ashrafi
advertisement

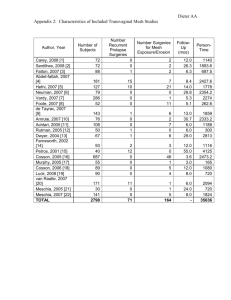
*Utrine Prolapse Vaginal Sugeries Maryam Ashrafi * ratio surgery for prolapse vs incontinence: 2:1 * prevalence of 31% in women aged 29-59 yrs * 20% of women on gynecology waiting lists * 11% lifetime risk of at least one operation * re-operation in 30% of cases * Principles of Pelvic Reconstructive Surgery * Restoration of pelvic structures to normal anatomical relationship * Restore and maintain urinary &/or fecal continence * Maintain coital function * Correct co-existing pelvic pathology * Obtain a durable result * Approach Approach to prolapse surgery include vaginal, abdominal, and laparoscopic routes or combination of approaches. Vaginal approach results in: * * * fewer wound complications, less postoperative pain, shorter hospital stay Vaginal procedures for prolapse * * * Restorative → use the patient’s endogenous support structures Sacrosinous Suspension Uterosacral suspension Iliococcygeus Fascia Suspension Compensatory → replace deficient support with some type of graft Obliterative → close the vagina Le fort colpoclisis Total colpoclisis Preoperative Evaluation And Preparation * * * A thorough pelvic floor history, Assessment of bothersome urinary symptoms and/or defecatory problems . A thorough speculum and bimanual pelvic examination The findings of the examination should be recorded using a quantitative and reproducible method for recording POP. Evaluation Of Urinary Dysfunction * Urinary incontinence • Reduced stress testing. • Urodynamics? * Urinary retention • Measure PVR 13 to 65 percent of continent women develop symptoms of SUI after surgical correction of the prolapse. Obliterative Procedure Obliterative surgery corrects prolapse by removing and/or closing off all or a portion of the vaginal canal (colpocleisis) * * Total colpocleisis Partial colpocleisis (Le Fort colpocleisis) Concomitant hysterectomy? Concomitant stress urinary incontinence surgery ? Kelly suburethral plication midurethral sling Effects of colpocleisis on bowel symptoms At baseline Bothersome bowel symptom(s) were present in 77% : * * * Obstructive (17-26%), Incontinence (12-35%) and Pain/irritation (3-34%) Procedures performed: partial colpocleisis (61%), total colpocleisis (39%), levator myorrhaphy (71%), and perineorrhaphy (97%). RESULTS: Of 121 (80%) subjects with complete data, Mean age was 79.2 +/- 5.4 years and all had stage 3-4 prolapse The majority of bothersome symptoms resolved (50-100%) with low rates of de novo symptoms (0-14%). CONCLUSIONS: Most bothersome bowel symptoms resolve after colpocleisis, especially obstructive and incontinence symptoms, with low rates of de novo symptoms. Sacrospinous Ligament Fixation * * * * The surgeon should be familiar with the anatomy of the sacrospinous ligament complex and of the pararectal space. Obtaining adequate exposure can be difficult. The sacrospinous ligament is a cordlike structure that exists within the body of the coccygeus muscle. The sacrospinous ligament attaches medially to the sacrum and coccyx and attaches laterally to the ischial spine. Sacrospinous Ligament Fixation * * * * The pudendal nerve and vessels pass directly posterior to the ischial spine. The sciatic nerve lies superior and lateral to the sacrospinous ligament. Superior to the ligament lies the inferior gluteal vessels and the hypogastric venous plexus. To avoid trauma to these structures, it is important to place the fixation sutures two fingers medial to the ischial spine. Complications * * * * * Hemorrhage can result from injury to the hypogastric venous plexus inferior gluteal vessels, and internal pudendal vessels. Postoperative gluteal pain due to pudendal nerves and the sciatic nerve injury. Approximately 10% to 15% of patients have transient moderate to severe buttock pain Inadvertent proctotomy. Potential stress incontinence. Results of sacrospineous Ligament Suspension for Vaginal Vault Prolapse Author No. of patients Follow-up in months (range) Success Jenkins 1997 50 6-48 88% Barber 2001 46 3.5-40 90% Karram 2001 202 6-36 89.5% Amundsen 33 et al. 2003 6-43 82% Viviane Diet 133 z 2006 3-55 84% Total transvaginal mesh (TVM) technique Prolift Pelvic Floor Repair System™ Complications * Febrile morbidity * Urinary tract infection * Deep hematoma * Granuloma (without exposure) * Mesh exposure * Shrinkage of mesh Ojectives: The objective of the study was to assess the effectiveness and complication rates for the transvaginal (TVM) technique in the treatment of pelvic organ prolapse (POP). Methods: All enrolled patients underwent prolapse repair surgery with GYNEMESH PS Prolene Nonabsorbable Soft Mesh using the TVM technique Conclusions: • Five-year results indicated that TVM provided a stable anatomic repair. • Improvements in quality of life and associated improvements in specific prolapse symptoms were sustained over the 5-year period. • Mesh exposure was the most common complication Of 85 patients: • 16 comlicated with Mesh exposure • 9 required partial mesh excision. • 3 patients with some degree of dyspareunia, (in 8, preexisting dyspareunia resolved). • 1 rectovaginal fistula reported and • 2 reported ureteral injuries, one of which resulted in a ureteral-vaginal fistula; all resolved after repair • 5 required reoperation for prolapse by 5 years To elucidate the outcome of transvaginal pelvic reconstructive surgery using polypropylene mesh (Gynemesh; Ethicon, Somerville, NJ, USA) for patients with pelvic organ prolapse (POP) stage III or IV. RESULTS: The average age of the patients was 64.1 years and average parity was 3.9 The success rate was 97.4%. Only one patient (2.6%) had recurrent genital prolapse (stage II) postoperatively.). The complication rate was 10.3 %, including onevaginal mesh erosion (2.6%), one dyspareunia (2.6%) (and two prolonged bladder drainage (longer than 14 days Neither long-term nor major complication was identified CONCLUSION: Transvaginal pelvic reconstructive surgery with polypropylene mesh reinforcement is a safe and effective procedure for POP on 1.5 years' follow- up. It also has positive influence on quality of life. Sacrocolpopexy and paravaginal repair for total pelvic floor prolapse