary capacities are as follows: 66 Respiratory Capacity • Vital Capacity VC • Maximum volume that can be exhaled after taking the deepest breath possible VC = TV + IRV + ERV • Inspiratory Capacity IC • Maximum volume that can be inhaled after a normal exhalation IC = TV + IRV 67 Respiratory Capacity • Functional Residual Capacity FRC • The amount of air left in the lungs after a normal exhalation FRC = ERV + RV • Total Lung Capacity TLC * can not be measured using spirometry* • Total volume of air that the lungs can hold. TLC = VC + RV 68 69 Depth and Rate of Ventilation • Eupnea- normal respiratory rhythm • Hypoventilation- caused by breathing either too shallowly or too slowly • CO2 levels increase and pH lowers. • Hyperventilation- a person over ventilates eliminates carbon dioxide faster than it is being produced causing the pH to increase. 70 Activity 25.2 • Expiratory capacity is equal to the sum of the tidal volume (TV) and expiratory reserve volume (ERV) • Is the maximum volume of air that can be forcefully exhaled after a normal inhalation. • Practice taking expiratory EC, ERV, TV and VC • Do Activity 25.3: calculate volumes and capacities follow instructions in manual 71 The End 72