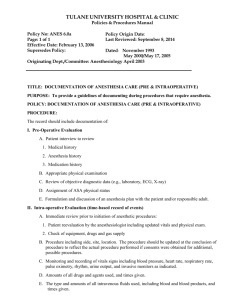
Clinical Decision Support

Perioperative Information Management Systems:
Driving Discovery & Reliability
In The Operating Room
Jesse M. Ehrenfeld, M.D., M.P.H.
Assistant Professor of Anesthesiology
Assistant Professor of Biomedical Informatics
Director, Perioperative Data Systems Research
Director, Center for Evidence-Based Anesthesia
Medical Director, Perioperative Quality
Co-Director, Vanderbilt Program for LGBTI Health
Vanderbilt University School of Medicine
Department of Anesthesiology jesse.ehrenfeld@vanderbilt.edu
Overview
Part I – Perioperative Information
Management Systems
Overview & Functionality
Reliable Processes
Part II – Clinical Decision Support
The Problem, The Need, Opportunities
Part III – Our Research & The Future
Using PIMS to Measure & Increase Reliability
Predictive Modeling / Real Time Feedback Loops
Case Studies: Blood Pressure Gaps & Glucose Control
Vanderbilt Department of Anesthesiology
60,000 adult and pediatric patient encounters
90 anesthetizing locations
20,000 patients are seen in the Vanderbilt Preoperative
Evaluation Clinic (VPEC)
3,000 patients are seen annually in our Vanderbilt
Interventional Pain Center
20,000 Vanderbilt adult and pediatric patients receive an anesthetic during a radiologic, gastrointestinal, or other diagnostic or therapeutic procedure
Provide care in eight intensive care units, including six adult, the pediatric and neonatal intensive care units
4,000 anesthetics per year in the labor and delivery suite
Perioperative Data Systems Research Group
Undergraduate Students
• Molly Cowan
• Lindsay Lee
• Shane Selig
• Jacob Shiftan
• Emily Wang
Graduate Students
• Amlan Bhattacharjee
• Sean Chester
• Kristen Eckstrand
• Aneesh Goel
• Paul Hannam
• Mary Marschner
• Monika Jering
• Ilana Stohl Project
Manager
Angelo del Puerto
Director
Jesse Ehrenfeld, MD
Data Warehouse
Architect
Michealene Johnson
Health Systems
Database Analyst
Dylan Snyder
Research
Analyst
Khensani Marolen
Data Intelligence
Analyst
Jason Denton
Health Systems
Database Analyst
Chris Eldridge
Data
Management
Specialist
TBD
Last updated 7.2012
Research
Assistant
Rasheeda Lawson
Overview
Part I – Perioperative Information
Management Systems
Overview & Functionality
Reliable Processes
Part II – Clinical Decision Support
The Problem, The Need, Opportunities
Part III – Our Research & The Future
Using PIMS to Measure & Increase Reliability
Predictive Modeling / Real Time Feedback Loops
Case Studies: Blood Pressure Gaps & Glucose Control
Biomedical Informatics
Medical Informatics
• Intersection of information science, computer science and health care
• Resources, devices, methods optimize information acquisition, storage, retrieval and use
• Involves computers, clinical guidelines, information, medical terminologies, communications systems
Perioperative Information Management Systems
Accurate / reliable data recording
Interface with hospital-wide EHR
PIMS Adoption in the U.S. – 2011
10
5
0
Geographical
Distribution
Northeast
Southeast
Southwest
Midwest
West
30
20
10
0
Academic Status
Teaching
40
30
20
10
0
40
30
20
10
0
Population/Development
Size
Stohl, Sandberg, Ehrenfeld. Assoc. of SCIP Compliance with Use of a PIMS. (submitted)
Rural
Urban
Areas Impacted by PIMS
Patients
Major Areas of Impact
Departmental management
Clinical
Practice
Ehrenfeld, J.M., Rehman, M.A. “Anesthesia Information Management Systems: Current
Functionality and Limitations” (2010) Journal of Clinical Monitoring and Computing Aug 24
PIMS: Impact on Patients
Impact on patients
• Provision of real-time intraoperative decision support
• Allows the anesthesia care team to focus on the patient, rather than recording vital signs
• Better legibility and availability of historical records
• More precise recording of intraoperative data & patient responses to anesthesia
Chau, A., Ehrenfeld, J.M. “Using Real Time Clinical Decision Support to Improve
Performance on Perioperative Quality and Process Measures” (2011) Anesthesiology
Clinics
PIMS: Impact on Dept Management
Impact on
Departmental
Management
• Supply cost analysis by provider/type of surgery/patient
• Improved billing accuracy and timeliness
• Fulfills the Joint Commission requirements for legible and comprehensive patient records
• Facilitates verification of Accreditation
Council for Graduate Medical Education case requirements for trainees
• Simplifies compliance with concurrency and other regulatory issues
Chau, A., Ehrenfeld, J.M. “Using Real Time Clinical Decision Support to Improve
Performance on Perioperative Quality and Process Measures” (2011) Anesthesiology
Clinics
PIMS: Impact on Clinical Practice
Impact on
Clinical
Practice
• Provides precise, high-resolution records which can be used for educational purposes
• Enables researchers to rapidly find rare events or specific occurrences across a large number of cases
• Facilitates individual provider performance tracking
• Allows better quality assurance functionality through the creation of more complete and precise records
• Integration with other hospital databases can allow assessment of short and long term patient outcomes
• Provision of additional legal protection via the availability of unbiased, precise information
Chau, A., Ehrenfeld, J.M. “Using Real Time Clinical Decision Support to Improve
Performance on Perioperative Quality and Process Measures” (2011) Anesthesiology
Clinics
Mobile PIMS: VigiVU TM
Transformative technology
• Enhance situational awareness
• Enable development of new anesthesia care models
• Significant impact on operational efficiency
Mobile PIMS: VigiVU TM
Push Notifications
Push Notifications
• Abnormal vital signs
• Lab results
• Operational notifications
• Patient in holding
• Patient in OR
• Surgeon closing
• Notable drug events
• Vasoactives
Process Reliability
Processes are collections of systems and actions following prescribed procedures for bringing about a result.
Reliability of any processes can be determined using data when process failure criteria are established.
Results of the analysis can be graphically displayed, problems identified, categorized and identified for corrective action.
The hardest part of any reliability analysis is getting the
data.
Process Reliability in Health Care
Given our intentions, as talented providers, why are clinical processes carried out at such low levels of reliability?
Don’t show up for work wanting to provide bad care!
‘‘It’s the system, not the people’’ – true, but not helpful as we aim to improve our processes
Resar, RK. Making Noncatastrophic Health Care Processes Reliable. Health Serv Res. 2006.
Process Reliability in Health Care
Reasons for reliability gap:
Health care improvement methods excessively dependent on
vigilance and hard work
We benchmarking to mediocre outcomes in health care – leads to false sense of process reliability
Allow clinical autonomy creates wide, unjustifiable, performance variation
Processes not designed to meet specific, articulated reliability
goals.
Resar, RK. Making Noncatastrophic Health Care Processes Reliable. Health Serv Res. 2006.
Overview
Part I – Perioperative Information
Management Systems
Overview & Functionality
Reliable Processes
Part II – Clinical Decision Support
The Problem, The Need, Opportunities
Part III – Our Research & The Future
Using PIMS to Measure & Increase Reliability
Predictive Modeling / Real Time Feedback Loops
Case Studies: Blood Pressure Gaps & Glucose Control
Clinical Decision Support
Perioperative Info.
Management Systems
• Not just record keeping systems
• Facilitate application of
• collective wisdom of previous
• cases to your current patient
• “Big brain” in the sky
• Advice and support
Problem/Need
Why do we need clinical decision support?
Mistakes happen
You own a calculator don’t you?
Knowledge evolves
Pubmed / Medline
Problem/Need
To err is human
• Time constraints
• Frequent interruptions
• Limits of memory
• Multi-tasking
• Fatigue
Not just looking for errors
• Define optimal care improve our performance
General Solution: Decision Support
“Clinical consultation systems that use population statistics and expert knowledge to offer real-time advice to clinicians…they provide for patient
specific information management and consultation.”
- EH Shortliffe, JAMA 1987;258:61-6
Clinical Decision Support
Objective: assist clinicians in
(1) making the best clinical decision and
(2) following recommended practices
Wide range of tools:
very simple data field checks
complex calculations performed in the background
Potential to changes approaches to patient safety
Reactive Proactive
General Solution: Decision Support
Goals in the Operating Room:
Optimize outcomes by enabling physicians
Reduce errors by providing reminders
Increase skill by sharing information
OR Decision Support Hierarchy
Type
Consequence
Level
Level of
Difficulty
Managerial Low Low
Example: Bayesian analysis to predict amount of surgical time remaining
Process of Care Medium Medium
Example: SCIP measures (antibiotics before incision, normothermia, etc.)
Outcome Based High High
Example: Provide risk-adjusted 30 day post-op pain scores after arthoplasty
OR Decision Support Hierarchy
Type
Consequence
Level
Level of
Difficulty
Managerial Low Low
Example: Bayesian analysis to predict amount of surgical time remaining
Process of Care Medium Medium
Example: SCIP measures (antibiotics before incision, normothermia, etc.)
Outcome Based High High
Example: Provide risk-adjusted 30 day post-op pain scores after arthoplasty
OR Decision Support Hierarchy
Type
Consequence
Level
Level of
Difficulty
Managerial Low Low
Example: Bayesian analysis to predict amount of surgical time remaining
Process of Care Medium Medium
Example: SCIP measures (antibiotics before incision, normothermia, etc.)
Outcome Based High High
Example: Provide risk-adjusted 30 day post-op pain scores after arthoplasty
OR Decision Support Hierarchy
Type
Consequence
Level
Level of
Difficulty
Managerial Low Low
Example: Bayesian analysis to predict amount of surgical time remaining
Process of Care Medium Medium
Example: SCIP measures (antibiotics before incision, normothermia, etc.)
Outcome Based High High
Example: Provide risk-adjusted 30 day post-op pain scores after arthoplasty
Clinical Decision Support
I’m not convinced. Does it really make a difference?
Perioperative Information
Management Systems (PIMS)
Mediate Improved SCIP
Compliance Compared to
Hospitals Without PIMS
Stohl, Sandberg, Ehrenfeld. Assoc. of SCIP Compliance with Use of an PIMS. (submitted)
Decision Support Version 1.0
Outside the Operating Room
Web-based tools
Computerized Physician Order Entry
PDA, iPhone applications
Inside the Operating Room
Anesthesia Information Management
Systems
Clinical Decision Support 2.0
Machine Learning
Techniques
Advanced Algorithms
Previous
Cases
Real-Time
Data
Clinical
Guidlines
Artificial
Intelligence
Contextual
Information
Processing
Clinical Decision Support 2.0
SURGICAL EVENT
(blood loss, allergy, etc) or
EXTERNAL EVENT
(lab values, new info, etc)
DATA FROM ALL
PREVIOUS CASES
SUGGESTIONS /
GUIDELINES /
STATISTICS
IDEAL
RESPONSE
Clinical Decision Support 2.0
Envelop of Care
Case Progression Over Time
Clinical Decision Support 2.0
Envelop of Care
Case Progression Over Time
Clinical Decision Support 2.0
Envelop of Care
Case Progression Over Time
Clinical Decision Support 2.0
Envelop of Care
Alert
Case Progression Over Time
Clinical Decision Support 2.0
Envelop of Care
Alert
Case Progression Over Time
Clinical Decision Support 2.0
Envelop of Care
Alert
Case Progression Over Time
Alerting
Once you generate knowledge/ information, how do you disseminate it?
Alerting modalities: Who and How?
Identify appropriate provider
Get their attention:
On-screen pop-ups
Pager messages
Emails
Limitations/Factors
Usability:
Ability to provide a useful function.
Does it do anything of value?
Limitations/Factors
Ergonomics:
The study of how people interact with their environment.
Can physicians use it?
Limitations/Factors
Latency:
Delays in usage and availability.
Will it work in a time-sensitive scenario?
Limitations/Factors
Interconnectivity / Interoperability:
Ability to connect to other sources of information and share information effectively.
Does it network well with existing infrastructure?
Limitations/Factors
Ability to Adapt:
If we don’t have the knowledge, can the system be used to generate missing info?
Can it develop a hypothesis?
Summary: Process Monitoring & Control
Goal: right info right time right person
Keys to electronic process monitoring
Process models
Process exceptions
Alert Generation
Overview
Part I – Perioperative Information
Management Systems
Overview & Functionality
Reliable Processes
Part II – Clinical Decision Support
The Problem, The Need, Opportunities
Part III – Our Research & The Future
Using PIMS to Measure & Increase Reliability
Predictive Modeling / Real Time Feedback Loops
Case Studies: Blood Pressure Gaps & Glucose Control
Required Components
Measure
Outcomes
Alerting Mechanism
Real-Time Data Capture
Define Norms of Practice / Baseline
Required Components
Measure
Outcomes
Alerting Mechanism
Real-Time Data Capture
Define Norms of Practice / Baseline
Required Components
Decision
Support
Engine
Measure
Outcomes
Alerting Mechanism
Real-Time Data Capture
Define Norms of Practice / Baseline
Define Norms of Practice
Single center retrospective analysis of PIMS data
Equipment performance characteristics
Ehrenfeld, J.M., Walsh, J.L. & Sandberg, W.S. “Right and Left Sided Mallinckrodt Double Lumen
Tubes Have Identical Clinical Performance” Anesthesia & Analgesia. (2008) 106 (6) 1847-1852.
Physiologic Monitoring
Ehrenfeld, J.M., Epstein, R.H., Bader, S., Kheterpal, S., Sandberg, W.S. “Automatic Notifications
Mediated by Anesthesia Information Management Systems Reduce the Frequency of Prolonged Gaps in Blood Pressure Documentation” Anesthesia & Analgesia. (2011) Aug;113(2):356-63. Epub 2011
Mar 17.
Ehrenfeld, J.M., Funk, L.M, Van Schalkwyk, J., Merry, A., Sandberg, W.S., Gawande, A. “Incidence of Hypoxemia During Surgery: Evidence from Two Institutions” Canadian Journal of Anesthesia.
2010: 57 (10) 888-97.
Predictors of Blood Transfusion
Henneman, J.P., Ehrenfeld, J.M. “A Predictive Model For Intraoperative Blood Product
Requirements” IARS, 5/11
Multi-center data aggregation (MPOG)
Epidural abscess / hematoma
Bateman, B.T., Mhyre, J.M., Ehrenfeld, J.M., Kheterpal, Abbey, K.R.,
Argalious, M., Berman, M.F., St. Jacques, P., Levy, W., Loeb, R.G., Paganelli,
W., Smith, K.W., Wethington, K.L., Wax, D., Pace, N.L., Tremper, K.,
Sandberg, W.S. “The Risk and Outcomes of Epidural Hematomas and
Abscesses Following Perioperative and Obstetric Epidural Catheterization:
A Report from the MPOG Research Consortium.” Anesth Analg. 2012 Apr 13.
Alerting Mechanisms
Notification modalities
Pagers / iPhones
On-screen pop-ups
Vibration belts
Heads-up displays
Frequency
One time vs. Multiple
Level of Acknowledgment
Hard-Stop vs. Soft Alerts
Alerts to Drive Performance
Active Avoidance Learning
Assessments of Cognitive Deficits in Mutant Mice
Ramona Marie Rodriguiz and William C. Wetsel
Duke University Medical Center
Outcomes Measurement
What are the Outcomes
Process of Care
“Wake-Up” time / Time to extubation
Room turnover time
Time to discharge from PACU
Patient Centered
Post-operative pain scores (immediate, 30 days)
Rates of PONV and PDNV
30 day re-admission rates
Mortality, wound infection rates
A Few Quick Examples …
…To Bring It All Together
1 . G A P S I N B L O O D P R E S S U R E
M O N I T O R I N G
2 . I N T R A O P E R A T I V E G L U C O S E
M O N I T O R I N G
3 . R E A L T I M E P A T I E N T P R E D I C T I V E
M O D E L S
4 . E N H A N C I N G V A L U E I N A N E S T H E S I A
Example #1
G A P S I N B L O O D P R E S S U R E M O N I T O R I N G
Ehrenfeld J, Epstein RH, Bader S, Kheterpal S, Sandberg WS. Automatic notifications mediated by anesthesia information management systems reduce the frequency of prolonged gaps in blood pressure documentation. Anesth Analg 2011;113:356–63
Gaps in Physiologic Monitoring
BP reading:
Induction:
BP reading:
9:52 am
9:53 am
10:08 am (16 minutes later)
Blood Pressure Gaps: Results
Blood Pressure Gaps: Results
Example #2
I N T R A O P E R A T I V E G L U C O S E M O N I T O R I N G
Closing Example
Diabetes Management
100.00%
90.00%
80.00%
70.00%
60.00%
50.00%
40.00%
30.00%
20.00%
10.00%
0.00%
12.22%
Diabetes Patients Receiving Intraoperative Insulin
Who Had Intraoperative Glucose Measured
100.00% 100.00%
24.33%
38.21%
57.84%
63.90%
77.52%
80.70%
87.88%
0-1 1-2 2-3 3-4 4-5 5-6 6-7
Surgical Duration
(excludes anesthesia induction & emergence time)
7-8 8-9 >9 hrs
Peterfreund, R.P., McCartney, K., Ehrenfeld, J.M. “Impact of Intraoperative Glucose Notifications” ASA 2012 (accepted)
Diabetes Management
100.00%
90.00%
80.00%
70.00%
60.00%
50.00%
40.00%
30.00%
20.00%
10.00%
0.00%
12.22%
Diabetes Patients Receiving Intraoperative Insulin
Who Had Intraoperative Glucose Measured
100.00% 100.00%
24.33%
38.21%
57.84%
63.90%
77.52%
80.70%
87.88%
0-1 1-2 2-3 3-4 4-5 5-6 6-7
Surgical Duration
(excludes anesthesia induction & emergence time)
7-8 8-9 >9 hrs
Peterfreund, R.P., McCartney, K., Ehrenfeld, J.M. “Impact of Intraoperative Glucose Notifications” ASA 2012 (accepted)
Better Care for Diabetic Patients
Peterfreund, R.P., McCartney, K., Ehrenfeld, J.M. “Impact of Intraoperative Glucose Notifications” ASA 2012 (accepted)
Better Care for Diabetic Patients
Reduced
Readmission
Rates
Peterfreund, R.P., McCartney, K., Ehrenfeld, J.M. “Impact of Intraoperative Glucose Notifications” ASA 2012 (accepted)
Example #3
R E A L T I M E P R E D I C T I V E
P A T I E N T M O D E L S
“Enhancing
Perioperative Safety
Through the
Determination of
Intraoperative
Predictors of Post-
Operative
Deterioration”
Funded by
Anesthesia Patient
Safety Foundation
PI – J. Ehrenfeld
Example #4
E N H A N C I N G V A L U E I N A N E S T H E S I A
Enhancing Value in Anesthesia
Wanderer, J.P., Hester, D., Ehrenfeld, J.M. “Cost Variability in Anesthesia Services” ASA 2012 (accepted)
Enhancing Value in Anesthesia
Wanderer, J.P., Hester, D., Ehrenfeld, J.M. “Cost Variability in Anesthesia Services” ASA 2012 (accepted)
Enhancing Value in Anesthesia
Value Cost
Enhancing Value in Anesthesia
Quality
Value
Cost
Enhancing Value in Anesthesia
Wanderer, J.P., Hester, D., Ehrenfeld, J.M. “Cost Variability in Anesthesia Services” ASA 2012 (accepted)
Vanderbilt Anesthesia Optimal Care Score
Real-Time Perioperative Dashboard
Blood Product Utilization Dashboard
Overview
Part I – Perioperative Information
Management Systems
Overview & Functionality
Reliable Processes
Part II – Clinical Decision Support
The Problem, The Need, Opportunities
Part III – Our Research & The Future
Using PIMS to Measure & Increase Reliability
Predictive Modeling / Real Time Feedback Loops
Case Studies: Blood Pressure Gaps & Glucose Control
What Does the Future Hold
More “Decision Support 2.0”
Live comparison of current clinical data
Indexed (pre-sorted) set of cases
Matching closest cases on surgery, age, ASA, etc
More Outcomes
Beyond PONV & the SSN death index
More Notification Modalities & Mobile Apps
More Patient Specific Real-Time Prediction Models
Perioperative Genomics
Conclusions
Medical Informatics will empower anesthesiologists in the 21 st century
Vanderbilt Perioperative Data Systems Research Group