The Sacrifice, The Labyrinth and the Minotaur
advertisement

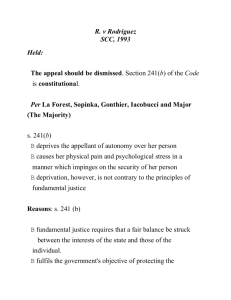
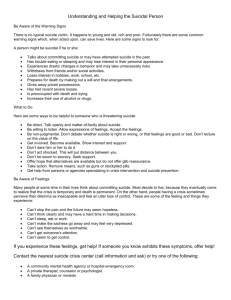
The Sacrifice, The Labyrinth and the Minotaur Silvia Baba Neal silviababaneal-psychotherapy.co.uk/mindspace Facts provided by the American Association of Suicidology Many beginning clinicians are unaware that suicide is an occupational hazard Approximately 1 in 5 psychotherapists (and as many as 1 in 2 psychiatrists and psychiatric trainees), lose a patient to suicide during the course of their career (McAdams and Foster, 2000, McIntosh, 2003, Ruskin et al., 2004) Novice clinicians have been found to experience higher rates of suicide among their clients than more seasoned clinicians. Experiencing the loss of a client by suicide can be psychologically traumatic for the provider, and may even become a career-ending event. Unfortunately, few training institutions or graduate programs prepare students for this possible traumatic loss (Reeves, 2010) Ariadne The clinician as survivour Significant emotional impact (Kleepsies, and Dettmer, 2000) Therapists have described client suicide as “the most profoundly disturbing event of their professional careers” (Hendin, et al. 2000) Fear of being blamed by supervisors, managers or trainers, and the client’s family (Farberow, 2005) May cause the therapist to seriously doubt their skills and competence therapist to consider abandoning a career in psychotherapy (Farberow, 2005) Therapist begins to use rules rigidly and defensively to prevent another suicide Therapists in training • Some authors have suggested that therapists in training may experience reactions even stronger than do their qualified colleagues (Brown, 1987; Kleespies et al., 1990, 1993) • Trainees may be less able to separate “personal failure from the limitations of the therapeutic process” (Foster & McAdams, 1999, p. 24) Five stages of grief model (On Death and Dying, Kübler-Ross, 1969) “The stages were never meant to help tuck messy emotions into neat packages. They are responses to loss that many people have, but there is not a typical response to loss as there is no typical loss. Our grief is as individual as our lives.” (Kübler-Ross and Kessler, 2006) www.suicidology.org/suicide-clinician-survivors Clinician 1 “Through shock little vibrations trickle through my body, a sinking feeling comes into my heart, then my stomach. I can not move. My mouth goes dry. Thoughts start tumbling through the air-landing on my body -- how, when, what does this mean, what will happen, will I be blamed, what is going on, how will I get through the day, don't scream must act professional, get concrete, O.K. I have a client waiting, stop the tears, act AS IF.” http://mypage.iu.edu/~jmcintos/therapists_mainpg.htm Clinician 2 “His death made absolutely no sense to me. After all, I had carefully assessed his suicidality during our last session and there was nothing there to alarm me. Yet, he was dead, and with his death, a part of me died as well. After the total shock and disbelief began to diminish, I started to sob, sobbing uncontrollably at times. I experienced extreme anxiety, gross sleep disturbances, and profound sadness. I was spiraling downward quickly, and I was emotionally paralyzed.“ Clinician 3 “Day 46: The feeling of loss has been very strong lately. I lost Mary. I lost being a member of the elite who has never lost a client to suicide. Already, I lost many hours of my time -planning, fretting, and talking. I lost sleep. I lost confidence. I may have lost part of my joy in being a therapist.” 7 months later: I still think of Mary. The waves of loss are farther between and much less overwhelming but the undercurrent is still there. Her suicide has touched me on many levels. During these past months, one professional implied that clinicians are not affected by a client's suicide and brushed me aside. I felt very invalidated and angry. Another colleague insisted that anti-suicide contracts really work. I felt defensive. I had taken this step and others, but it was not enough to save Mary's life.” Clinician 4 “I must say at the start that this is a very difficult case to discuss. In 25 years I have not publicly talked about it. This is a case where it is important to tell you all about my credentials as an analyst, as a senior university faculty member, etc. Notice that I included the word "Senior ." Can you believe that? After 25 years I still need to armor myself?” Trauma Trauma is “a sudden and violent emotion capable of provoking a permanent alteration of psychic activity” (Devoto and Oli, 1990 p. 2002 in Mazzetti, 2008, p.285) Prolonged stress following unprocessed trauma significantly impacts the neurological structures in the limbic system related to implicit memory and emotional life (thalamus, amygdala, hippocampus, and prefrontal cortex) (McEwen et al., 2009) the learning involved in trauma is resilient or “fixated” (Cozolino, 2010) Traumatic ego-states (Berne, 1961/2005) Berne (1961)– a traumatic stimulus modifies an ego state in an abrupt way. A traumatic ego-state is like “a warped coin, which would skew the pile” (1961/2005, p. 52) Penfield’s experiments (Penfield and Perot, 1963 in Milner, 1977) • Summary maps indicating all points from which electric stimulation of the exposed cortex has elicited complex auditory experiences in patients undergoing a surgical operation for epilepsy Trauma, stress response and the brain Psycho-social stress and the brain, (McEwen et al., 2009) Amygdala and hippocampus neurons exposed to chronic stress (Davidson and McEwen, 2012) One dendrite synapses (www.harvard.edu) Memory systems (Allen, 2011) Impasses: developmental perspective P2 (Mellor, 1980) A2 Type 1 P1 C2 A1 P0 A0 C0 Type 2 Type 3 Type 3 impasse When Mellor described his model of impasse, he suggested that third degree impasses can also develop later, whenever someone is: “(…) so traumatized or otherwise overloaded at the time they develop impasses that their current levels of functioning give way to earlier levels. This type of response results in the development of higher levels of impasse at ages when their development would no longer be possible if a strict developmental ordering would apply.” (Mellor, 1980, p. 218) Factors that may contribute to development of Type 3 impasse Your own Script System: core beliefs about yourself, others and the world (Erskine, 2010) and personality style Your Parent Ego state (P2): Rigid views about suicide influenced by religion, philosophy, public policy. Antidote: Tim Bond, 2000, Anddrew Reeves 2010 The context: “prevention-prediction culture” associated with the medical model views every completed suicide “a failure at instiutional or individual level” Antidote: Reeves, 2010 and Szatz, 2011, Mental Capacity Act, 2005, Suicide Act, 1961 Prescriptive, unchallenged, TA practices formally and informally handed down to the therapist i. e. “no-suicide” contracts Antidote: Erskine, 2009, Little, 2009, Hargaden and Stuart, 2000/2001 debate Psychological modifiers of stress-response (Sapolsky, 2004) Outlets for frustration A sense of predictability and control Social support A perception of life improving Self- Care • Activate support systems. Let it out: express feelings of anger, rage, despair, grief in a safe and appropriate context (therapy, supervision, peer supervision). • • • Take control: manage workload, be proactive in seeking information and support, deal with the tasks of writing reports, informing the relevant people etc. Silver lining: How can you use this experience to teach and support others? How can you improve your practice and the general pool of knowledge? Ethical considerations around: Collaborating with police investigation Case review- psychological autopsy (Marshall, 1980) Coroner’s report Notifying insurance company Letting the relevant people know (course director, placement facilitator) Calls of condolence (There is a GP/psychiatrist/social worker out there going through the same experience!) Receiving calls from family members or friends of the deceased Attending the Coroner’s Inquest Possibly attending the funeral, depending on circumstance (Bond and Mitchels, 2008) Bond, 2010, Gabriel and Casemore, 2009) Supervisers’ helpful/unhelpful responses The response of the immediate supervisor to the (supervisee’s) client’s suicide is a critical factor in influencing how the event personally or professionally affects trainee development (Foster & McAdams, 1999) Talking with a colleague who knew the patient or who had had a similar experience with a patient was beneficial in reducing isolation and providing support (Hendin et al., 2000) Providing emotional support and an intellectual context for understanding and growing from the experience of a client suicide (Brown, 1987) Supervisors helpful if they assured trainees that the way in which the trainee reacted to the suicide was clinically appropriate and if the supervisor shared responsibility for the outcome of the case (Kleespies et al. 1990, 1993) Unhelpful those supervisors who prematurely requested that trainees talk about their cases or immediately barraged them with stories of their own patients who suicided when the trainees were not ready (Kolodny et al., 1979) Need sufficient time to prepare themselves for the painful but necessary task of a “psychological autopsy” (Marshall, 1980) Recommendations for supervision (Knox et al., 2006) Allow supervisees to control when, where, how, and with whom they process the suicide Allow supervisees to access extra supervision, consultation, therapy Continue to provide a supportive time and place for supervisees to work through the client suicide even after the immediate responses seem to have abated Acknowledge/normalize that the effects of a client suicide, both short term (e.g., more thorough assessment for suicide) and long term (e.g., awareness of therapeutic responsibilities of suicidal clients, lingering feelings), may be painfully learned growth Bibliography • • • • • • • • • • • American Association of Suicidology [founded in 1997 to support clinician survivours] Clinician survivours testomonies: http://mypage.iu.edu/~jmcintos/therapists_mainpg.htm Comprehensive bibliography on suicide impact: http://mypage.iu.edu/~jmcintos/Surv.Ther.bib.htm Berne, E. (1961/2005) Transactional Analysis in Psychotherapy, London: Souvenir Press Bond, T. (2010) Standards and Ethics for Counselling in Action (third edition), London: Sage (Kindle edition) Bond, T. and Mitchels, B. (2008) Confidentiality and Record Keeping in Counselling and Psychotherapy, London: Sage Brown, H. N. (1987) The impact of suicide on therapists in training, in Comprehensive Psychiatry, 28(2): 101-112 Davidson, R. J. and McEwen, B. (2012) Social influences on neuroplasticity: stress and interventions to promote wellbeing, in Nature Neuroscience, 15: 689-695, Available online: http://www.nature.com/neuro/journal/v15/n5/full/nn.3093.html (Accessed 13 Nov. 2013) Erskine, R. (2009) The culture of transactional analysis: theory, methods and evolving patterns, in TAJ, Vol. 39, no. 1 Erskine, R. (2010) The Script system in Life Scripts [Richard Erskine, ed] Farberow, N. L. (2005, February). The mental health professional as suicide survivor. Clinical Neuropsychiatry: Journal of Treatment Evaluation, 2(1), pp. 13-20 Bibliography • • • • • • • • • • • Foster, V. A., & McAdams, C. R. (1999). The impact of client suicide in counselor training: Implications for counselor education and supervision. Counselor Education and Supervision, 39, 22–29 Gabriel, L. and Casemore R. (2009) Relational Ethics in Practice: Narratives from Counselling and Psychotherapy, East Sussex: Routledge Glaser (2007) The effects of maltreatment on the developing brain, in The Link, 16(2): 1 and 4 Hargaden, H.(2000) Escape hatches: Sacred rite or useful tool?, in TA UK, 58: 33-34 Hendin, Lipschitz, Maltsberger, Haas, and Wynecoop (2000) Therapists’ reactions to patients’ suicides, in American Journal of Psychiatry, 157(12): 2022: 2027 Kleespies, P. M., Smith, M. R., & Becker, B. R. (1990). Psychology interns as patient suicide survivors: Incidence, impact, and recovery. Professional Psychology: Research and Practice, 21, 257–263. Kleepsies, P. M., & Dettmer, E. L. (2000). The stress of patient emergencies for the clinician: Incidence, impact, and means of coping. Journal of Clinical Psychology, 56, 1353-1369 (especially 1354-1355, "Patient Suicidal Behavior"; also includes a section on "The Impact of Working with Suicidal Patients," pp. 1357-1358) Kleespies, P. M., Penk, W. E., & Forsyth, J. P. (1993). The stress of patient suicidal behavior during clinical training: Incidence, impact, and recovery. Professional Psychology: Research and Practice, 24, 293–303. Kleespies, P. M., Smith, M. R., & Becker, B. R. (1990). Psychology interns as patient suicide survivors: Incidence, impact, and recovery. Professional Psychology: Research and Practice, 21, 257–263. Kolodny, S., Binder, R. L., Bronstein, A. A., & Friend, R. L. (1979). The working through of patients’ suicides by four therapists. Suicide and Life-Threatening Behavior, 9, 33–46. Knox, S. Burkard, A. W., Jackson, J. A., S., Shaack, A. M. , Hess, S. A. (2006) Therapists-in-training who experience a client suicide: Implications for supervision, in Professional Psychology: Research and Practice, 37(5) Available online: http://epublications.marquette.edu/cgi/viewcontent.cgi?article=1005&context=edu_fac (Accessed 13 Nov. 2013) Bibliography • • • • • • • • • • • • • • Kubler-Ross, E. (1969/2011) On death and dying, New York: Touchstone (Kindle Edition) Kubler-Ross, E. and Kessler, D. (2006) On Grief and Grieving: Finding the Meaning of Grief Through the Five Stages of Loss, Scribner: New York Little, R. (2009) Understanding the psychodynamics of suicidal clients: exploring suicidal and para-suicidal states, in TAJ, vol. 39, no. 3 Marshall, K. A. (1980) When a patient commits suicide in Suicide and Life-Threatening Behavior, 10(1): 29-40 Mazzetti, M. (2008) Trauma and migration: A transactional analysis approach toward refugee and torture victims, in the TAJ, vol. 38 no. 4 McAdams, C. R., III, and Foster, V. A. (2000). Client suicide: Its frequency and impact on counselors, in Journal of Mental Health Counseling, 22, 107-121 Milner, B. (1977) Memory Mechanisms, CMA Joural vol. 116 McEwen, B, Roozendaal, B. and Chattargi, S. (2009) Stress, memory and the amygdala in Nature Reviews, 10: 423-433 Available online here: http://www.nature.com/nrn/journal/v10/n6/full/nrn2651.html Mellor, K. (1980) Impasses: A Developmental and Structural Understanding, Transactional Analysis Journal, 10 (3): 213-222 Porges, S. W. (2011) The Polyvagal Theory: Neuropshysiological Foundations of Emotions, Attachment, Communication and Self-Regulation, New-York: Norton Reeves, A. (2010) Counselling Suicidal Clients, London: Sage Publications Ruskin, R., Sakinofsky, I., Bagby R. M., Dickens, S., Sousa, G. (2004) Impact of patient suicide on psychiatrists and psychiatric trainees, in Academic Psychiatry, 28(2): 104-110 Stewart, I. (2001) Closing escape hatches, always therapeutic, never routine, TA UK, No. 6, Summer, p. 29 Szatz, T. (2011) Suicide prohibition – The shame of medicine