Neurology MCQs - Helen Nightingale
advertisement
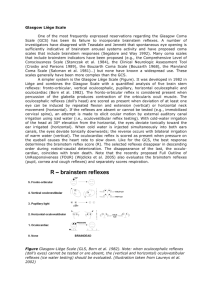
Neurology Questions Dr Helen Nightingale Correct stems highlighted in bold Question 1 Which of the following are true about confirming brainstem death? 1. 2. 3. 4. 5. There should be absence of pupil responses There should be no plantar responses The oculo-vestibular reflexes should be absent There should be no cough reflex It should be undertaken by one doctor who has been qualified for more than five year Extended answer According to the academy of royal colleges to confirm brainstem death there should be: No brain-stem reflexes Fixed pupils which do not respond to “ sharp changes” in light intensity No corneal reflex No oculo-vestibular reflex This test involves the slow injection into each external auditory meatus of (at least) 50mls of ice cold water. It is essential that there is clear access to the tympanic membranes and the head should be at 30o . An intact brainstem response would elicit nystagmuss with fast movements away from the injected ear. In brainstem death no response is seen. No cranial nerve motor responses Central (or peripheral) painful stimuli would normally produce a response in the cranial nerve territory - this is not the case in brainstem death. No cough or gag response No chest movement in response to hypercapnia – the apnoea test This should only be performed if the other tests are consistent with brainstem death. The patient is preoxygenated with 100% oxygen for 10 minutes to achieve a PCO2 of > 5 kPa. The patient is then disconnected from the ventilator but 6 L/min of oxygen is still deliveryed by the endotracheal tube. The pCO2 should then rise to > 6.65 kPa. If there are no chest movements this confirms brainstem death. The patient can then be again attached to the ventilator. This must be carried out by 2 or more medical practitioners who have been registered for more than 5 years. At least one must be a consultant and they must be competent in undertaking and interoperating brain-stem testing. Please see the link below for more information http://www.bts.org.uk/Documents/A%20CODE%20OF%20PRACTICE%20FO R%20THE%20DIAGNOSIS%20AND%20CONFIRMATION%20OF%20DEAT H.pdf Question 2 A 40-year-old woman is admitted to A+E with a 4-day history of progressive lower limb and numbness. She is normally fit and well apart from vomiting and diarrhoea for a few days 9-10 days ago. Which of the following investigations would help you make the diagnosis? 1. Lumbar puncture 2. Nerve conduction studies 3. CT brain 4. MRI Brain 5. Autoantibodies Extended answer This history is consistent with Gullian Barre syndrome (GBS). GBS is an acute onset usually demyelinating (but sometimes axonal) motor polyneuropathy with prominent proximal weakness. This tends to be preceded by sensory symptoms. Typically this starts distally and ascends unlike its variant Miller Fisher syndrome. Miller Fisher syndrome is associated with GQ1b antibodies and comprises of ataxia, opthalmoplegia, reduced reflexes with spared power in the limbs. Prior to the onset of GBS patients have often experienced in the preceding 12 weeks a (generally) mild illness such as an URTI or D+V. Known triggers include: Campylobacter jejuni HIV CMV EBV Mycoplasma species Investigations include: Autoantibodies: o GM1 is associated with a worse prognosis o GQ1B associated with Miller-Fisher variant CSF o Usually acellular with raised protein Nerve conduction studies o Usually show demyelination although some patients have axonal loss Serology for campylobacter jejuni Pulmonary function tests may show a reduced forced vital capacity Question 3 You are placed on a neurology ward and are watching the registrar examine one of the patients. You observe that the patient has bilateral extensor plantar responses but absent ankle reflexes bilaterally. What is the differential diagnosis for this finding? 1. 2. 3. 4. 5. Friedreich’s ataxia Parkinsons disease Middle cerebral artery infarct Motor neuron disease Wilson’s disease Extended answer This is a classical examination question any of the following would be potential options: • Subacute combined degeneration of the spinal cord • motor neurone disease • Syphilitic tabo-paresis • Friedreich's ataxia • A lesion at the conus medullaris or cauda equina lesion • Multiple sclerosis • Niacin deficiency • Stroke + diabetic neuropathy Question 4 A 23-year-old male economics study is admitted to your hospital whilst he was on his Easter break from University. He doesn’t really seem his normal self and has not been sleeping. His father has seen him crying a few times. He has also been unsteady on his feet and has started to talk like “he is drunk” and this morning wet himself. What is this most likely diagnosis? Schizophrenia Wilson’s disease Variant CJD Alcoholism Multiple sclerosis Extended Answer Variant Creutzfeldt-Jakob Disease tends to affect younger patients that the sporadic form. It is caused by a prion protein, which undergoes posttranslational modification into beta sheets. These accumulate in neurones ultimately leading to cell death. Typical features include those describe in the history a more comprehensive list is given below: Ataxia and dysarthria Psychiatric disturbance and insomnia Sensory disturbance Myoclonus and involuntary movements Dysphagia Urinary incontinence Immobility, mutism and cortical blindness occur in the late stages. Question 5 You are in the neurology outpatient clinic and meet a 40-year-old man known to have myotonic dystrophy. Which of the below are typical of the genetic of this condition? 1. 2. 3. 4. 5. Autosomal recession inheritance Autosomal dominant inheritance Exhibits anticipation X-linked inheritance Located on the X chromosome Extended answer Myotonic dystrophy is an autosomal dominant disorder, which is caused by a trinucleotide repeat (AGC) located on chromosome 19. With each successive generation the number of repeats and thus the severity of the disease may increase this is termed anticipation.