Power Point Presentation - Center for Development of Human
advertisement

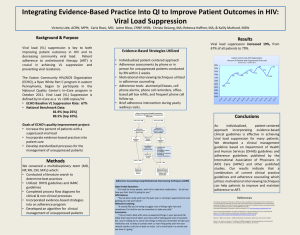
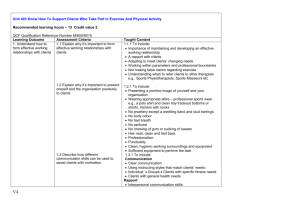
Examining Adherence Barriers in Pediatric and Adolescent HIV Patients PACT Clinic, Women and Children’s Hospital of Buffalo University at Buffalo Melannie Cummings, PharmD Student Desiree Tomilo, PharmD Student Linda Catanzaro, PharmD Assistant Professor School of Pharmacy and Pharmaceutical Sciences © 2004 CDHS, College Relations Group BSC/SUNY Research Foundation Objectives Provide an overview of HIV infection and treatment options Discuss opportunistic infections and prophylaxis Discuss medication adherence and potential barriers to adherence Discuss the health consequences of non-adherence Describe tools and methods used to improve adherence Discuss what to expect when caring for a child with HIV Describe the pediatric and adolescent patient population at the PACT Clinic, at Women’s and Children’s Hospital of Buffalo Global Estimates for adults and children end 2003 People living with HIV/AIDS New HIV infections in 2003 Deaths due to HIV/AIDS in 2003 40 million 5 million 3 million About 14,000 new HIV infections a day in 2003 Almost 2000 are children under 15 years of age About 12,000 are 15-49 years of age About 50% of these are 15 -24 years of age HIV Global Estimates1 In the year 2003 – estimated 700,000 children under 15 years old became infected mostly in sub-Saharan Africa >90% were due to mother to infant transmission 1. <AVERT.org> 3/3/04. Incidence of Children with HIV in the United States1 Most are living in inner cities poverty poor housing drugs limited access to health care and social services 1. National Institutes of Allergy and Infectious Disease <www.niaid.nih.gov> 2004. Good News in New York State 1996 - “Baby AIDS Law” mandatory HIV testing added to newborn screening program mother to infant transmission rates have decreased by 78%1 study of infants born from 19972002 1. NYS Dept. of Health. <www.health.state.ny.us/> May 2004. Methods of Transmission sexual contact contact with infected blood needle sticks unprotected administration of first aid mother to child perinatally - during delivery of the baby through breast milk Prevention of Perinatal Transmission Early identification of maternal infection goal: keep viral load <10001 to decrease risk of transmission to baby by up to 70%2 Antiretroviral prophylaxis with zidovudine during pregnancy, labor, and to newborns2 Cesarean-Section Delivery Mother’s viral load >1,000, regardless of therapy1 Counseling and advisement of infected women to use an alternative to breast milk 1. Committee on Obstetric Practice. ACOG committee opinion scheduled Cesarean delivery and the prevention of vertical transmission of HIV infection. Number 234, May 2000. International Journal of Gynaecology & Obstetrics. 2001 Jun;73(3):279-81. 2. Sperling RS, Shapiro DE, Coombs RW et al. “Maternal viral load, zidovudine treatment, and the risk of transmission of human immunodeficiency virus type 1 from mother to infant.” Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. N Eng J Med, 1996;335(22) :1621-9. Effects of HIV on the Human Body HIV attacks and weakens the immune system If the virus is not suppressed and it continues to replicate, further damage to the immune system and progression to AIDS can occur. The likelihood of developing AIDS or death within 12 months, when a child is not on antiretroviral therapy, can be as high as 51% and 30%, respectively1. 1. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. January 20, 2004. Diagnosis of HIV in Infants All newborns are tested for HIV, regardless of the mother’s status. In infants born to infected mothers, diagnostic testing should be done: before the infant is 48 hours old at 1-2 months old at 3-6 months old Six months after birth, all infected infants can be definitively diagnosed. Surrogate Markers as Predictors of Disease Progression Surrogate markers are obtained from an individual’s blood work. CD4+ T-cells cells in the immune system that are needed to fight off infection; higher CD4+ percentages indicate better immune status Surrogate Markers Viral load (HIV-RNA) measures how much virus is in the body; the lower the viral load the better indicates if medication is effective; lower viral load limits the potential for development of resistance to medications Indications for when to initiate therapy in children > 1 year of age1 Clinical Category CD4+ % HIV-RNA Recommendation AIDS OR(severe symptoms) < 15% Any value Treat Mild-Moderate Symptoms OR- Asymptomatic AND- OR15-25% >100,000 copies/mL AND>25% <100,000 copies/mL 1. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. January 20, 2004. Consider treatment May defer therapy and closely monitor surrogate markers Role of Medications Antiretroviral medications work by suppressing viral replication seen by low viral load do not completely eradicate the virus (not a cure) Choice of Antiretroviral Medication Regimens in Pediatric Patients The first regimen that is chosen has the best chance of reducing the viral load to undetectable by assay or test (<50 copies/mL). It is recommended that a regimen consist of: 2 NRTIs + 1 PI -orin children >3 years: 2 NRTIs + Efavirenz (a NNRTI) in children <3 years or who can’t swallow capsules: 2 NRTIs + Nevirapine (a NNRTI)1 1. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. January 20, 2004. Classes of Antiretroviral Medications Nucleoside Analogue Reverse Transcriptase Inhibitors (NRTIs) Nucleotide Reverse Transcriptase Inhibitors (NtRTIs) Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) Protease Inhibitors (PIs) Fusion Inhibitors- not approved for pediatrics Nucleoside Analogue Reverse Transcriptase Inhibitors (NRTIs) Mechanism of Action (MOA): block an enzyme that is needed by the virus in order to make DNA can be taken without regard to meals Adverse Effects seen with NRTIs Common side effects: nausea, vomiting, diarrhea, fatigue, weakness, headache, dizziness, loss of appetite, insomnia with the exception of fatigue, these side effects usually go away Severe side effects: pancreatitis, anemia (with AZT), hypersensitivity reaction/rash (with ABC), peripheral neuropathy (tingling and/or numbness in the extremities), liver damage NRTIs commonly used in pediatrics zidovudine, AZT (Retrovir) lamivudine, 3TC (Epivir) Available in capsules, tablets, syrup (strawberry) Available in tablets and oral solution (strawberry-banana) stavudine, d4T (Zerit) Available in capsules powder for oral suspension- once mixed, shake before use, refrigerate and discard after 30 days NRTIs didanosine, ddI (Videx) take on an empty stomach Available in chewable tablets (orange flavored)- Do not swallow tablets whole, must be chewed or crushed in water and 1 oz. apple juice; take on empty stomach; many children do not like these powder for solution- mix with 4 oz. water; once mixed, store in refrigerator; shake well before use and discard after 30d buffered powder packets for solution- mix with 4 oz. water and discard after 4 hours enteric coated capsules- must not be opened, swallow whole NRTIs Abacavir, ABC (Ziagen) Available in tablets oral solution (strawberry-banana)- may be refrigerated A life-threatening allergic reaction can occur in 5% of patients; characterized by rash or flu-like symptoms; discontinue medication, do not try to give to patient again, and call MD Combination NRTIs lamivudine+zidovudine, 3TC+ZDV (Combivir) Available in tablets: 150mg 3TC + 300 mg ZDV abacavir+lamivudine+zidovudine, ABC+3TC+ZDV (Trizivir) Available in tablets: 300mg ABC + 150mg 3TC + 300mg ZDV This drug contains abacavir do not give if patient had a previous allergic reaction to abacavir NRTIs These NRTIs do not have sufficient data to support their use in pediatrics: ddC- zalcitabine (Hivid) FTC- emtricitabine (Emtriva) TFV- tenofovir (Viread) currently being studied in pediatrics Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) MOA: block an enzyme needed by the virus in order to make DNA Side effects: rash, depression, insomnia, vivid dreams, These symptoms usually resolve within the first few weeks numerous drug interactions A single mutation can cause resistance to the entire NNRTI class. NNRTIs Efavirenz (Sustiva) Available in tablets capsules - can be opened and added to liquids or foods Take on an empty stomach and give at bedtime NNRTIs Nevirapine (Viramune) once daily for 14 days, then titrated to 2x/day increased risk of rash Available in tablets suspension - sweetened, shake before using Delaviridine (Rescriptor) Insufficient data to support use in pediatrics Protease Inhibitors (PIs) MOA: block an enzyme needed to assemble the infectious virus particles Side effects: fat maldistribution, liver damage, elevated triglycerides, diabetes These usually occur over long periods of time. numerous drug interactions PIs Nelfinavir (Viracept) Available in tablets - may be crushed and added to 3 oz. water or a small amount of food powder - may be mixed in a small amount of food, milk, formula, soy milk or formula, dietary supplements, or soft foods; refrigerate solution and discard after 6 hours Should be given with a meal or light snack. PIs Ritonavir (Norvir) children 2-16 years of age Available in soft gelatin capsules - store in refrigerator or use within 30 days if at room temperature solution - shake before use; can mix with milk, chocolate milk, Ensure and give within 1 hour of mixing; do not refrigerate PIs Amprenavir (Agenerase) children >3 years of age Available in Soft gelatin capsules Solution (grape-bubblegum-peppermint) Keep both at room temperature Do not give with a high fat meal Avoid using supplements containing vitamin E PIs Lopinavir/ritonavir (Kaletra) Children >6 months Available in capsules solution Keep both in refrigerator; if at room temperature, use within 2 months. Give with food PIs These PIs do not have sufficient data to support their use in pediatrics: Indinavir (Crixivan) Saquinavir (Fortovase) Fosamprenavir (Lexiva) Atazanavir (Reyataz) currently being studied in pediatrics Opportunistic Infections Cause of 90% of deaths in HIV infected patients Caused by common organisms Develop due to loss of cell-mediated immunity Development can be predicted by CD4+ lymphocyte levels 1. Dipiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM. Pharmacotherapy A Pathophysiologic Approach, 5 th edition. The McGraw-Hill Companies, Inc. 2002. Opportunistic Infections HAART (Highly Active Anti-Retroviral Therapy) was introduced in the United States in 1995 1 From 1996-1998 1. 2. PCP rates decreased 21% per year 2 MAC rates decreased 39.9% per year 2 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Dipiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM. Pharmacotherapy A Pathophysiologic Approach, 5th edition. The McGraw-Hill Companies, Inc. 2002. Opportunistic Infections Appropriate treatment of HIV is essential Prevention and management of opportunistic infections is still a very important part of the care of HIV infected patients 1. Dipiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM. Pharmacotherapy A Pathophysiologic Approach, 5th edition. The McGraw-Hill Companies, Inc. 2002. Opportunistic Infections Pneumocystis carinii Pneumonia (PCP) Mycobacterium avium Complex (MAC) Vaccinations Pneumococcal H. influenzae type b (Hib) Pneumocystis carinii Pneumonia (PCP) Who Should Receive PCP Prophylaxis? Infants 1-12 months old - if HIV-infected or HIVindeterminate Children 1-5 years old - with a CD4+ count <500 cells/µL or CD4+ percentage <15% Children 6-12 years old - with a CD4+ count <200 cells/µL or CD4+ percentage <15% 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Who Should Receive PCP Prophylaxis? Adolescents and Adults - with a CD4+ count <200 cells/µL or a history of orophangeal candidiasis Consider prophylaxis for adolescents and adults with a CD4+ percentage <14% or with a history of AIDS defining illness 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Recommended PCP Prophylaxis Children Trimethoprim/Sulfamethoxazole (TMP/SMZ) 150/750 mg/m2/d in 2 divided doses given by mouth three times a week on consecutive days Other options: varying doses of Trimethoprim/Sulfamethoxazole (TMP/SMZ) Dapsone Aerosolized Pentamadine Atovaquone 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Recommended PCP Prophylaxis Adolescents and Adults Trimethoprim/Sulfamethoxazole (TMP/SMZ) one double strength tablet per day Other options: varying doses of Trimethoprim/Sulfamethoxazole (TMP/SMZ) Dapsone (with or without pyrimethamine) Aerosolized Pentamadine Atovaquone 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV November 28, 2001 Discontinuation of PCP Prophylaxis Children Continue through first year of life Children with a history of PCP infection should receive lifelong prophylaxis Safety and efficacy of discontinuation has not been studied thoroughly 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Discontinuation of PCP Prophylaxis Some clinicians consider discontinuing if: a child 1-5 years old has had a CD4+ count >500 cells/µL or CD4+ percentage >15% for at least three months A child 6-12 years old has had a CD4+ count >200 cells/µL or CD4+ percentage >15% for at least three months 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Discontinuation of PCP Prophylaxis Adolescents and Adults 1. Discontinue when the CD4+ count has been >200 cells/µL for at least three months 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Infected with HIV - November 28, 2001 Persons Mycobacterium avium Complex (MAC) Who Should Receive MAC Prophylaxis? Children <1 year old: CD4+ count <750 cells/µL 1-2 years old: CD4+ count <500 cells/µL 2-6 years old: CD4+ count <75 cells/µL ≥6 years old: CD4+ count <50 cells/µL Adolescents and Adults CD4+ count <50 cells/µL 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Recommended MAC Prophylaxis 1. 2. Children Clarithromycin 7.5mg/kg (max 500mg) by mouth twice daily Azithromycin 20mg/kg (max 1200mg) by mouth every week 1 Adolescents and Adults Clarithromycin 500 mg by mouth twice daily 2 Azithromycin 1200 mg by mouth once weekly 2 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Lexi-Comp Online, 2004. Available at: http://www.crlonline.com/crlsql/servlet/crlonline Discontinuation of MAC Prophylaxis Children Safety has not been studied in children Children with a history of MAC infection should receive lifelong prophylaxis 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Discontinuation of MAC Prophylaxis Some clinicians consider discontinuing MAC prophylaxis in children if: <1 year old: CD4+ count >750 cells/µL for at least three months 1-2 years old: CD4+ count >500 cells/µL for at least three months 2-6 years old: CD4+ count >75 cells/µL for at least three months ≥6 years old: CD4+ count >50 cells/µL for at least three months 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV November 28, 2001 Discontinuation of MAC Prophylaxis Adolescents and Adults CD4+ count >100 cells/µL for at least three months 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Vaccinations Children Should receive all of the typical childhood vaccines <5 years old: H. influenzae type b (Hib) and pneumococcal conjugate vaccine >2 years old: should also receive the 23-valent polysaccharide pneumococcal vaccine Revaccincate after 3-5 years if child ≤10 years old and after 5 years if >10 years old 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Vaccinations Adolescents and Adults CD4+ count ≥200 cells/µL: single dose of 23-valent polysaccharide pneumococcal vaccine (if they have not received it in the past five years) Pneumococcal vaccine can be considered in patients with a CD4+ count <200 cells/µL but there is no proof of efficacy H. influenzae type b (Hib) is not recommended 1. 2001 USPHS/IDSA Guidelines for the Prevention of Opportunistic Infections in Persons Infected with HIV - November 28, 2001 Medication Adherence > 95% adherence is needed to adequately suppress viral replication 1. Esch LD. “Issues in Human Immunodeficiency Virus (HIV) Pharmacotherapy Practice. The Emerging Role of Pharmacotherapy Specialists in Enhancing Antiretroviral Success.” J Inform Pharmacother 2001;4:306-316. Potential Barriers to Adherence Pill burden Drug use/alcohol abuse Depression Lack of education1 Unwillingness to disclose HIV status2 Unstable environment 2 Side effects Lack of palatability of medications2 1. Esch LD. “Issues in Human Immunodeficiency Virus (HIV) Pharmacotherapy Practice. The Emerging Role of Pharmacotherapy Specialists in Enhancing Antiretroviral Success.” J Inform Pharmacother 2001;4:306-316. 2. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infections-January 20, 2004 Adherence Pediatric adherence is of special concern because the status of the caregiver as well as the patient has to be taken into account Consequences of poor adherence Virologic failure-incomplete (or lack of) HIVRNA response Incomplete virologic response Virologic rebound 1. Guidelines for the Use of antiretroviral agents in HIV Infected Adults and Adolescents – March 23, 2004 Consequences of poor adherence 1. Development of resistance inadequate levels of medication to suppress viral replication selective pressure-resistant virus is able to replicate and repopulate patient1 Regimen changes decreased medication choices for the future Luber AD. “Pharmacotherapy of Human Immunodeficiency Virus Infection”. In: Koda-Kimble M, Young LY, Kradjan WA, Guglielmo BJ, editors. Applied Therapuetics. The Clinical Use of Drugs. Seventh Edition. New York: Lippincott Williams and Wilkins; 2001. Consequences of poor adherence Resistance and virologic failure increase the risk of comorbidities and death High HIV-RNA levels and low CD4+ lymphocyte counts - increased risk of progression to AIDS (see Table 1) 1. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infections-January 20, 2004 Potential Adherence Interventions Pill boxes Calendars Alarm watches Home visits Refill checks Phone calls Adherences visits/clinic appointments See table 2 1. Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infections-January 20, 2004 Education of foster parents of HIV+ children Universal precautions Avoid contact with child’s blood Use caution if child is vomiting or has diarrhea Guidelines: NIH (http://www.nih.gov/) CDC (http://www.cdc.gov/) Disease education Education on medication regimens PACT Clinic Baseline Characteristics (Total Number of Patients=24) CD4+ T Cell Percentage No Suppression (>25%) Moderate Suppression (15-24%) Severe Suppression (<15%) Unknown <12 months 0 0 0 0 1–5 years old 2 2 0 0 6–12 years old 7 2 1 0 >12 years old 5 2 2 1 Total 14 6 3 1 CD4+ T Cell Percentage Immune Suppression in all Children at the PACT Clinic Severe Unknown, 1, 4% Suppression No Suppression (>25%) (<15%), 3, 13% Moderat e Suppression (1524%) Severe Suppression (<15%) Moderat e Suppression (15- No Suppression 24%), 6, 25% (>25%), 14, 58% Unknown CD4+ T Cell Percentage Immune Suppression in Children 1-5 years old Severe Suppression (<15%), 0, 0% Unknown, 0, 0% No Suppression (>25%) Moderate Suppression (15-24%) Moderate Suppression (15-24%), 2, 50% No Suppression (>25%), 2, 50% Severe Suppression (<15%) Unknown CD4+ T Cell Percentage Immune Suppression in Children 612 years old Severe Suppression (<15%), 1, 10% Unknown, 0, 0% Moderat e No Suppression (>25%) Moderat e Suppression (1524%) Suppression (1524%), 2, 20% Severe Suppression (<15%) No Suppression (>25%), 7, 70% Unknown CD4+ T Cell Percentage Immune Suppression in Children >12 years old No Suppression (>25%) Unknown, 1, 10% Severe Moderat e Suppression (1524%) Suppression (<15%), 2, 20% No Suppression (>25%), 5, 50% Severe Suppression (<15%) Unknown Moderat e Suppression (1524%), 2, 20% Living Situations Of the 24 patients: 79.2% (19) are living with a biological relative 12.5% (3) are in non-kinship foster placements 8.3% (2) are living alone History of Depression in Patients and Caregivers History of Depression Child Only Caregiver Only Both 8 4 3 No Documented History 8 Unknown 1 History of Substance Abuse in Patient and Caregivers History of Substance Abuse Child Only Caregiver Only Both No Documented History Unknown 2 10 0 11 1 Adherence Good Adherence = 0-2 missed doses/month Fair Adherence = 3-5 missed doses/month Poor Adherence = >5 missed doses/month Patient Reported Medication Adherence in all Children at the PACT Clinic Good Adherence 12 Fair Adherence No ART 3 1 Total N=24 Poor Adherence 2 Unknown 6 Patient Reported Medication Adherence in Children Ages 1-5 years old Good adherence 1 Fair Adherence No ART 1 1-5 years old 0 Poor adherence 0 Unknown 2 Patient Reported Medication Adherence in Children Ages 6-12 years old Good Adherence 5 Fair Adherence No ART 2 6-12 years old 0 Poor Adherence 1 Unknown 2 Patient Reported Medication Adherence in Children > 12 years old Good Adherence 6 Fair Adherence No ART 0 > 12 years old 1 Poor Adherence 1 Unknown 2 Reasons for Missed Doses away from home 2 (14%) 4 (30%) 1 (7%) side effects 1 (7%) ran out confidentiality 1 (7%) 2 (14%) fell asleep 3 (21%) substance use other Reasons for Missed Doses Other commons reasons for missed doses include: forgetting pill burden At baseline no one in this population reported these reasons. Medication Administration Unknown-2 (8%) No ART-3 (13%) Both-9 (37%) Patient-3 (13%) Patient Caregiver Caregiver-7 (29%) Both No ART Unknown Patient Reported Adherence vs. Medication Administration Good Adherence (0-2 missed doses/month) Patient, 2, 17% Patient Caregiver Both, 6, 50% Both Caregiver, 4, 33% Patient Reported Adherence vs. Medication Administration Fair Adherence (3-5 missed doses/month) Caregiver, 0, 0% Patient, 0, 0% Patient Caregiver Both Both, 1, 100% Patient Reported Adherence vs. Medication Administration Poor Adherence (>5 missed doses/month) Patient, 1, 50% Both,1, 50% Patient Caregiver Both Caregiver, 0, 0% Patient Reported Adherence vs. Medication Administration • 3 patients were not on antiretroviral therapy • 6 patients were unknown Association between fair or poor adherence and depression and/or substance abuse Fair Adherence Patient 1: Patient-depression, Caregiver-no documented depression No documented substance abuse in patient or caregiver Patient and caregiver are involved in medication administration Association between fair or poor adherence and depression and/or substance abuse Poor adherence Patient 1: Patient-Depression, Caregiver-no documented depression Patient-Substance abuse, Caregiver-no documented substance abuse Patient is in charge of medication administration Association between fair or poor adherence and depression and/or substance abuse Poor adherence Patient 2: Patient-Depression, Caregiver-Depression Patient-no documented substance abuse, Caregiver-substance abuse Patient and caregiver are in charge of medication administration Conclusions Adherence appears to be better when both the caregiver and the patient are involved in medication administration Substance abuse and depression in the patient and/or the caregiver appears to negatively effect adherence Due to the small patient population of the PACT Clinic, the assessment of the baseline characteristics should not be extrapolated to the general population PACT Clinic Follow-up Interventions During the appointed period (September 2003-May 2004) one patient was added, making our total number of patients 25 Methods: Standard of Care Bi-weekly or as needed adherence appointments Patient interviews using follow-up questionnaires Monthly case conferences with PACT nurses Pharmacist and RN available by pager for questions Adherence interventions Pill boxes Home visits and refill checks by adherence nurse Medication administration schedule PACT Clinic Interventions Of the 25 patients: 96% (24) were seen during the appointed time Of the 24 patients seen: 12.5% (Cases 1,2, and 3) required interventions Treatment of depression Intensive follow-up (including home visits and refill checks) Supplying adherence tools Pillboxes Case 1 History 13 year old HIV+ male presented to clinic in January Patient had previously seen a psychiatrist and was diagnosed with major depression. An antidepressant was prescribed. Based on patient’s CD4+ count, PCP prophylaxis was also previously prescribed After questioning it was determined that the patient was non-adherent to both medications Currently not on ART and was being deferred until improvement was seen in depression and adherence Case 1 Intervention Pharmacist and patient came to written agreement stating that the patient would be adherent to both his medications Results At two week and six week follow-up visits, patient demonstrated significant improvements in mood and adherence Patient showed interest in helping to choose an ART regimen Currently waiting for most recent surrogate markers to evaluate need for starting ART Case 2 History 13 year old HIV+ male presented to clinic reporting excellent adherence Surrogate markers suggested current regimen was failing and a change was considered Intervention Adherence nurse made a home visit and discovered multiple vials of all of his antiretroviral medications Adherence was inaccurately reported by the patient Case 2 Results Change in ART deferred until patient demonstrates willingness to adhere to current regimen Home visits and follow-up phone calls are still being used to evaluate adherence Case 3 History 18 year old HIV+ female Unstable home environment, was living with sister Friends over every night Drinking alcohol frequently Patient reported poor adherence for various reasons Alcohol, confidentiality issues, oversleeping Case 3 Intervention Patient was given a pillbox and counseled to fill it at the beginning of each week It was suggested to keep the pillbox in her dresser drawer so that she could take her medications privately Good adherence was encouraged and consequences of poor adherence were discussed Results Currently waiting for follow-up visit to assess adherence Case 4 The following case is an example of the impact the home environment and the caregiver can have on a child’s HIV status Case 4 History Five year old HIV+ male with increasingly elevated viral load (as high as 300,000 copies/mL), which suggested non-adherence to regimen Living with mother during this period Unstable home environment Mother not giving patient medications Case 4 Child went to live with father Father took an interest in caring for child’s HIV Attended adherence visits at PACT Clinic Was educated on patient’s medications and the importance of adherence At follow-up appointments, reported good adherence Viral load has dramatically decreased to goal of undetectable (<50 copies/mL) Overall Conclusions Adherence barriers include being away from home, sleeping through doses, side effects, forgetting, running out of medication and confidentiality Depression and substance abuse may be significant barriers to adherence Pharmacy-based interventions potentially improve adherence Overall Conclusions Basic education of potential caregivers regarding the disease itself and the medications used is crucial. Universal precautions Adherence education Comprehension of regimen Involvement of primary healthcare provider Caring for a child with HIV can be challenging, but with the support of members of the healthcare team and social services, a caregiver can provide everything that is needed for the child to live a normal, healthy life. Questions?