Online Module: Brain Death Brain Death
advertisement

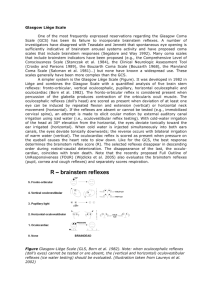
Online Module: Brain Death Brain Death Brain Death is “irreversible cessation of brain and brainstem function.” In Louisiana, any MD can pronounce a patient “brain dead,” although different institutions have different rules and regulations regarding this (for example, at LSU interim hospital it must be a chief resident or faculty physician). Criteria for determination of Brain Death Absent cerebral and brainstem function Well-defined etiology that is irreversible Persistent absence of all brain and brainstem function after observation and/or treatment Hypothermia, intoxication, metabolic encephalopathy, shock, and/or other reversible factors that can confound the assessment are excluded, corrected, and/or absent. In other words… There must be a known and sufficient etiology to account for the patient’s condition. All reversible causes of brainstem dysfunction must have been excluded. The passage of sufficient time to demonstrate irreversibility. The failure of all relevant therapeutic measures to reverse the condition. Don’t “D’oh!” A patient under anesthesia IS NOT BRAIN DEAD!!! Nor can you call an intoxicated patient brain dead (even though he/she may be), or a patient that has a core body temperature less than 90 degrees F, etc., etc., etc. Less than two years ago, a Louisiana resident MD declared a patient “brain dead” who literally walked out of the hospital two days later. Clinical Brain Death Cerebral unresponsiveness No spontaneous motor activity Absent brainstem reflexes Papillary, corneal, oculocephalic, etc. Absent cough/gag reflex with deep endotracheal suctioning Absent respiratory drive to hypercarbia (PaCO2>60) Confirmatory tests EEG Radionuleotide angiography Contrast cerebral angiography …or any radiographical method that assesses intracerebral blood flow Others exist… Confirmatory tests Key to understand is that none of these “confirmatory tests” is sufficient, in and of itself, to diagnose brain death. They are merely adjuncts. First, you must have a clinical exam consistent with brain death. Confirmatory tests A silent EEG, for example, can be consistent with brain death. It can also be consistent with pharmacological influence (i.e., anesthesia) or drug intoxication. By contrast, EEGs don’t always “confirm” brain death. There can be minor transient EEG activity even in the setting of clinical brain death. Electrical artifacts on EEG in the ICU setting have been described. Important point The most important thing to understand is that a good clinical examination is the foundation of an accurate brain death determination. Confirmatory tests are utilized on a case by case basis for a variety of reasons, but are nevertheless not the cornerstone of brain death determination. Moving to the clinical exam… Clinical Evaluation: Unresponsiveness The patient must demonstrate no response to any stimulation. Spontaneous movement is almost always absent. Seizures, shivering, any posturing, etc., indicates brainstem function and is not consistent with the determination of brain death. The presence of spinal reflexes does not exclude brain death, but if there is any doubt then the diagnosis of brain death should be withheld. Brainstem Reflexes: Pupils The pupils must be unreactive to light (note: they do NOT have to be dilated) in the absence of confounding variables (i.e. cateracts, significant ocular/orbital trauma, pharmacological effects, etc.). Any pupil movement in response to light is inconsistent with diagnosis of brain death. Review the light reflex pathway, in case you get asked! Brainstem Reflexes: Pupils Shine a light directly into each eye individually, observing the direct response of the pupil as well as the consensual response of the other pupil. In the ER or ICU setting (i.e. a comatose patient), it sometimes helps to dim the lights of the room, or turn them out entirely during the exam, to increase the contrast and be sure that there is no light response. Brainstem Reflexes: Corneals The corneal reflex has an afferent and efferent component as well. The afferent limb is carried by branches of the 5th cranial nerve, which carries sensation from the cornea back towards the brain/brainstem. The efferent limb is carried by the 7th cranial nerve, which directs the eyelid “blink” in response to the stimulus. Its presence, even if only on one side, is not consistent with diagnosis of brain death. Brainstem Reflexes: Corneals In the ER or ICU setting, you may need to hold the eyelid(s) open. Use a small piece of cotton, the corner of a 2x2, etc., and gently touch the cornea (repeat for other eye). Look very closely for any response (sometimes it is very subtle). Avoid touching the eyelashes, as you may inadvertently move the lid and think you’ve seen a response when there was none. Brainstem Reflex: Doll’s Eye The Oculocephalic, or “Doll’s Eye” reflex, is mediated by unconscious brainstem pathways that work to keep your eyes focused on a point or target during movement of your head. The easiest way to think about it is this: When your head moves one way, your CNS produces eye movement in the opposite direction in order to keep whatever image you’re viewing “locked in place” on the retina. Brainstem Reflexes: Doll’s Eye To check the Oculocephalic reflex, turn the patient’s head rapidly to one side and check to see if the eyes move in response. For example, if you check a patient with a NORMAL Doll’s Eye reflex who is laying on a stretcher and staring at the ceiling, turning the patient’s head to the left should cause the patient’s eyes to look to the right in an attempt to remain focused on the ceiling. Brainstem Reflexes: Doll’s Eye Note: This test should be avoided in the setting of a patient with questionable stability of the cervical spine (i.e. in a trauma setting where cervical spine injury has not yet been ruled out). Brainstem Reflexes: Cold Calorics The oculovestibular reflex (i.e., “cold calorics”) is an excellent tool to assess the vestibular pathways in a patient with an uncleared cervical spine. This is performed by injecting cold water into the ear canal(s) for 20-30 seconds. Cold Calorics The head of the patient should be elevated to ~30 degrees. Infuse cold water into each ear canal separately for 20-30 seconds, observing the eyes for any response both during and immediately after the infusion of water. Any ocular movement in response to this test indicates residual brainstem function, and is inconsistent with brain death. Cold Calorics Note: This test should be avoided in the setting of a patient with possible CSF leak (i.e. a trauma setting where a patient has sustained a significant traumatic brain injury and there is blood/fluid leaking out of one or both ears). Brainstem reflexes: Cough/Gag Deep endotracheal suctioning and gentle manipulation (without dislodging it or changing its position) of the endotracheal tube are good ways to evaluate a patient’s cough/gag reflex. Presence of the cough and/or gag reflexes indicates persistence of the glossopharyngeal and vagal systems and is inconsistent with the diagnosis of brain death. Apnea Test The Apnea Test has become a key component in the determination of brain death. Understand: If ANY prior component of your clinical exam is inconsistent with brain death and/or any criteria for determination of brain death is not met, it is inappropriate to perform an Apnea Test. Thus, the Apnea Test is often the “last straw” in the clinical determination of brain death. Apnea Test The logic of the Apnea Test is based upon hypercarbia being a significant driving force for respiration. Thus, in the presence of significant hypercarbia ( > 60 mm Hg), if there is absence of respiratory effort, a diagnosis of brain death is supported. Apnea Test According to the American Academy of Neurology, the following represents the recommended protocol for performing an apnea test… Apnea Test Prerequisites Normal core body temperature Systolic Blood Pressure > 90 Normal PaCO2 (~35-45 mm Hg) So, draw ABG right before starting the test. Absence of any other underlying conditions that could confound diagnosis by mimicing brain death or suppressing respiratory drive Performing the Apnea Test Pre-oxygenate with 100% Oxygen for 30 min. Connect a pulse-ox, then disconnect ventilator. Place a nasal cannula at the level of the carina; give 100% Oxygen at 8L/min. during test. Watch closely for respiratory movements (any abdominal or chest movement that represents respiratory effort) Draw ABG ~10 minutes and reconnect ventilator. Interpreting the test The apnea test is POSITIVE (i.e., supports the diagnosis of brain death) if: There are no respiratory efforts during the test AND Repeat ABG shows PCO2 > 60 mm Hg. Interpreting the test The apnea test is INDETERMINATE if: after 10 minutes, the patient demonstrates no respiratory effort, but the PCO2 is < 60 mm Hg. The apnea test is NEGATIVE (i.e., does NOT support the diagnosis of brain death) if: the patient demonstrates any respiratory effort at any time during the test. Cease the test and reconnect the ventilator immediately upon observing respiratory effort. The Apnea Test If the patient becomes unstable at any point during the Apnea Test (i.e. SBP drops less than 90, significant desaturation on pulse-oximetry, observance of cardiac arrhythmias, etc.), the test should be aborted. The Apnea Test should not “induce a code!” Final Thought Remember that the clinical exam is the cornerstone of brain death determination, and there is no test or substitute for an examiner’s judgment and skills.