Nephrolithiasis for the Internist
advertisement

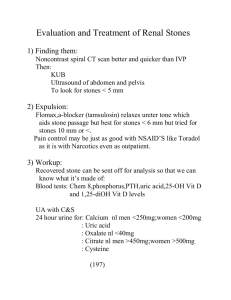
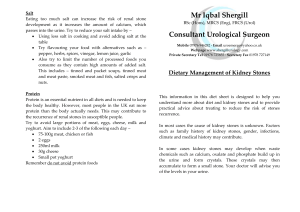
Nephrolithiasis for the Internist Rajiv Kumar Divisions of Nephrology and Endocrinology Departments of Medicine, Biochemistry and Molecular Biology Mayo Clinic, Rochester Meira and Shaul G. Massry Visiting Professorship Dr. Massry has had an exceptionally distinguished career. He has received honorary doctorates from universities across Europe and has been the recipient of numerous awards from universities and societies throughout the world. Dr. Massry was the Editor-inChief of the American Journal of Nephrology, and of Mineral and Electrolyte Metabolism. He is the coEditor of the Textbook of Nephrology. Shaul G. Massry, M.D. , Professor Emeritus of Medicine and Physiology & Biophysics at the Keck School of Medicine, University of Southern California and Emeritus Chief of the Division of Nephrology (1974-2000). Dr. Massry is a past President of the National Kidney Foundation, American Society of Renal Biochemistry and Metabolism, International Society of Nutrition and Metabolism in Renal Diseases, International Society of Uremia Research and Toxicity, and International Association of the History of Nephrology. Dr. Massry has been a frequent guest speaker at national and international meetings and a visiting professor at many universities across the globe. He has published over 600 scientific papers, 111 chapters in books and edited 32 books. Mayo Clinic Rochester Disclosures • None Objectives • Familiarize you with recent trends in kidney stone prevalence • Discuss the pathogenesis of kidney stones • Review diagnostic tests required to assess kidney stones • Review medical therapeutic interventions which will reduce stone recurrence Case 1 • You are asked to evaluate an 85 yo female with a history of Crohn's disease with multiple ileal resections and an ileal transverse colostomy. 122 cm of the ileum have been resected. At the present time the patient does not have any diarrhea, but she has had frequent loose stools in the past. • She was evaluated in the ED for left-sided ureteric colic three weeks ago. She underwent a cystoscopy, left retrograde pyelogram, left flexible ureteroscopy, laser lithotripsy and basket extraction of stones from her left ureter. A ureteral stent was placed. Since then, she has been asymptomatic. Chemical analysis of her stones has been performed. • The patient does take vitamin D and calcium for treatment of osteoporosis, but she has not been hypercalcemic or hypercalciuric per report. There is also a history of vitamin C use. Oral fluid intake is low. Case 1 • VITAL SIGNS. Height 15.0 cm; weight 58.0 kg; BMI 24.2 kg/m2; temp 36.8 C; BP 99/55 mmHg; P 56 bpm, regular. • PHYSICAL EXAMINATION. Negative except for colostomy and multiple abdominal surgical scars. Case 1 contd. Stone analysis is likely to reveal: • • • • • Ca oxalate monohydrate and Ca oxalate dihydrate 100% uric acid Struvite (Ca-Mg-NH4) stone Brushite (Ca phosphate) Hydroxyapaptite Case 1 contd. You would recommend treatment with which of the following? • • • • • A high fluid intake – 2.5 L/day or more A low oxalate diet Calcium carbonate 1gm po tid All of the above None of the above Case 2 • You are asked to evaluate an 80 yo female with a history of recurrent kidney stones. Recently, she underwent a cystoscopy and laser lithotripsy for a L ureteral stone. Two and four years prior to seeing you, she had extracorporeal shock wave lithotripsy for stones in the left and right renal pelvis, respectively. • With respect to risk factors for stones, she has a two-year history of intermittent hypercalcemia with serum Ca values as high as 11.1 mg/dL and a non-suppressed PTH. She also has a history of gout dating back twenty years, for which she takes colchicine when she has an acute attack, and for which she is on chronic allopurinol. She has not had any recent gouty attacks. With respect to medications, she takes no vitamin D, calcium, or vitamin C. She has taken prednisone in the past for a short period of time. Case 2 • There is no history of ulcerative colitis, regional ileitis, malabsorption, or diarrhea. • Her diet does not reveal a high oxalate or purine precursor intake. She is on treatment at the present time with Urocit-K 20 mEq PO t.i.d. as well as allopurinol. Case 2 contd. • VITAL SIGNS: Height: 167.3 cm. Weight: 97.60 kg. BSA(G): 2.16 M2. BMI: 34.870 KG/M2. Temperature: 36.8 °C. Blood Pressure: 141/68 mmHg. Pulse Rate: 78/minute, regular. PHYSICAL EXAMINATION: There was a left parotid mass approximately 3 cm in diameter. No nodes were felt. No other neck masses noted. The rest of the exam was normal. Labs: PTH 120 Case 2 contd. Case 2 contd. Chest x-ray; 2 views: Prominent fat pad right cardiophrenic angle. Slight scarring or atelectasis in the right middle lobe. Calcified granuloma left lower lobe. Mild thoracolumbar curve. ECG normal. Case 2 contd. ACE – 71 U/L (nl 8-53); PTH-RP < 0.2 pmol/L (nl - < 2.0 pmol/L); whole molecule PTH – 120 pg/mL (nl 5-65 pg/mL); serum monoclonal protein by immunofixation small IgG l. Parathyroid scan performed with technetium 99m sestamibi and I-123 including SPECT imaging. Subtraction imaging showed a discordant area of increased sestimibi uptake test posterior to the inferior pole of the right thyroid lobe consistent with an abnormal parathyroid gland. In addition there was increased sestamibi localization posterior to the left inferior lobe of the thyroid that is less certain but worrisome for a second abnormal parathyroid gland. No additional foci of discordant sestimibi uptake. Ultrasound of the neck demonstrated a 6 mm by 8mm x 9 mm hypoechoic nodule posterior to the lower right thyroid lobe which could be a parathyroid adenoma. There was also a 6 mm x 7 mm hypoechoic nodule in the posterior portion of the inferior left thyroid lobe which is likely a benign thyroid nodule. Small area of calcification in the mid left thyroid lobe which was not associated with a focal nodule. No cervical adenopathy. Case 2 contd. • An endocrine surgeon performed a two gland parathyroidectomy with resolution of hypercalcemia and subsequent stone activity. Intra-operative Neck Vein PTH, pg/mL Baseline PTH 10 minutes 15 minutes 254 48 40 Post-op Ca 9.0 mg/dL. Pathology of parathyroid glands: A. Parathyroid, left superior, parathyroidectomy: Normocellular parathyroid gland (50.0 milligrams). B. Parathyroid, left inferior, biopsy: Normocellular parathyroid tissue. C. Parathyroid, right superior, parathyroidectomy: Hypercellular parathyroid (230.0 milligrams). D. Parathyroid, right inferior, parathyroidectomy: Hypercellular parathyroid (240.0 milligrams). Case 2 contd. Stone analysis is likely to reveal: • • • • • Ca oxalate monohydrate and Ca oxalate dihydrate 100% uric acid Struvite (Ca-Mg-NH4) stone Brushite (Ca phosphate) Hydroxyapaptite Nephrolithiasis is Common, Costly and Preventable • Nephrolithiasis is a common disorder (yearly incidence of nephrolithiasis in the US is ~ 0.5%) that is associated with considerable morbidity and economic cost. • In the USA the economic cost is estimated at between $2.1 and $5.3 billion billion per year, with the vast majority ($4.5 billion) attributed to direct medical/urological costs. • Strategies to accurately diagnose the type of stones and institute measures to prevent stone recurrence will have a great impact on reducing costs associated with this illness. The Prevalence of Nephrolithiasis has Increased • The prevalence of nephrolithiasis in the United States and Europe has increased in the two decades between 1970-1990 from about 3% to about 5%. Percent Prevalence of History of Kidney Stones 1976-1980 and 1988-1994 Statmatelou, Kidney International 63: 2003 Incidence of Kidney Stones 1950-1974 and 1970-2000 in Rochester, MN Lieske et al, Kidney International (2006) 69, 760–764. Why the “Stone Boom”? • Better diagnostic tools • Life style • Dietary habits • Obesity Life Style Risk Factors for Stone Formation • Low water intake : low volume and infrequent intake increased urine supersaturation • Consumption of food rich in calories and salt, and low in fiber and alkali hypercalciuria, deficiency in urinary stone inhibitors • Sedentary lifestyle obesity Stone Episodes and Obesity Siener R, Obesity Res, 12: 106-113, 2004 BMI and Relative Risk of Symptomatic Stones Taylor E, JAMA, 293(4), 455-462 2005 Urine Composition with Obesity • Decreased Urine pH • Elevated urinary excretion of Sodium Calcium (men > women) Phosphate, sulfate Uric acid Oxalate (women) Siener R, Obesity Research 12:106-113, 2004 Nephrolithiasis is Associated with an Increase in the Incidence of CKD Rule et al, Clin J Am Soc Nephrol, 6:2069-2075, 2011. Nephrolithiasis is Associated with an Increased Incidence of Myocardial Infarction Rule et al, J Am Soc Nephrol. 2010 Oct;21(10):1641-4. Composition of Kidney Stones Percentage of stones Characteristics Calcium oxalate monohydrate 40-60% Radio-opaque, wellcircumscribed Calcium oxalate dihydrate 40 to 60% Radio-opaque Calcium phosphate, apatite, Ca10[PO4]6[OH]2 20-60% Radio-opaque Calcium phosphate, Brushite, CaHPO4.2H2O 2-4% Radio-opaque Uric Acid 5-10% Radiolucent Struvite (magnesium ammonium phosphate) 5-15% Can be staghorn Cystine 1.0-2.5% Mildly radio-opaque Ammonium urate 0.5-1 .0% Crystal type Mixed stones Calcium oxalate-phosphate 35-40% Radio-opaque Mixed uric acid-calcium oxalate 5% Radio-opaque Herring et al, J. Urol, 88:545, 1962; Mandel et al, J. Urol, 142-1513, 1989; Mandel et al, J. Urol, 142:1516,1989 Pathophysiology of Stones A number of metabolic abnormalities are associated with the occurrence of renal calculi. • Increased urinary concentration of solutes due to a reduction in fluid intake and urine volume. • Metabolic abnormalities: Hypercalciuria, hypocitraturia, hyperoxaluria, hyperuricosuria, and altered urinary pH. Individuals at Increased Risk for Stone Formation • • • • • Hypercalciuria Hypocitraturia Hyperparathyroidism Hyperoxaluria GI diseases (Colitis, Crohn’s, malabsorption) • Surgery for obesity • Family History • Gout/hyperuricosuria/ Uric acid • Infected stones • Genetically determined •Cystinuria •Primary Hyperoxaluria •RTA Type I •2,8 Dihydroxyadenine •Xanthine Pathophysiology of Renal Stones Cause Pathophysiology Stone Composition Clinical Clues All Stones Low urine volume (raises concentration of solutes) Reduced intake or increased loss of water Renal water conservation All stones Urine volume less than 1 L per day and osmolality greater than 600 mOsm/Kg Absorptive hypercalciuria Increased absorption in intestine Calcium oxalate or calcium phosphate Urine Ca >6 mmol/liter (240 mg) per day Renal leak Loss of Ca in via kidney Urine Ca >6 mmol/liter (240 mg) per day HPT Increased absorption in the intestine and increased bone resorption High PTH concentrations and high 1, 25(OH)2D concentrations. Immobilization Increased bone resorption High U Ca Excess sodium in diet Sodium induced hypercalciuria Increased urine Na Excess protein or acid in diet Protein induced bone loss and renal leak Urine NH4 increased, high urine sulfate, low urine pH Range of monogenic disorders Bone loss, gut hyperabsorption and various combinations Calcium stones Hypercalciuria (raises saturation of calcium salts) Pathophysiology of Renal Stones Cause Pathophysiology Stone Composition Clinical Clues Calcium stones Hypocitraturia (increases urinary ionized Ca, reduces inhibitor activity against Ca salts) Renal tubular acidosis (distal type) Abnormal renal defense of acid-base balance Calcium phosphate Urine citrate concentrations less than 1.7 mmol/day. High urine pH High acid load (absence of detectable acidemia) Physiological hypocitraturia Calcium phosphate and calcium oxalate Urine citrate concentrations less than 1.7 mmol/day. High urine pH Hyperoxaluria (raises saturation of calcium oxalate) Hyperuricosuria (Na urate precipitation causes nidation of Ca salts) Excess of dietary oxalate Increased delivery of luminal oxalate Calcium oxalate Urine oxalate greater than 0.4 mmol/day Bowel disease (malabsorption, gastric bypass procedures) Reduced formation of luminal/intestinal Caoxalate complexes Calcium oxalate Urine oxalate greater than 0.4 mmol/day Increased endogenous production of oxalate Primary hyperoxaluria, type I and 2 High purine intake High purine intake Raised production & excretion of sodium urate Urinary uric acid excretion of greater than 600 mg/day Gout, Myeloproliferative disease, enzymatic defect, uricosuric drugs, renal leak Increased excretion of uric acid Hyperuricosuria, serum uric acid may be decreased Pathophysiology of Renal Stones Cause Pathophysiology Stone Composition Clinical Clues Uric acid stones Low urine pH or hyperuricosuria High acid load, metabolic syndrome, other causes of hyperuricosuria Urate salts are converted to uric acid which is insoluble and low urinary pH Uric acid Low urine pH, less than 5.5 Congenital mutations of di-basic amino acid transportersubunits Increased urinary cystine and other of basic amino acids Cystine Urine cystine greater than 150 μmol/mmol creatinine Urea-splitting organisms Production of ammonium and bicarbonate ions from urea Magnesium ammonium phosphate, carbonate apatite High urinary pH, pyuria, positive cultures for organism producing urease Cystine stones Cystinuria Infection-related stones Urinary tract infection Kidney Stone Management Recognize Risks Manage risks Monitor Evaluation of the First Stone First Stone Episode Diet Fluid 3-6 month follow-up Determine Metabolic Activity Dual Energy CT Urinalysis Urine chemistries No growth Monitor every 1-2 years Metabolic activity Treatment options Chemical Evaluation of Stones • Serum •Ca, Pi •PTH •Vitamin D Metabolites •Uric Acid •Na, K, Cl, HCO3 • Urine •pH •Sediment •Osmolality •Gram’s stain •Culture • 24hr urinary profile •Volume •Calcium •Citrate •Oxalate •Phosphorus •Sodium •Magnesium •Urinary supersaturation • Radiological Studies •Dual energy CT •CT Urogram Renal Stone Characterization Using DECT Uric acid calculus Non-uric acid/ Calcium calculus Hartman et al. Radiologic Clinics of North America 2012 vol:50 iss:2 pg:191 -205 Renal Stone Characterization Using DECT Ca oxalate calculus Hydroxyapaptite calculus Liu et al, Academic Radiology, 20, 1521–1525, 2013 General Measures for the Treatment of Renal Stones: Lifestyle changes These interventions are applicable to all stones • • • • BMI 18-25 kg/m2 Balancing excess fluid loss Dietary changes Physical activity General Measures: Dietary Prevention of Stone Formation These interventions are applicable to all stones • Fluid • • • • Total intake: 2.5-3.0 L/day Urine output: 2.0-2.5 L/day Intake balanced throughout the day Neutral beverages General Measures: Dietary Prevention of Stone Formation These interventions are applicable to all stones • Limit animal protein: 0.8-1.0 grams/Kg/day • Limit sugar and fat content • Limit sodium: 4-5 grams/day Calcium: 1,000• • • 1,200 mg/day (not with absorptive hypercalciuria) Limit oxalate intake Rich in vegetable fiber Rich in alkaline potassium General Measures: Restriction of Dietary Animal Protein and Sodium A high intake of animal proteins/purine precursors • • • • Increases urinary uric acid excretion Decreases urinary pH Decreases urinary citrate excretion Increases urinary calcium excretion A high intake of sodium chloride • High salt diet – increases urinary calcium excretion Dietary Animal Proteins and Salt: Risks for Stone Formation Kok D at al. J Clin Endocrinol Metab. 71:661. 1990 A High Calcium Intake is Associated with Reduced Urinary Oxalate Excretion Von Unruh G, et al, JASN 15(6), 1567-73, 2004 Specific Measures for the Treatment of Nephrolithiasis Lifestyle or Dietary Modification Pharmacological Treatment Low urine volume Increase fluid intake to 2.5-3 liters per day Increased Fluid Intake Hypercalciuria Sodium moderation less than 150 mmol per 24 hours Hydrochlorothiazide or indapamide + potassium alkali (potassium citrate 5-10 mEq p.o. t.i.d.) Protein moderation Hyperoxaluria Restriction of dietary oxalate Avoidance of calcium restriction Calcium supplementation in malabsorption syndrome or following bypass surgery Low-fat intake in malabsorption syndrome Pyridoxine for primary hyperoxaluria; liver kidney transplantation Specific Measures for the Treatment of Nephrolithiasis Lifestyle or Dietary Modification Hyperuricosuria Purine restriction Pharmacological Treatment Potassium citrate, other alkalinizing agents such as Bicitra Allopurinol Low urinary pH Protein restriction Potassium citrate Cystinuria High fluid intake Potassium citrate, Dpenicillamine, bmercaptopropionyl glycine Urinary Tract Infection Antibiotics Specific Measures For Calcium Oxalate Stones • • • • • Assessment of Risk factors Hypercalciuria, Hyperoxaluria, Hyperuricosuria, Hypocitraturia Low urine volume Diet: Low fluids, High salt, High protein, High sugar Family History Sex Measures Which Decrease the Risk of Recurrent Calcium Oxalate Stone Disease • • • • Low animal protein diet Low salt diet Increased fluids 2.5-3 L/day Normal Ca intake (1 g/day) A High Calcium Intake is Associated with Reduced Urinary Oxalate Excretion Von Unruh G, et al, JASN 15(6), 1567-73, 2004 Management of Calcium Oxalate Stones: Urinary Profiles, Risks and Interventions • Hypercalciuria – • Hydrochlorothiazide 25-50 mg/d • Indapamide 1.25 mg/d • Chlorthalidone 50 mg/d • Potassium citrate 5-10 mEq p.o. t.i.d. • Hypocitraturia – • Lower dietary animal protein • Potassium citrate 5-10 mEq p.o. t.i.d. Management of Calcium Oxalate Stones: Urinary Profiles, Risks and Interventions • Hyperoxaluria – • Calcium 500 mg/day with meals • Magnesium 200 - 400 mg/day • Hyperuricosuria – • Potassium citrate 5-10 mEq p.o. t.i.d. • Allopurinol 100 mg/day • Hypomagnesiuria – • Magnesium 200 - 400 mg/day Nephrolithiasis and Hyperoxaluria are Complications of Bariatric Surgery • Although there is a decrease in overall mortality and an improvement in lipid and carbohydrate metabolism in patients after RYGB surgery, the incidence of nephrolithiasis and hyperoxaluria increases post-RYGB surgery. • In a recent study of 4,639 RYGB patients who had undergone bariatric surgery and 4,639 obese control patients, Matlaga et al noted that 7.65% (355 of 4,639) of RYGB patients developed urolithiasis compared to 4.63% (215 of 4,639) of the obese control patients in the control group (Matlaga et al J. Urol, 2009). Kidney Stones Associated with Malabsorption and Gastric Bypass Surgery: Hyperoxaluric Stone Disease • Increased oxalate absorption from the colon • Excess free fatty acids – fat malabsorption • Bind calcium and magnesium • Leave free oxalate to be absorbed • Fatty acids and bile salts increase colonic oxalate absorption Kidney Stones Associated with Malabsorption and Gastric Bypass Surgery: Hyperoxaluric Stone Disease • Increase in Urinary supersaturation • Decreased water absorption – low urine volumes • Decreased absorption of crystallization inhibitors: • Magnesium, phosphate, pyrophosphate Kidney Stones Associated with Malabsorption and Gastric Bypass Surgery: Hyperoxaluric Stone Disease • Urinary Profile •Hypocalciuria •Hypomagnesiuria •Hypocitraturia •Hyperoxaluria •Low urine volumes •Acidic urine • Treatment •Correct underlying malabsorption •Dietary calcium •Magnesium sup. •Citrate •Low oxalate diet •Increase fluids •Decrease dietary fat •Cholestyramine Kidney Stones Associated with Bowel Disease: Uric Acid Stones • Etiology: low urine output and acidic urine • Colectomy with ileostomy – loss of fluid and alkali • Treatment • Alkalinize the urine • Fluids • Allopurinol Stones Associated with an Acidic Urine: Uric Acid Stones • 5-10% of all stones • With gout, 25% form uric acid stones • Etiology: • Low urine volume • Acidic urine • Chronic diarrhea – colectomy and ileostomy • Excess protein intake Stones Associated with an Acidic Urine: Uric Acid Stones • Treatment: dissolve and prevent • Increase fluid intake and decrease protein intake • Alkalinize the urine – citrate • Allopurinol Stones with an Acidic Urine: Cystine Stones • 1% of Kidney stones formers • Autosomal recessive : homozygotes – stones • Defect in intestinal and renal absorption of cystine, ornithine, lysine, and arginine (COLA) • Diagnosis: • Crystalluria on UA – hexagonal • Cystinuria ( 400mg/day) • Family History Stones with an Acidic Urine Cystine Stones • Treatment • Alkalinize urine to > 7.0 • Chelators: tiopronin or penicillamine (+ pyridoxine) Stones Associated with an Alkaline Urine :Calcium Phosphate Stones • RTA type I • Hyperparathyroidism • Use of absorbable alkali (Tums, Rolaids, AlkaSeltzer) • Medullary Sponge Kidney Stones Associated with an Alkaline Urine: RTA Type I • Hyperchloremic Hyperkalemic Metabolic Acidosis • Nephrocalcinosis • Urinary Profile • Hypercalciuria • Hypocitraturia • Urine pH always > 5.3 Stones Associated with an Alkaline Urine: RTA Type I • Treatment • High fluid intake • Correct acidosis: K citrate Stones Associated with an Alkaline Urine: Struvite Stones • Magnesium ammonium phosphate stones • All are infected Proteus, other gram-negative organisms • 10% of all kidney stones / 50% are bilateral • Urine Profile : pH 8.0 • Treatment: • Preoperative antibiotics • Surgical removal of all stone material • Post-op bacterialcidal antibiotics for 6-12 months Hyperparathyroidism and Kidney Stones The association is well-recognized – “stone, bones, groans” etc. The association first recognized in the case of Captain Martell by Dr. Eugene F. DuBois in 1926. Captain Martell had become disabled by demineralization of the skeleton in association with hypercalcemia over many years. He had several episodes of flank pain, kidney calcification and stones. He was extensively studied at the MGH and eventually, a parathyroid adenoma was removed from the mediastinum at his seventh operation in 1932 with correction of his serum calcium. Interestingly, in 1925 in Europe, Felix Mandl, had removed a parathyroid tumor from a patient with kidney stones and a bony disorder, with marked clinical improvement. Hyperparathyroidism and Nephrolithiasis • Only 15-20% of patients with HPT develop stones. • The reason for this might be that patients with stones have a concomitant increase in their 1,25(OH)2D concentrations and increase in intestinal Ca absorption. Broadus et al , N Engl J Med 1980; 302:421-426. Treatment of Stone with HPT • Identify aberrant gland • Parathroidectomy Primary Hyperoxaluria Oxalate Metabolism •Oxalate is poorly absorbed from the alimentary tract. About 10-20 percent of the oxalate excreted in the urine is dietary in origin, the vast majority being endogenously derived. •About 40 percent of oxalate production appears to be derived from glycine metabolism. •Most oxalate precursors are metabolized via glyoxylate and/or glycolate the oxidation of which is the main regulatory step in the metabolism of carbohydrates to oxalate. Metabolism of Oxalate Aronson PS, Kidney International 2006 Oxalate Metabolism C. J. Danpure •PH1 is caused by a functional deficiency of the liver-specific peroxisomal enzyme alanine:glyoxylate aminotransferase (AGT) •PH2 by a deficiency of the cytosolic enzyme glyoxylate reductase (GR) and hydroxypyruvate reductase (HPR). •One-third of PH1 patients have significant levels of AGT catalytic activity due to a unique intracellular protein trafficking defects in which AGT is erroneously localized to the mitochondria. Treatment Stones and PH • Pyridoxine • Hepatic or hepatic/renal transplantation Surgical Therapy • Obstruction • Persistent severe hematuria • Persistent metabolic activity despite maximal medical therapy Case 1 • Patient with long standing Crohn’s disease and an intact colon. Case 1 contd. Stone analysis is likely to reveal: • • • • • Ca oxalate monohydrate and Ca oxalate dihydrate 100% uric acid Struvite (Ca-Mg-NH4) stone Brushite (Ca phosphate) Hydroxyapaptite Case 1 contd. On a 24 hour urine you would expect to see which of the following: • • • • • • Hyperoxaluria Hyper-uricosuria Hypercalciuria Hypo-citraturia All of the above None of the above Case 1 contd. You would recommend treatment with: • • • • • A high fluid intake – 2.5 L/day or more A low oxalate diet Calcium carbonate 1gm po bid or tid All of the above None of the above Case 2 • Patient with primary HPT Case 2 contd. Stone analysis is likely to reveal: • • • • • Ca oxalate monohydrate and Ca oxalate dihydrate 100% uric acid Struvite (Ca-Mg-NH4) stone Brushite (Ca phosphate) Hydroxyapaptite Summary • Nephrolithiasis is increasing in frequency • Metabolic abnormalities can and should be identified in the urine and serum to guide therapy • A treatment program can be designed based on findings • Serial follow-up is necessary