ATPMetabolism - frozencrocus.com
advertisement

General Overview of Intermediary Metabolism
Just about anything you eat is metabolized to carbon dioxide &
water with the concomitant synthesis of ATP to provide the
chemical energy necessary to build and repair cellular components
or to sustain muscle contraction.
An Exercise-Centric View of Metabolism
ATP used up by muscle contraction can be regenerated through 4 processes:
1-MK
2-CPK
3-Glycolysis
4-Oxidative Phosphorylation
The Myokinase reaction:
ADP + ADP → ATP + AMP
is impossible to sustain at maximal rates because AMP cannot be
regenerated to ADP and ATP; it can, however, be used to generate
fumarate through the purine nucleotide cycle (costs NRG):
AMP + H2O → IMP + NH4+
IMP + Aspartate + GTP → AMP + Fumarate + GDP + Pi
The Creatine Phosphokinase reaction:
ADP + CP ↔ ATP + C
is impossible to sustain at maximum activity because of relatively
limited supplies of CP in the cell and CP can’t be regenerated very
quickly if the vast majority of ATP is being used up for the
contractile demands. It is however, more active than MK because it
has a lower Km: ~0.02 mM vs. ~0.120mM; [ADP] rest ~ .08, Ex
~0.15) therefore CPK is always active – indicating an important role
in shuttling regulating ATP/ADP/Pi while MK is active only at higher
[ADP]
Just for fun we should not view ATP generation for energy as the only metabolism
happening:
A Nutritionist’s View of Metabolism (& Cell Function)
Minerals
(functional) components of enzymes, molecular binding
factors, catalysts . . .
Vitamins
co-factors, antioxidants, gene regulators . . .
Amino Acids
NRG, amino acid sequence produces structure of enzymes,
DNA, RNA, NAD+, FAD+ . . .
Fatty Acids
NRG, part of structure of some enzymes, Phospholipids . . .
Carbohydrates
NRG, component of DNA, RNA, ATP, NAD+, FAD+ . . .
Enzymes perform chemical reactions of metabolism
- requires (protein) synthesis of enzymes (duh!)
- many enzymes contain minerals as part of their structure
- many enzymes require co-factors which
contain vitamins as part of their structure.
Protein synthesis
- requires DNA, RNA, mRNA, GTP . . .
- synthesis enzymes require Cr+?, Mg++, Zn+ to function
Synthesis of DNA, RNA, ATP, GTP . . .
- folic acid, B12, glucose, aa, PO4 (structure)
- enzymes for synthesis require Zn+,Cr+?, Mg++, to function
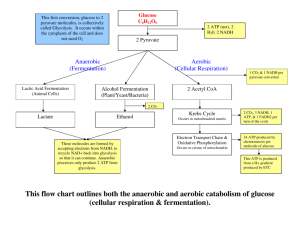
Getting back to the ATP thing, these are
some of the major metabolic pathways for
resting and exercise metabolism:
Glycolysis: produces pyruvate for acetyl
CoA production in mitochondria, produces
NADH (electrons) for ETC in mitochondria,
anaerobic production of ATP
MK & CPK: anaerobic production of ATP
TCA: accepts acetyl-CoA for citrate
synthesis, production of NADH (electrons)
for ETC, “anaerobic” production of GTP
β-oxidation: produces acetyl CoA for TCA
Transamination: produces pyruvate, or
acetyl CoA, or TCA intermediates
ETC: electrons from TCA cycle & glycolysis
are “joined” to oxygen to make water & the
production of ATP
Pentose Phosphate Pathway: production of
ribose and NADPH for nucleotide and other
synthesis processes
Glycolysis (+ PDH), β-Oxidation, & several transamination
reactions lead to the production of acetyl CoA which transfers
the acetate group to oxaloacetate in the mitochondria for
further breakdown to CO2 and H2O.
Glycolysis is the metabolic pathway through which glucose is
broken down to pyruvate in the cytosol.
In order to prevent glucose
from building up inside the cell
and producing a huge osmotic
(and gradient) problem it is
immediately phosphorylated
by the enzyme hexokinase
(using up one ATP molecule).
The resulting glucose 6phosphate can either be
stored as glycogen or
progress through the
glycolytic pathway.
Step 3, catalyzed by the
enzyme Phosphofructokinase
(PFK) is the rate-limiting step
in glycolysis. It converts
fructose 6-P to fructose 1,6
bisP.
After several more steps two
pyruvates & 2 NADH + H+ are
made with 4 ATP being
produced; a net gain of 2 ATP
for this pathway.
The 2 pyruvates and 2 NADH +
H+ are picked up by the
mitochondria.
©C. Murray Ardies, 2008
Inside the mitochondria, the
pyruvate is converted to 2
acetyl CoA, 2 CO2 and 2
(more) NADH + H+ by the
enzyme PDH.
The acetyl CoA condenses
with oxaloacetate (OAA) to
synthesize citrate and leave
behind the CoA.
Through a series of enzyme
reactions, the citrate is
converted back into OAA
with the concomitant
production of 1 GTP, 1
FADH2, 3 NADH + H+, and 2
CO2.
The NADH and FADH are
transferred to the ETC while
most of the CO2 diffuses to
the blood (and lungs) for
disposal. The GTP can be
used for protein synthesis or
converted to ATP for use as
“NRG”.
©C. Murray Ardies, 2008
REGULATION OF GLYCOLYSIS
The rate limiting enzyme of glycolysis: PFK, is the slowest one of the
pathway. It is regulated predominantly by ATP, citrate, AMP, H+ and
fructose 2,6 Bis-P; with the 2,6 BP being the major regulator in liver and a
relatively minor regulator in muscle.
ATP, H+, and citrate greatly inhibit it, promoting storage of glucose as
glycogen whenever ATP levels are high. When ATP levels decrease (slightly)
as a result of extreme rates of ATP use, such as with maximum muscle
contraction, the inhibition of PFK is attenuated and rates of pyruvate and
ATP production increase.
When AMP levels increase from increasing MK activity due to increasing
production of ADP during exercise, rates of glycolysis are greatly speeded up.
Maximally stimulated rates of glycolytic enzyme activities can exceed the
maximal velocities of mitochondrial enzymes by about 40x.
Regulation of glucose levels in the blood is very important
Normal Fasting (Serum) ~ 70 – 100 mg/dl
Elevated = Diabetes
Low = Hypoglycemia
Insulin from pancreas stimulates uptake of glucose into muscle
cells by activating the GLUT4 transporter. When serum levels
of glucose decrease too much, then the pancreas releases
glucagon to stimulate the liver and kidney to break down
glycogen to glucose and release glucose into the blood
(glycogenolysis). Adrenals will release cortisol if levels stay too
low to enhance breakdown of protein in muscles to release
amino acids so the liver can pick up the amino acids and make
them into glucose (gluconeogenesis).
Epinephrine stimulates the triglyceride lipase to cleave fatty acids
off of the glycerol; making lots of fatty acids available for NRG.
Fatty acids are transported into the mitochondria by a carnitine transporter
which is in the membrane. (Note that ascorbic acid is required for carnitine
synthesis.)
Once inside the
mitochondria the
fatty acids are
oxidized into twocarbon fragments
(acetate) which are
utilized by the TCA
cycle in the form of
Acetyl-CoA.
The central role of
glycolysis and TCA cycle
in intermediary
metabolism is illustrated
by all the different
compounds which
originate from these
pathways and which can
be metabolized
through these
pathways
Glycolysis + PDH, βOxidation & some
transamination
reactions produce
acetyl CoA (different
transamination
reactions produce TCA
cycle intermediates)
The GTP
produced can be
used for protein
synthesis while
the NADH+H+/
FADH2 donate
their electrons to
the electron
transport chain
In the simplest terms, NADH passes its
electrons to complex I while FADH gives
them to Co-Q.
The electrons are passed alomg the ETC
to complex IV where they are “joined” to
oxygen.
At the same time, hydrogens are
transferred from the matrix to the intermembrane space, creating a proton
gradient.
When the protons move through the ATP
synthase to return to the matrix, their
movement through the synthase powers
the regeneration of ATP from ADP + PO4
Note from the preceding slide that some of the hydrogens that make it to the
intermembrane space can leak out when the membrane gets too hot and some
leak back into the matrix through the mitochondrial permeability transition (and
other mitochondrial uncoupling proteins) which are activated by calcium
coming in through the calcium uniporter.
Also note that electron carriers can autooxidize directly to oxygen, creating
oxygen radicals (Co-Q is the major site of autooxidation) with as much as 5% of
resting oxygen use due to this phenomenon.
All of these processes represent a significant amount of electron transfer to
oxygen without concomitant ATP synthesis and all become much more active
when exercising hard, creating interesting complications when trying to
interpret oxygen consumption and its association with athletic performance.
When accounting for ATP synthesis on the basis of the actual proton cost, you
will get ~ 2.5 ATP for each NADH + H+ and ~ 1.5 ATP for each FADH2.
Because of hydrogen leaks & oxygen-radical chemistry, actual yields of ATP
from the electron donors are much less than the proton cost-based ~ 2.5 ATP &
~ 1.5 ATP; a yield that will diminish at higher temperature and higher calcium
conditions (think exercise here).
Theoretical efficiency of ATP production from 1 molecule of
glucose:
Glycolysis produces 2 pyruvate molecules and 2 NADH + H+
(enters the mitochondria as FADH2), PDH produces 1 NADH
+ H+ and 1 acetyl CoA for each pyruvate molecule, and TCA
cycle produces 3 NADH + H+ and 1 FADH2 for each pyruvate
molecule for a total of 9 NADH + H+ (x 2.5) to produce 22.5
ATP, 3 FADH2 (x 1.5) to produce 4.5 ATP, and a net gain of 2
ATP in glycolysis and ~1.5 ATP (GTP) in TCA cycle for a
grand total of ~ 30 ATP for each glucose molecule oxidized to 6
CO2 and 12 H2O.
(It costs H+ to transport GTP (ATP) out of the mitochondria
which makes the yield less than the 2 GTP actually produced)
6 CO2 produced for 6 O2 (RER: 6/6 = 1) used and ~ 30 ATP
produced gives 30/6 = ~ 5 ATP/C and 30/6 = ~ 5 ATP/O2 used
Theoretical efficiency of ATP production from 1 molecule of
palmitate, a 16 carbon saturated fatty acid.
7 turns of β-oxidation produces 7 NADH + H+ and 7 FADH2 and
8 acetyl CoA.
Each acetyl CoA produces 3 NADH + H+, 1 FADH2, and 1 GTP
for a total production of 31 NADH + H+ (x 2.5) to produce 77.5
ATP, 15 FADH2 (x 1.5) to produce 22.5 ATP and 8 GTP to
produce a net of 6 ATP for a grand total of 106 ATP for each
palmitate molecule metabolized to CO2 and H2O.
16 CO2 produced for 23 oxygen used (RER: 16/23 = 0.695) and
106 ATP produced gives 106/16 = 6.625 ATP/C and 106/23 = 4.6
ATP/O2 used.
In comparing fat to glucose as a substrate it is clear that
glucose gives a better ATP yield per oxygen used: ~ 5 for
glucose vs. ~ 4.6 for palmitate indicating that glucose is a
better substrate to use when efficiencies of ATP synthesis
through the ETC are increasingly diminished as metabolic
intensity increases (think exercise).
On the other hand, fat gives a better ATP yield per carbon
stored: ~ 6.625 for palmitate vs. ~ 5 for glucose. Thus fat
makes for a better storage form of substrate; especially when
you consider that glycogen is hydrophilic: 1:1 (or greater)
water:glycogen.
Summary Of Substrate Use:
ATP Yield /
O2 Used
ATP Yield/
CO2
Water
Content
(stored)
Glucose/
Glycogen
~ 5/
~ 5.2
~5
~ 5.2
~5:1
Palmitate
~ 4.6
~ 6.625
0
Of course, these are the theoretical maximums of total
ATP yield: ~ 106 ATP for each palmitate molecule
metabolized to 16 CO2 and 46 H2O & ~ 30 ATP for each
glucose molecule oxidized to 6 CO2 and 12 H2O.
It doesn’t really happen that way in vivo…
Notice that heat increases the permeability of the
mitochondria membrane to H+. That means that
efficiency of ATP synthesis MUST be less than 2.5
ATP / NADH and 1.5 / FADH… even at rest!
The membranes are in fact, permeable to several
compounds produced in the mitochondria, including
some produced in the TCA cycle (especially citrate,
oxaloacetate & succinyl Co-A).
If TCA intermediates leak out, they must be replaced or the cycle shuts down: w/o
oxaloacetate to condense with Acetyl CoA, citrate simply cannot be made and the cycle
is done for… and if they leak out… they obviously can’t be oxidized as a source of
electrons – another reason for less than 2.5 ATP / NADH…
Regulation of PDH, TCA cycle, and ETC are exceedingly
important; if they worked fast all of the time then the electron
carriers NAD and FAD would be full of electrons (FADH2 and
NADH + H+) and they can easily autooxidize to produce
superoxide anions.
These radicals react to produce peroxide:
O2 -
+ O2 -
H2 O 2
+
O2
Peroxide and superoxide can then react to produce the dreaded
hydroxyl radical:
O2-
+
H2O 2
.OH + -OH +
O2
Note that as molecular oxygen picks up electrons and reacts with
other oxygen radicals (ROS) the end result is the production of
water and hydroxyl radicals.
In the presence of free iron, rates of ROS chemistry are
greatly accelerated! Highly relevant if ROS-mediated iron
release from aconitase occurs…
Recall the oxygen radical chemistry from the previous slide which produces
the hydroxyl radical:
O2 -
O2-
+ O2-
H2 O2
+ H2O2
.OH
+
O2
+ -OH +
O2
In order to protect ourselves from the consequences of these reactions we have
antioxidant enzymes which help avoid the problem:
Manganese or copper/zinc
Superoxide
Dismutase
O2 -
+ O2-
H2 O2
+
O2
iron
Catalase
H2O2 + H2O2
2 H2O + O2
The enzymes SOD and CAT reduce oxygen radicals to water and oxygen,
preventing the build-up of the hydroxyl radicals and reducing ROS damage –
an important consideration for exercise (recall IOM recommendations) since
exercise can greatly enhance the production of ROS.
Other means exist to reduce ROS-mediated
damage such as ingesting sufficient amounts of the
antioxidant: vitamin C (ascorbic acid)
Notice that ascorbate can be
regenerated by
glutathione
Vitamin E also acts as an
antioxidant; although it
specifically acts on lipid
radicals, not watersoluble ones like ascorbic
acid.
Notice, however, that it
can be regenerated by
ascorbic acid/glutathione
(and also directly by
glutathione).
Because a high rate of
metabolism during
exercise is a
potent ROS
generator,
regular exercise
enhances the need for
antioxidants.
So… if TCA intermediates leak out, how do we regenerate
the OAA? … Through what are called: Anapleurotic
reactions: The major anapleurotic reactions are catalyzed
by the enzymes: pyruvate carboxylase; glutamate
dehydrogenase and alanine aminotransferase.
Note that GDH produces
ammonia (toxic) while ALT
produces alanine (from
pyruvate).
Both PC and ALT may have
important implications for
high-intensity exercise:
Pyruvate can be made into
useful non-lactate products
and the alanine diffuses out of
the cell very easily, lactate
does not!
Recall that Ile & Val are
metabolized mainly in muscle
and also can be made into
Succinyl Co-A; normal aa
metabolic pathways that also
can be considered
anapleurotic…
Overview of the major anapleurotic reactions…
PDH activity is enhanced by NAD+, Co-A, Ca++, and insulin and
inhibited by Acetyl CoA, NADH + H+, and ATP
Citrate synthase is inhibited by ATP
α-ketoglutarate dehydrogenase activity is inhibited by NADH +
H+ and Succinyl CoA and both α-ketoglutarate dehydrogenase
and isocitrate dehydrogenase are activated by Ca++
Cytochrome oxidase activity is enhanced by ADP while the ATP
synthase is activated by Ca++ and ETC as well.
-note that just about all of the regulated enzymes in
mitochondria can be activated by Ca++ (they are actually more
sensitive to calcium than the other allosteric regulators)
ensuring increased ATP supply immediately as it is needed while
there are multiple inhibitors to prevent unnecessary electron
transfer.
Recall that H+ and citrate inhibit glycolysis and that it can only be maximally stimulated a lot by
AMP (citrate leaks out of the mitochondria when you make lots of it!). This ensures that rates of
glycolysis will more or less match rates of oxidative phosphorylation at all rates of ATP demand,
at least until rates of glycolysis speed up due to increasing muscle contraction.
We must remember that both mitochondria and LDH enzymes co-exist in cells and therefor they
“compete” for the pyruvate that is produced by glycolysis. Because the muscle form of LDH
maintains [lactate] >> {pyruvate] some of the pyruvate produced through glycolysis will always
be converted to lactate while some is picked up by the mitochondria. Losing lactate from the cell
would be awkward because then it wouldn’t be made into pyruvate by LDH so it is transported
out of the cell only at relatively high [lactate]. Thus lactate diffuses out of muscle cells at high
rates of lactate production (i.e. during exercise) and is an indicator that the LDH is outcompeting the mitochondria for pyruvate - a situation that can change when more mitochondria
are synthesized.
Oxygen consumption will continue to increase at higher workloads (up to the your maximum
ability to remove electrons from “food”) while increasing inefficiencies in oxidative
phosphorylation occur at increasing temperature-, ROS-, and calcium-loads.
Thus your maximum capacity to produce ATP through oxidative (aerobic) pathways; “aerobic
max” (to make ATP), is reached at a workload somewhat similar to that producing the
appearance of lactate in the blood (lactate threshold, OBLA). This approximates to that point
where increasing inefficiencies in coupling O2 consumption to ATP synthesis (due to increasing
heat and radical formation at higher work-loads) match the increasing rate of flow of electrons
from substrates to O2 through the metabolic pathways to produce no net gain in “aerobically”
produced ATP.
An interesting issue….recall the major
anapleurotic reactions…
…what might
happen with a
specific
nutritional deficit
… such as
say…ascorbic
acid???
Ascorbic acid a necessary co-factor carnitine synthesis as well as an antioxidant
Because aconitase and Co-Q are
especially sensitive to oxygen-radical
attack, ascorbic acid deficiency should
lead to a decrease in β-oxidation of fatty
acids, a decrease in α-KG production
from citrate, a decrease in FADH coupling
to Co-Q, and an increase it citrate leaking
The major compensatory mechanism(s) is simply to accelerate the
velocity of the glycolytic and anapleurotic enzymes to make up for the
deficits…