Nucleotide metabolism
advertisement

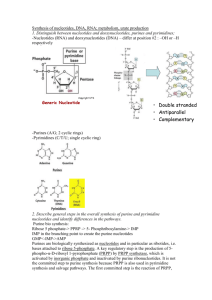
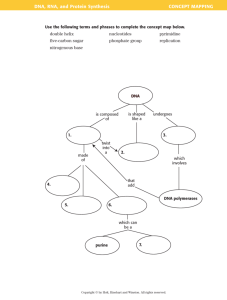
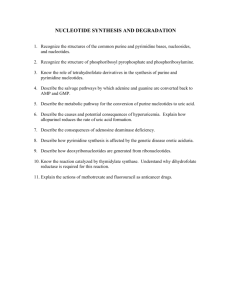
Dr. S.Chakravarty, MD A 30 year old man comes with severe pain in great toe of right foot !! Learning objectives • Discuss the components of Nucleotides and molecules contributing to formation of purine and pyrimidine ring • Describe the Pyrimidine metabolism and its defects – Orotic acidurias and Megaloblastic anemias • Differentiate the features of Denovo and salvage pathways of purine metabolism • List the causes of Hyperuricemias, its clinical features and treatment • Discuss the clinical features and the enzyme defects in SCID and Lesch - Nyhan syndrome – clinical features • List the anticancer drugs acting on purine and pyrimidine metabolism and its mechanism of action Importance of nucleotides: • Building blocks of nucleic acids – DNA and RNA • Act as co-enzymes – FAD, NAD, NADP • Second messengers – cAMP and cGMP • Energy currency – ATP and GTP • Nucleoside and nucleotide analogs – treatment of cancer. • Donors of sugar moiety – UDP-Glucuronic acid. Nomenclature • Base= (Purines or Pyrimidines) • Nucleosides = Base + sugar • Nucleotides = Base + sugar + phosphate • Sugar = Ribose in RNA = 2 - Deoxyribose in DNA Purines Pyrimidines Mnemonic : CUT Pyrimidine biosynthesis • The donors of C and N atoms to the pyrimidine ring are Aspartate, Glutamine and CO2 • The pyrimidine ring is initially assembled & the ribosephosphate is added later (compare to purine biosynthesis) De From Kaplan Step 1 lecture notes CO2 + ATP Glutamine -VE OROTIC ACIDURIA -VE -VE Hydroxyurea Dihydrofolate reductase -VE 5-flurouracil -VE Methotrexate – Eukaryotes Trimethoprim – prokaryotes Pyrimethamine - protozoal Conversion of the ribonucleotides to deoxyribonucleotides Ribonucleotide diphosphate (ADP, GDP, CDP, UDP) Thioredoxin, NADPH+H+ Ribonucleotide reductase (-) Hydroxyurea Deoxyribonucleotide diphosphate (dADP, dGDP, dCDP, dUDP) Carbomyl phosphate synthase • • • • • • Carbamoyl phosphate synthetase I - involved in urea synthesis - uses free ammonia as the source of nitrogen - occurs in liver mitochondria - activated by N-acetylglutamate - not affected by UDP or UTP • • • • • • Carbamoyl phosphate synthetase II - involved in pyrimidine synthesis - uses glutamine as the source of nitrogen - occurs in the cytosol of all nucleated cells - Inhibited by UDP and UTP, Activated by PRPP, ATP - not activated by N-acetylglutamate Orotic aciduria • Deficiency in UMP synthase activity – Orotate Phosphoribosyl transferase – Orotidylate decarboxylase • Pyrimidine synthesis is decreased, excess orotic acid is excreted in urine (hence Orotic aciduria) • Due to demand for nucleotides in red blood cell synthesis megaloblastic anemia – Important :- Unresponsive to vit B12 and folic acid, Orotic aciduria • Administration of Uridine improves anemia (Uridine is used for the synthesis of thymidine and cytidine) • UTP is feedback inhibitor of CPS II, uridine administration results in a fall in orotic acid levels. Orotic aciduria – other causes: • Urea cycle defect : Ornithine transcarbomylase (OTC) • Drugs – Allopurinol competes with orotic acid for the enzyme orotate phosphoribosyl transferase . Question • A one year old female child is weak and anemic. The child was found to have megaloblastic anemia. The height and weight of the child are less than normal. Urine demonstrates an elevated level of orotic acid excretion and normal blood ammonia levels. • Which of the following enzyme will be deficient ? – A. Ornithine transcarbamoylase – B. Orotate Phosphoribosyl transferase Pyrimidine catabolism • Dephosphorylated to nucleotide • Cytosine converted to uracil • Uracil converted to b-alanine • Thymine converted to b-aminoisobutyrate NH3 cytosine cytosine deaminase NH2 uracil CO2 CH2 -alanine uracil NH3 CH2 C - O O NH3+ CO2 thymine -aminoisobutyrate NH3 CH2 H C CH3 C - O O Purine Biosynthesis N10-Formyl Tetrahydrofolate Purine synthesis- De novo pathway Ribose- 5 phosphate PRPP synthase Allopurinol 6- Mercaptopurine Azathioprine PRPP (+) (-) PRPP Amidotransferase 5-phosphoribosylamine (-) IMP (Hypoxanthine base) Aspartate AMP Glutamine GMP (-) Purine catabolism Adenosine Severe combined Immunodeficiency ADENOSINE DEAMINASE NH3 (-) Guanosine T-cell deficiency Insosine Ribose 1 P (-) (-) Purine nucleoside phosphorylase Purine nucleoside phosphorylase Hypoxanthine Ribose 1 P Guanine Guanase Xanthine Oxidase Xanthine Xanthine Oxidase Uric acid Urine (-) Allopurinol (-) Allopurinol 90% 10% From Kaplan Step 1 lecture notes Purine salvage pathway Inosine Guanine (90%) Hypoxanthine (90%) PRPP PRPP Hypoxanthine Guanine phosphoribosyl transferase GMP IMP (-) •Purines from Diet •Nucleic acid turnover •Other nucleotide metabolism Adenine Adenine phosphoribosyl transferase AMP Lesch Nyhan syndrome Advantage of purine salvage pathway: • Reutilization of nucleotides • Prevents loss of ATPs which are required for denovo purine synthesis • Nucleotides formed in the salvage pathway inhibits denovo pathway at the rate limiting step • Decreases uric acid formation – end product of purine catabolism Conversion of nucleosides to nucleotides • NMP + ATP Nucleoside Mono phosphate kinase • NDP + ATP NDP NTP Nucleoside DI phosphate kinase Conversion of Ribonucleotides to De-oxy Ribonucleotides: • NDP dNDP Ribonucletide reductase (RNA) (DNA) Lesch Nyhan syndrome • X-linked recessive disease • Complete deficiency of HGPRT – Hypoxanthine guanine phosphoribosyl transferase. • Increased uric acid production – pathogenesis: 1. Deficient salvage of nucleosides 2. Decreased IMP and GMP and increased PRPP- REMOVAL OF FEEDBACK INHIBITON which stimulates PRPP amido transferase – DeNovo purine synthesis Clinical features • Severe heritable form of Gout – due to increased uric acid production. • Features of Gout. • Self mutilation – head banging, biting of lips and fingers • Involuntary movements- choreoathetotic movements. • Uric acid stones. Self mutilation Adenosine deaminase deficiency • Part of SCID – severe combined immuno deficiency syndrome. • Autosomal recessive – def of enzyme Adenosine deaminase • Def leads to accumulation of deoxyadenosine which increases the concentration d-ATP. This inturn inhibits ribonucleotide reductase which is required for converting ribonucleotides to deoxyribonucleotides. Clinical features • Deficiency of both T and B lymphocytes • Leads to deficiency of both cell mediated and humoral immunity. • Prone to infections. • Bubble boy – sterile environment. • Treatment – gene therapy. • Normal URIC ACID LEVEL2-7mg/dl • HYPERURICEMIA is not GOUT !! • HYPERURICEMIA PREDISPOSES TO GOUT !! GOUT (Podagra) • Recurrent attacks of inflammatory arthritis • Metatarso- phalengeal joint of Big toe – MC • Also presents as tophi, kidneystones and urate nephropathy. • Elevation of uric acid levels – over production or under excretion of uric acid. Monosodium urate crystals • Poor solubility and hypersaturation leads to formation of needle shaped monosodium urate crystals (negatively birefringent) which are deposited in joints, tendons, and subcutaneous tissues. • crystals attracts inflammatory cells inflammation – inflammatory mediators - Causes of primary Gout 1. Decreased excretion : Defect in tubular secretion in kidneys. 2. Increased production :PRPP synthase mutation – low Km for ribose – 5- PO4 or high Vmax for PRPP production. 3. HGPRT deficiency- Lesch Nyhan syndrome Secondary GOUT • • • • • • • Lactic acidosis Von-Gierke’s disease Cancer chemotherapy Tumorlysis syndrome Hereditary Fructose intolerance Renal failure Purine rich foods. Treatment of Gout • Colchicine – inhibits migration of inflammatory cells • NSAIDS – Antiiflammatory and analgesics • Uricosuric drugs –probencid and sulfinpyrazone – CONTRAINDICATED IN RENAL GOUT • Xanthine oxidase inhibitors – Allopurinol. MCQ1 Gout is characterized by elevated uric acid concentrations in blood and urine due to a variety of metabolic abnormalities that lead to the overproduction of purine nucleotides. Allopurinol is used in the treatment of gout because this drug, and its metabolic product, alloxanthine, act as inhibitors of: • • a) Xanthine Oxidase • b) PRPP synthetase • c) Adenyl succinate synthase • d) Hypoxhantine guanine phosphoribosyl transferase • e) Nucleotides MCQ2 • Hereditary Orotic aciduria is characterized by severe anemia, growth retardation, and high levels of orotic acid excretion. It is produced by deficit of enzymes related with: • • a) synthesis of pyrimidine nucleotides • b) catabolism of pyrimidine nucleotides • c) synthesis of purine nucleotides • d) catabolism of purine nucleotides • e) synthesis of Heme • f) catabolism of Heme