History of Addictions & Recovery
advertisement

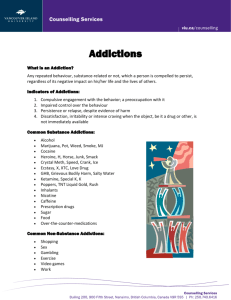
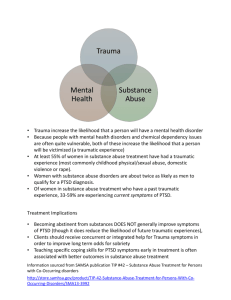
The Art and Science of Treating Clients with Addictions and Dual Diagnosis Problems in Community Counseling Setting. Cathy Moonshine, Ph.D., MAC, CADC III School of Professional Psychology Pacific University Abstract This paper will focus on how to treat mild to moderate addictions in a community counseling setting that primarily provides mental health services. The paper will discuss the process of diagnosing and initial level of care placement. When to refer for medical evaluation, detox services and formal addictions treatment program will be reviewed. When and how to chose an abstinence or harm reduction treatment approach. Recommendations will be made for the use of the evidence based practices of ASAM PPC-II-R, Motivational Interviewing, Matrix Model, Dialectical Behavior Therapy and 12-Step Facilitation. Coordinating and collaborating care when client is enrolled in treatment program. Treatment Team • Students received a brief overview of diagnosing and treating addictions in the first year course work. • Self select to be placed on substance use disorder treatment team at community counseling setting. • Student clinicians receive individual and group supervision focused on treating addictions and dual diagnosis clients. • Students can also take a semester long course on addictions treatment as an elective. Prevalence According to the Center for Substance Abuse Treatment (2005) anywhere from 20%-50% of individuals seeking mental health treatment also meet criteria for a co-occurring disorder (COD). “The term co-occurring disorders (COD) refers to co-occurring substance-related and mental disorders. Clients said to have COD have one or more substance-related disorders as well as one or more mental disorders” (Center for Substance Abuse Treatment, 2006). Use • • • • • • • Use can be defined as the ingestion of alcohol or other drugs for encouragement, relaxation, etc that does not negatively impact the individual’s life. This impact can be in terms of: Physical Health Emotional Well-being Social Skills Relationships Adequate Work Performance Legal Financial Addiction Complex progressive behavior patterns having biological, psychological and behavioral component’s with an individual’s pathological involvement in or attachment to it, subjective compulsion to continue it and reduced ability to exert personal control over it. Substance Intoxication The results from the recent ingestion of a substance such as alcohol, marijuana, heroin or even caffeine (APA, 2000). Substance Withdrawal This occurs when an individual stops using a substance in which he or she has become physiologically, cognitively and behaviorally dependent. It is most important to intervene if there are medical concerns. Alcohol and benzodiazepines are the most medically compromising (APA, 2000). Substance Abuse • • • • A maladaptive pattern of substance use leading to clinically significant impairment or distress, as manifested by one or more of the following within the last 12 months: Failure to fulfill major life obligation Use when physically hazardous Legal problems related to use Continued use despite having persistent or recurrent social or interpersonal problems (APA, 2000) Substance Dependence • • • • • • • A maladaptive pattern of substance use, leading to clinically significant impairment or distress, as manifested by at least 3 of the following in the same 12 months: Tolerance Withdrawal Substances taken in larger amounts than planned Persistent desire or inability to cut down Great deal of time spent in activities related to use Important social, occupational or recreational activities given up Continued use despite knowledge of having a persistent or recurrent physical or psychological problem (APA, 2000) Substances that qualify • • • • • • • • • • • Alcohol Amphetamine Caffeine Cannabis Cocaine Hallucinogens Inhalant Nicotine Opioids Phencyclidine Sedatives, hypnotics or anxiolytics (APA, 2000) Polysubstance Dependence This diagnosis is reserved for behavior during a consecutive 12-month period in which the person has repeatedly used at least three groups of substances, not including caffeine and nicotine, but no single substance predominated. (APA, 2000) Initial Screening Tools • CAGE – – – – Cut down Annoyed by use Guilty about use Use as an eye opener • CRAFFT – – – – – – Car Relax Alone Family & Friends Forget Trouble Initial Screening Tools • • • • Alcohol Use Disorder Identification Test (AUDIT) Drug Use Disorder Identification Test (DUDIT) Michigan Screening Alcohol Test (MAST Drug Abuse Screening Test (DAST) Initial Level of Care Placement • Is the client appropriate for outpatient therapy in a student clinic? – – – – – – What substances are being use? How often is the use? Use may be physical risk? When did use begin? Any previous treatment? Willingness to attend community support? Medical Evaluation In most cases it is recommended that the client be evaluated by a primary care physician to rule out any medical problems and support treatment. Detoxification If the client requests detox or use indicates a need for detox, then a referral should be made. In particular, if the client is using alcohol and/or benzodiazepines then detox is recommended. While detox from heroin, methadone or opioid pain pills may not be medically compromising, social detox may be very useful in establishing initial abstinence. Formal Addictions Treatment Program Referral • When using in a dangerous ways • If drug screens are recommended • Meets criteria for dependence of two or more substances • Needs significant case management services • Will benefit from Intensive Outpatient or Residential Services • Refuses to attend community supports • Indications of dishonesty and delinquency Psychiatric Medications • Based on the prevalence of co-occurring disorders, psychiatric evaluation is likely appropriate • Inform psychiatric prescriber of addictions issues • Medications that are contraindicated for addictions are – Ritalin and Adderall – Valium, Xanax, Klonopin or other benzodiazepines – Vicodin, Oxycodone or other opiod pain killers Abstinence or Harm Reduction • Abstinence: – – – – Evidence of biological/genetic component Demonstrated inability to cut down Using when physically/psychological dangerous Exacerbates mental health issues Abstinence or Harm Reduction • Harm Reduction: – – – – Young adults & college students Use creates mild to moderate problems Level of functioning not impacted by use Other negative impacts of use are non-existent • Harm Reduction as a means to Abstinence ASAM PPC-II-R • American Society of Addiction Medicine publishes the Patient Placement Criteria 2nd Edition Revised. • This publication is used for initial evaluation, placement, continued stay, transfer and discharge planning. ASAM PPC-II-R Life Dimensions 1. Intoxication and Withdrawal Potential 2. Biomedical 3. Emotional, Behavioral and Cognitive 4. Readiness for Change 5. Relapse, Continued Use and Continued Problem 6. Recovery Environment ASAM PPC-II-R Levels of Care 0.5 Prevention & Early Intervention 1 Outpatient Services 2 Intensive Outpatient Services 3 Residential Treatment 4 Inpatient Hospitalization Stages of Change • • • • • • Pre-contemplation Contemplation Preparation Action Maintenance Relapse or return to old behavior/patterns (Prochaski and DiClemente, 1996). Motivational Interviewing • • • • Extrinsic & intrinsic motivation Enlightened self-interest Developing discrepancy Rolling with resistance – Supportive & strategic interventions • Decisional balance • Change plan worksheet (Miller and Rollnick, 2002). Matrix Model The model integrates treatment elements from a number of strategies, including relapse prevention, motivational interviewing, psycho-education, family therapy, and 12-Step program involvement. Combines Evidence Based Practices: • Motivational Interviewing • CBT & Classic Conditioning • Drug & Alcohol Education • Brain Chemistry • Stages of Recovery The basic elements are group sessions, individual sessions, along with encouragement to participate in 12-Step activities, delivered over a 16-week intensive treatment period (Obert, Rawson, McCann, & Ling, 2006). Dialectical Behavior Therapy • Learn and practice skills in the areas of: – – – – Mindfulness Emotional Regulation Distress Tolerance Interpersonal Effectiveness • Diary Cards • Chain Analysis • Ultimate goal to build a life worth living (Moonshine, 2008). 12-Step Facilitation 12-Step Facilitation encourages acceptance of the addiction, commitment to abstinence and willingness to participate actively in 12-step fellowships as a means of establishing recovery. • • • • • • • • Evaluate the substance use problems and advocate abstinence. Explain basic 12-step structure and concepts. Encourage client to engage in 12-Step meetings Facilitate ongoing participation Discuss and support client working each of the 12-Steps Include support system in the therapeutic process Utilizing 12-Step network when in crisis Assist the client making a moral inventory and engaging in amends • Encourage involvement in 12-Step beyond formal therapy Coordinating and Collaborating Care • Regular conversations with treatment program • Collaborative treatment planning • Include ancillary providers such as PCP & dentist • On the same pages with community support meetings References American Psychiatric Association, (2000). Diagnostic and statistical manual of mental disorders (4th ed.) (DSM-IV-TR). Washington, D.C. Center for Substance Abuse Treatment (2006). Definitions and terms relating to co-occurring disorders. COE Overview Paper 1. DHHS Publication No. (SMA) 06-4163. Rockville, MD: Substance Abuse and Mental Health Services Administration, and Center for Mental Health Services. Center for Substance Abuse Treatment (2005). Substance Abuse Treatment for Persons with Co-Occurring Disorders. Treatment Improvement Protocol (TIP) Series 42. DHHS Publication No. (SMA) 05-3992. Rockville, MD: Substance Abuse and Mental Health Services Administration. Obert, J.L., Rawson, R.A., McCann, M.J., & Ling W. (2006). Counselor’s treatment manual: Matrix Intensive outpatient treatment for people with stimulant use disorders. Rockville, MD: Substance Abuse and Mental Health Services Administration