NPTE Pharmacology - Dr. Tomas Madayag
advertisement

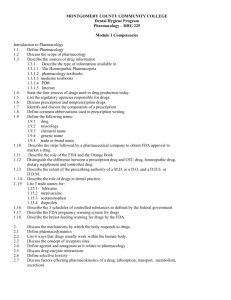
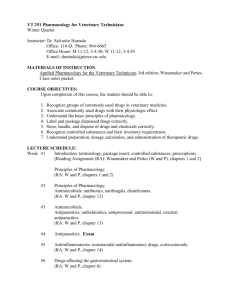
NPTE Pharmacology Basic Principles of Pharmacology • Drug Nomenclature – Chemical name – Generic name – Trade name Basic Principles of Pharmacology • Drug Development & Approval – FDA – Preclinical testing – Human testing – New drug application approval Basic Principles of Pharmacology • Controlled substances – Schedule 1- (mescaline, marijuana, heroine) • highest potential for abuse • Restricted to approved research – Schedule 2- (morphine, meperidine, barbiturates) • Specific therapeutic purpose • High potential for abuse – Schedule 3 (opioids) • Mild to moderate dependence – Schedule 4 (benzodiazepines) • Low potential for abuse – Schedule 5 (low doses of opioids) • Lowest relative abuse potential Pharmacokinetics • Routes of administration ENTERAL Parenteral Oral Inhalation Sublingual Intravenous Rectal Intra-arterial Intramuscular Intrathecal Topical Transdermal • Drug elimination rates – Clearance • Blood flow to the organ • Extraction ratio – Half life • Amount of time required for 50% of drug to be eliminated Drug Receptors • Agonist vs Antagonist – Agonist • Drug binds to receptor & initiates a change in function of cell – Antagonist (Blockers) • Drug binds to receptor but will not cause change the function of cell CNS Pharmacology • The Blood Brain Barrier – Inability to pass from bloodstream to CNS – Tight junctions between capillary endothelial cells – Non-polar, lipid soluble drugs able to cross by passive diffusion CNS Pharmacology • Sedative-Hypnotic & anxioloytics – Barbiturates • Barb- – Benzodiazepines • -epam • -olam Problems & adverse effects Tolerance & physical dependence Residual effects GI (N & V), dry mouth Incoordination CNS Pharmacology • Considerations for the PT – Patient calmer – Benzodiazepines reach peak 2-4 hrs • Schedule sessions during that time • In over sedated states – Hazardous to do gait training & exercise DRUGS USED FOR AFFECTIVE DISORDERS • Pathophysiology of depression – Underactive influence of NE, serotonin, dopamine in limbic system – Increased sensitivity of the post-synaptic receptor for NE • Leads to compensatory decrease in sensitivity of the receptor • Drugs for affective disorders – Tricyclics • Blocks re-uptake of amine neurotransmitters into the presynaptic terminal • -triptyline; -pramine (amitriptyline; desipramine) – MAO inhibitors • Enzyme located at amine synapses • Blocking this enzyme allow released amines to remain in the cleft • (Isocarboxazid [Marplan]; Phenelzine [Nardyl]; tranylcypromine [parnate]) – Second-generation agents • Mechanisms similar to tricyclics • Selective blocking of serotonin • Bupropion [Wellbutrin]; fluoxetine [Prozac]; sertraline [Zoloft]) • Problems & adverse effects – Tricyclics • Sedation • Anticholinergic effects – – – – – – Confusion, delirium Dry mouth, constipation Urinary retention Tachycardia Arrhythmias, orthostatic hypotension Potential for fatal overdose • Problems & adverse effects – MAO Inhibitors • CNS excitation – Restlessness, irritability, agitation, sleep loss • Central & peripheral anticholinergic – Tremor, confusion, dry mouth, urinary retention – *may cause ↑BP, HTN crisis » Ingested tyramine + decreased catecholamine breakdown (MAO inhibition)→ hypertensive crisis » Avoid fermented cheese and wine • Manic-Depression – Mood swings • Overactive NE & serotonin → manic phase • Rebound effect→ depression • Manic-Depression – Lithium • Precise mechanism of action remains undetermined • Therapeutic: 1.0 to 1.4 mEq/L • Toxic: 2.5 mEq/L • Special Concerns for PT – These drugs maybe used for other reasons (SCI, burns, amputation, pain) – Sedation, lethargy & muscle weakness (tricyclics, lithium) – Orthostatic hypotension (tricyclics) – Hypertensive crisis – Suicidal tendency • Anti-psychotics (neuroleptics) – Schizophrenia • • • • Marked disturbance in thought Delusions Hallucinations ? Increased dopamine???? – Severe paranoid disorders • Problems & Adverse Effects – EPS – Less likely with clozapine (Clozaril) because selective for dopamine receptors that affect behavior rather than those affecting motor function • Tardive dyskinesia • Pseudoparkinsonism – Resting tremor, bradykinesia, rigidity • Akathisia (motor restlessness) • Dyskinesia & dystonias (torticollis, oculogyric crisis, opisthotonos) • Neuroleptic malignant syndrome (catatonia, stupor, rigidity, tremors, fever) – Severe – High mortality • Problems & Adverse Effects – Nonmotor effects • Sedation • Anticholinergic effects • Other – Orthostatic hypotension – Photosensitivity (chlorpromazine) • Special Concerns for the PT – Monitor motor involvement • Change in posture, balance • Involuntary movements – **refer to health care provider ANTIEPILEPTIC DRUGS • Antiepileptic Drugs – Epilepsy- recurrent seizures – Seizures- sudden, transient disturbances in cerebral excitation • Classification of Seizures – Generalized, partial, or unclassified – Partial • Only part of the brain is involved (e.g. one cerebral hemisphere) – Generalized • Whole cerebral brain is involved • Partial Seizures Type Classification Simple partial Limited (focal) motor or sensory signs Consciousness remains intact Complex partial seizures Consciousness impaired; bizarre behavior Partial becoming generalized progressive • Generalized seizures Seizure type Classification Absence (petit mal) Sudden brief loss of consciousness Motor signs may be absent Myoclonic Sudden, brief, shock-like contraction of muscles in the face & trunk or in one or more extremities Consciousness may be impaired Clonic Rhythmic, synchronized contractions throughout the body Loss of consciousness Tonic Generalized, sustained contractions throughout body Loss of consciousness Tonic-clonic (grand Sustained contractions of all muscles (tonic phase) followed by mal) powerful rhythmic contractions (clonic); loss of consciousnesss Atonic Sudden loss of muscle tone; consciousness may be maintained or lost briefly • Drugs used to treat epilepsy – Barbiturates – Benzodiazepines – Carboxylic acids (valproic acid [Depakene]) – Dicarbamates (felbamate [Felbatol]) – Hydantoins (phenytoin) – Iminostilbenes (carbamezapine [Tegretol]) – Oxazolidinediones (paramethadione [Paradione]) – Succinimides (ethosuximide [Zarontin]) • Special concerns for the PT – Frequent side effects affecting treatment • Headache, dizziness, sedation, gastric disturbances – Schedule when sx are mild • Cerebellar side effects (e.g. ataxia) – Coordination exercises • Prevention of seizures – Quiet setting for therapy Pharmacology in Parkinson’s • Pertinent facts – Movement disorder – Pathophysiology • Degeneration of dopamine producing cells in substantia nigra – Loss of dopaminergic input into corpus striatum • Therapeutic Agents – Levodopa – Levodopa- Carbidopa (1:4-1:10) • Adverse Effects – GI – CV » Arrhyhtmias, postural hypotension – Dyskinesias – Behavioral changes • Other Drugs – Dopamine agonists • Bromocriptine (Parlodel) • Pergolide (Permax) – Anticholinergics • Benztropine mesylate (Cogentin); trihexyphenidyl (Artane); diphenhydramine (Benadryl) – Amantadine (Symmetrel)- anti-viral. Exact mechanism ?? – Selegiline (Eldepryl)- prevents breakdown of dopa • Special considerations for PTs – Coordinate treatment with peak effect (1 hr) – Schedule after breakfast dose – During drug holiday- maintain mobility – Monitor BP – Prevent orthostatic hypotension Local Anesthetics • Methods of administration – Topical – Transdermal • Iontophoresis (electricity) • Phonophoresis (ultrasound) – Infiltration – Peripheral nerve block – Central neural blockage • Epidural • Spinal nerve block – subarachnoid – L3-L4 or L4-L5 • Significance in Rehabilitation – Schedule sessions immediately after injection – When central neural blockage used • Sensation below diminished • Motor function affected DRUGS AFFECTING SKELETAL MUSCLE Skeletal Muscle Relaxants • Centrally acting agents – Baclofen (GABA agonist) • Drowsiness, confusion, hallucinations – Diazepam • Sedation – Others • • • • Carisoprodol (Soma) Cyclobenzaprine (Flexeril) Metaxalone (Skelaxin) Methocarbamol (Robaxin) – Drowsiness, dizziness • Direct-acting Relaxants – Dantrolene Sodium (Dantrium)- impairs Ca+ release • Generalized muscle weakness • Hepatotoxicity • Other relaxants – Botulinum Toxin (Botox) • Symptoms return after 2 to 3 months – Transdermal clonidine • Useful in spasticity in SCI • Special Concerns for PTs – Accommodate sedation effects – Schedule when effects are at a minimum DRUGS USED TO TREAT PAIN & INFLAMMATION Opioid Analgesics • Strong Agonists – for severe pain (mu & kappa receptors) – Fentanyl (Sublimase) – Hydromorphone (Dilaudid) – Meperidine (Demerol) – Methadone (Dolophine) – Morphine (Duramorph) – Oxymorphone (Numorphan) • Mild to moderate agonists – Codeine – Hydrocodone (Hycodan) – Oxycodone (Percodan) – Propoxyphene (Darvon) • Mixed Agonist-Antagonists (kappa & sigma receptors) – Less tolerance & dependence • Naloxone (Narcan) • Naltrexone • Special Concerns for PTs – Schedule during peak effects – Respiratory response to exercise blunted (↓rate) • Nonsteroidal Anti-inflammatory Drugs – – – – – – – – – – Aspirin Diclofenac (Voltaren) Diflunisal (Dolobid) Ibuprofen (Motrin) Indomethacin (Indocin) Ketorolac (Toradol) Mefenamic acid (Ponstel) Naproxen (Anaprox, Naprosyn) Piroxicam (Feldene) Sulindac (Clinoril) • Mechanism of action of NSAIDS Inhibition of cyclooxygenase enzyme Elimination of thromboxane & prostaglandin • Special Concern for PTs – Good for moderate to mild pain but not for severe pain – GI complications – Acetaminophen lacks anti-inflammatory effects – High-dose of ASA can lead to hearing loss PHARMACOLOGY IN RA OR OSTEOARTHRITIS • Goals of treatment – To decrease joint inflammation • NSAIDs • corticosteroids – To arrest progression of disease • DMARDs • Corticosteroids – Inhibits prostaglandin & leukotriene • Betamethasone (Celestone) • Dexamethasone (Decadron) • Methylprednisolone (Medrol) – Adverse side effects • • • • Osteoporosis Muscle wasting, weakness Aggravation of DM Cataracts & glaucoma • DMARDS – Modifies the pathologic process – Inhibit immune response • Anti-malarial drugs (decreased T cells) – Chloroquine (Aralen); hydroxychloroquine (Plaquenil) – Adverse effects: retinal damage • Azathioprine (Imuran)- impairs DNA – Adverse effect: fever, chills, sore throat fatigue, loss of appetite, n&v • Gold therapy- inhibiting phagocytes – Aurothioglucose (Solganal); gold sodium thiomalate (Miochrysine) – Adverse effects: GI, stomatitis, thrombocytopenia, leukopenia • DMARDS –continued – Methotrexate (Folex, Rheumatrex)inhibits folic acid decreased nucleoproteins impaired production of genetic material • Adverse Side Effects – GI including GI bleed – Penicillamine (Cuprimine)- depresses T cell function • Adverse Side Effects – Fever, joint pain, rashes, lymph swelling • Special Concerns for PTs – Use ROM & strengthening exercises cautiously in those on corticosteroids – Prevent skin breakdown- corticosteroids AUTONOMIC & CV PHARMACOLOGY The Autonomic Nervous System • Divisions – Sympathetic NS (thoracolumbar division) – Parasympathetic or craniospinal – (originating in mid-brain, brainstem & sacral region of the spinal cord) Sympathetic • Heart – ↑contractility (beta 1) – ↑ heart rate (beta 1) • Arterioles – VC -skin & viscera (alpha-1) – VD sk. Muscle, liver (beta-2) • Lungs – BD (beta-2) Parasympathetic • Heart – ↓ HR (musc) – ↓ contractility-slight (musc) • Arterioles – No innervation • Lungs – BC (musc) Sympathetic • GI Function – ↓ motility (alpha 1,2; beta 1,2) • Bladder detrusor – Relaxation (beta 2) • Bladder Trigone & Sphincter – Contraction (alpha 1) • Liver – Glycogenolysis & gluconeogenesis (alpha 1, beta 2) Parasympathetic • GI Function – ↑ motility & secretion (musc) • Bladder detrusor – Contraction (musc) • Bladder Trigone & Sphincter – Relaxation (musc) • Liver – Glycogen synthesis (musc) Adrenergic Receptors • Alpha-1 – Smooth muscle • Alpha-2 – CNS inhibitory synapses – GI tract, pancreatic islet cells (↓insulin secretion) • Beta-1 – Predominate in heart & kidneys (↑ renin) • Beta-2 – Bronchiole smooth muscle (relaxation) – Some arterioles (vasodilation) Cholinergic Drugs • Bethanechol – Post op GI & urinary atony • Pilocarpine – Glaucoma Antimuscarinic Anticholinergic Drugs • Prototype- Atropine • Clinical applications – GI system • Peptic ulcer, IBS – Parkinson’s – Motion sickness Adrenergic Drugs • Alpha-1 Selective Agonists – Primarily on vascular smooth muscle • Vasoconstriction & increased PVR – Phenylephrine – Pseudoephedrine • Alpha-2 Selective Agonists – Inhibits sympathetic discharge • Useful in hypertension – Clonidine, methyldopa • Beta-1 Selective Agonists – Receptor primarily in myocardium – Increased heart rate & inotropy • Dobutamine • Dopamine • Beta-2 Selective Agonists – Bronchiole smooth muscle • Albuterol (Proventil, Ventolin) • Isoetherine • Metaproterenol (Alupent) Adrenergic Antagonists • Alpha antagonists – Reduces peripheral vascular tone→ vasodilation • Ergotamine, phentolamine, prazosin • May cause reflex tachycardia • Beta Antagonists – Negative chronotropic, negative inotropic • Acebutolol, Esmolol, Nadolol, Propranolol ANTIHYPERTENSIVE DRUGS Diuretics – Decreases circulating volume • Classification – Thiazide • Inhibits Na+ reabsorption – Chlorothiazide – Loop (ascending loop) • Inhibits reabsorption of Na+ and CL– Bumetanide, Ethacrynic acid, Furosemide – Potassium Sparing (distal tubule) • Prevents K+ excretion – Amiloride, Spironalactone, Triamterene (Dyrenium) Sympatholytic Drugs • Beta Blockers – Lowers heart rate & force of contraction= decreased CO • Acebutolol • Labetalol • Alpha Blockers – Decreased vascular resistance • Doxazosin, Prazosin, Terazosin Presynaptic Adrenergic Inhibitors • Inhibits release of norepinephrine – Guaethidine, Reserpine Centrally Acting Agents • Inhibition of sympathetic discharge from the brainstem – Clonidine, methyldopa Vasodilators • Decreased peripheral resistance – Hydralazine, Diazoxide (Hyeprstat) ACE Inhibitors • Prevention of conversion of Angiotensin I to AII – Benazepril – Captopril – Enalapril – Fosinopril Calcium Channel Blockers • Inhibits contractile process – Diltiazem – Felodipine – Isradipine – Nicardipine – Nifedipine – Verapramil Special Concerns for the PT • Caution in changing postures • Avoid widespread vasodilation – Whirlpool, Hubbard Tank • Exercise may cause vasodilation in skeletal musculature • If beta blockers- exercise tolerance may be impaired • Encourage compliance TREATMENT OF ANGINA PECTORIS Organic Nitrates • Precursor, activated when converted to nitrous oxide→vasodilation • Dilation of systemic venous system; arterioles→ decreased PVR • Decreased pre-load, afterload • Decreased myocardial O2 demand – Nitroglycerine – Isosorbide dinitrate – Amyl nitrite Beta-adrenergic blockers • Decreased heart rate • Negative inotropic effect – Atenolol – Metoprolol Calcium Channel Blockers • Coronary vasodilation • Peripheral vasodilation – Diltiazem – Felodipine – Nifedapine Special Concerns for PTs • Make sure patient has NTG available • Angina may occur during therapy • Patients taking these drugs may have increase tolerance to exercise • Some drugs may blunt ability of heart to respond to exercise • Adjust exercise workloads • CaCB & nitrates- patients may experience hypotension when systemic heat is applied TREATMENT OF CARDIAC ARRHYTHMIAS • Sodium channel blockers – Procainamide, Quinidine • Beta Blockers • Class III- prolongs repolarization – Bretylium; Amiodarone • CCB • Special Concerns for the PT – In exercise (cardiac rehab) monitor for arrhythmias – Watch for postural hypotension TREATMENT OF CHF • • • • Digitalis glcosides Diuretics ACEI Other – Amrinone, Milrinone- + inotropic – Dopamine, dobutamine – vasodilators • Special Concerns for the PT – Monitor for signs of CHF – Report signs of digitoxicty – Watch for postural hypotension COAGULATION DISORDERS &HYPERLIPIDEMIA • Drugs to treat overactive clotting – Anticoagulants • Heparin, Oral anticoagulants – Antithrombotic drugs • ASA – Thrombolytics • Streptokinase, urokinase • tPa • Treatment of clotting deficiencies – Vitamin K – Antifibrinolytics • Aminocaproic acid (Amicar) • Agents to treat hyperlipidemia – HMG-CoA Reductase Inhibitors • Decreases cholesterol production (LDL, VLDL) – Lovastatin, pravastatin, simvastatin – Fibric acid • Increases breakdown of triglyceride-rich lipoproteins (LDL, IDL) • Clofibrate, gemfibrozil – Adverse Effects • GI, cutaneous vasodilation (niacin) • Liver dysfunction, gallstones, pancreatitis • Myalgia, fatigue/weakness • Special Concerns for PTs – Those on anticoagulants, watch for bleeding – Caution with deep tissue massage or chest percussion – Hemophilia-hemarthrosis • Improve joint function after resolution RESPIRATORY & GI PHARMACOLOGY Respiratory Drugs • • • • • Drugs for Respiratory Tract irritation Antitussives Decongestants Antihistamines Mucolytics & expectorants • Drugs to maintain airway patency on Obstructive PD – Beta adrenergic agonists • Albuterol, epinephrine, isoetharine, metaproterenol, terbutaline – Xanthine derivatives • Aminophylline, theophylline – Anticholinergic drugs • Ipratropium (atrovent) – Corticosteroids • Beclomethasone, dexamethasone – Cromolyn sodium • Prevents bronchospasm • Treatment of bronchial asthma – Steroids – Beta-2 agonists – Leukotriene inhibitors • Special Concerns for PTs – Postural drainage & breathing exercises – Chest PT more effective after 30 min-1 hr. after treatment – Advise patients to bring medications – Monitor side effects • Arrhythmias, nervousness, confusion • For those on steroids- watch for skin breakdown GI Drugs • Control of gastric acidity & secretion – Antacids – H2 receptor Blockers • Cimetidine, Famotidine, Nizatidine, Ranitidine – Anticholinergics • Pirenzepine – – – – Metaclopramide (Reglan) Omeprazole (Prilosec) Sucralfate, Carafate Prostaglandins • Misoprostol (Cytotec) • Special Considerations for the PT – GI drugs well tolerated – Generally will not interfere with therapy ENDOCRINE PHARMACOLOGY • Special Concerns of adrenal steroid – Causes general breakdown (catabolic) in muscle, bone, skin, & other collagenous structures – Strengthening exercises help maintain muscle mass – Weight bearing to reduce bone loss – Avoid injury – Prevent skin breakdown – Na+ & water retention – Immunosuppression – Watch for mood changes & psychoses • Special concerns for use of sex hormones (estrogen progesterone, androgens) – Monitor BP (salt & H2O retention) – Teach about effects if androgens • Thyroid & Parathyroid Drugs – Hyperthyroidism • Iodide • Radioactive iodine – Hypothyroidism • • • • Levothyroxine Liothyronine Liotrix Thyroglobulin • Parathyroid Glands – PTH- controlled release by amount of Ca+ in plasma • ↓ plasma calcium stimulates PTH – Increases bone resorption, – renal reabsorption (as renal calcium reabsorption, PTH also increase phosphate excretion)→ rise in Ca+, ↓ plasma phosphate – GI tract via interaction of PTH & Vitamin D » PTH increases conversion of Vit. D to 1,25-dihydroxycholecalciferol (calcitrol) which increases GI reabsorption of Ca+ (small intestine) • Regulation of Bone Mineral Homeostasis – Parathyroid Hormone • Decreased or normal PTH encourages bone synthesis & remodeling – Vitamin D • Increases intestinal calcium and phosphate absorption • Decreases renal calcium & phosphate excretion • Enhances bone formation by increasing Ca+ & Phosphate – Calcitonin • Antagonist to PTH • Lowers blood calcium by stimulating bone formation • Increases renal excretion of calcium & phosphate Drugs for Bone Homeostasis • Calcium Supplements – Calcium gluconate • Vitamin D analogues – Calcifediol – Calcitriol • Diphosphonates – Etidronate • Calcitonin – Calcimar • Special Concerns – Do not overstress hypothyroid patients – Calcium abnormality- watch arrhythmias – Ultraviolet light increases endogenous Vitamin D biosynthesis facilitating calcium absorption and bone formation • Significance of Diabetes Mellitus for PTs – Watch for hypoglycemia – Ensure that patient did not skip meal before exercise – Have sources of glucose available