The Aging Egg: is there any solution? A critical review of causes
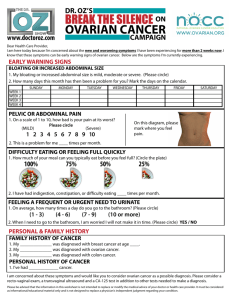
advertisement

The Spectrum of Ovarian “Aging”: From birth to menopause Etiologies and treatment strategies Amber R. Cooper MD, MSCI Disclosures • No relevant financial disclosures Objectives • Understand the decline in oocyte quality and quantity across a woman’s lifespan • Differentiate between normal and pathologic ovarian “aging” • Discuss potential treatment strategies for women with ovarian “aging” who desire pregnancy The Ovary • The human enigma • Structure discovered early, normal and abnormal function remain elusive Salvador Dali, 1929 • “Ovarian Aging” • Natural • Pathogenic Natural Ovarian Aging • Differs from somatic aging (and testicular aging) • We tend to focus on the oocyte…but the follicular unit may be equally important • Age at menopause has a high heritable component • Twin and Mother/daughter studies • Individual variability exists in initial follicle pool, rate of depletion, and age at menopause Clinical Spectrum of Natural & Pathologic Ovarian Aging Recurrent pregnancy loss Fertile Infertility Ovarian aging Diminished ovarian reserve Primary ovarian insufficiency Early menopause Menopause Oocyte Pool Quantity vs. Quality Fixed Pool; peaks at 5-6 mill 80% lost by birth 500,000 Modified from: Speroff. Clinical Gynecologic Endocrinology and Infertility. 7th ed. 25,000 1,000 Declining Oocyte Quantity Originally thought to be a simple exponential decline in number (in the reproductive years) Mattison DR. Dixon (ed). Reprod Toxicol 1985 Block E. Acta Anat 1952 Most ultimately believed bi-exponential model of decline Concept of critical mass (25,000) Magical age of “37-37.5” Faddy MJ Hum Reprod 1992 In reality, more like a constant increasing rate of loss than a magical number Hansen K R et al. Hum Reprod 2008 Oocyte Quality = Age (and maybe a little AMH?) The Impact of Female Age Alone (vs. Behavior) Marital fertility rates by 5-year age groups in specific populations ACOG and ASRM Practice Guideline. Fertil Steril 2008 The Impact of Female Age Alone •French Study of Female Fecundity •2193 nulliparous women with azoospermic men •Donor Inseminations in 11 centers •Cumulative success rates after 12 cycles •30 years of age or younger: 74% •31-35 years old: 61% •Over 35 years: 54% Schwartz D, Mayaux MJ. NEJM 1982; 306 (7): 404. Why does fertility decline with age? Ovarian aging *** Increased aneuploidy *** Endometrial aging Behavioral changes Increased incidences of other infertility-related conditions (fibroids, tubal disease, endometriosis, etc) Increased exposure to iatrogenic and environmental cytotoxic agents Normal Reproductive Aging Regular menses does NOT imply normal fertility Societal and Behavioral Shifts… Ovarian Aging Reproductive Delay Advancing Technology Demand for “Female Fertility Testing” The term “ovarian reserve” “Describes a woman’s reproductive potential with respect to ovarian follicle number and oocyte quality” ASRM Practice Committee Aging and Infertility in Women 2006 “A term that is used to determine the capacity of the ovary to provide eggs that are capable of fertilization resulting in a healthy and successful pregnancy” Wikipedia Measuring ‘Ovarian Reserve’ Term coined to predict oocyte yield and outcomes in IVF; Individualize therapies; Not perfect Serum assays FSH, Estradiol, Inhibin B Anti-Müllerian Hormone (AMH) US measurements Antral follicle count (AFC) Ovarian volume Dynamic Tests Which population are we talking about? All females Women Delaying Conception Infertility IVF Antimüllerian Hormone: AMH • Hot topic of ovarian reserve screens • Produced by granulosa cells of 2-6 mm follicles • indirectly reflecting remaining primordial pool • Seen as the “recruitment regulator” • Diminishes with age; often undetectable 5+ years before menopause • Not cycle day specific • Beware of assay, storage and handling variability • Elevated in PCOS patients • Influenced by BMI and hormonal contraception Is AMH Nonlinear? Anti-müllerian hormone (AMH) nomogram, based on a quadratic model of log(AMH) on age Nelson. AMH age nomogram. Fertil Steril 2010. Antral follicle count (AFC) Widely used ultrasound measure of ovarian reserve Transvaginal, early follicular phase best studied Probably the best predictor of ovarian response to stimulation Thresholds for a low AFC definition vary Most use the combined number of 2-9 or 2-10 mm follicles on each ovary There is an age-related decline in AFC High AFC may have predictive value also 10 y/o girl Abnormal ovarian aging… Ovarian Insufficiency • Probable mechanisms • Reduced oocyte pool • Accelerated follicular atresia • Alterations in follicular processes ** The oocyte is vulnerable in its state of arrest in meiosis I** • Cumulative exposure ?? Iatrogenic (Surgery, toxic therapies Environmental (EDC, tobacco) Autoimmune Genetic/Epigenetic • Nuclear • mtDNA Idiopathic Phenotypes of Ovarian Insufficiency DOR POI Cooper AR, Covington SN, Nelson, LM. Primary ovarian insufficiency (POI). In: Santoro N, et. al. ed. Amenorrhea: A Case-based clinical guide. Humana Press, c2011. Nelson LM. Clinical practice. Primary ovarian insufficiency. N Engl J Med 2009;360:606-14. Primary Ovarian Insufficiency (POI) Premature ovarian failure vs Primary ovarian insufficiency Not a dichotomous state Much more like a continuum Unlike natural menopause Ovarian function is unpredictable 5-10% may still conceive Accelerated physiologic aging or pathologic reduction through other mechanisms? Spontaneous POI 90+% remain idiopathic Other etiologies have been proposed 2% FMR1 premutation (0.7% early menopause; 0.4% controls) 4% possible steroidogenic cell autoimmune mechanism Abnormal karyotypes Primary amenorrhea (~10% POI): 50-60% Secondary amenorrhea: 5-15% Other rare genetic mechanisms (e.g. WRN, GALT, FOXL2) 10-20% may have familial component Associated with autoimmune diseases (thyroid and adrenal) Nelson L. NEJM 2009 van Kasteren et al Hum Reprod 1999 Murray et at. Genet Med 2014; Voorhuis Hum Reprod 2013 “Diminished ovarian reserve” (DOR) • Less severe phenotype than POI or different pathologic process? • No clear consensus definition despite hundreds of publications Ferraretti et al. Hum Reprod 2011 ESHRE: Defines the poor responder Need 2 of 3: (i) advanced maternal age or any other risk factor for Poor Ovarian Reserve (ii) a previous POR (iii) an abnormal ovarian reserve test (ORT). Using a stricter definition helps create a more crisp and reliable results from research Hum Reprod. 2011;The Bologna criteria Ovarian “responsiveness” vs “aging” • Could reduced ovarian “responsiveness” be part of the aging process? • Could glycosylation of FSH play a role? Jiang et al. JCEM 2015 • Or is the ovary itself the master regulator of the aging process? X chromosome and Ovarian Aging Turner syndrome-ovarian dysgenesis in 85-90% Critical regions Xp11.2-22.1 Xq26-q28; Xq13-q21 Deletions at/distal to Xq21 usually secondary amenorrhea/POI Smaller deletions Xq27-q28 may just have early menopause Several other candidate genes Rizzolio et al Hum Reprod 2006 and 2007; Spatz et al Nature Rev 2004 Adapted from Spatz et al. Nature Reviews 2004 Meiosis is critical to oocyte development Adapted from Marston and Amon, Nature Reviews Molec Cell Bio 2005 • Homologue pairing and recombination is vital. • Probably-pairing along the whole X chromosomes in order to make viable oocytes… • Examples: • The mule • The seedless watermelon Genetics of Ovarian Aging Polygenic and Multifactorial Complex trait • Genetic/Heritability • Environmental A number of genes throughout the genome have a suggested role in ovarian function Past POI studies identified some candidate genes through FISH/PCR; few through array, linkage, or GWAS • All small • Lack power to detect genes with smaller effect sizes • Most focus on common variants not rare The Environment and Ovarian Aging • Smoking • 1 to 1.5 years earlier menopause • Obesity? • Endocrine disrupting chemicals • Our recent study found an association between 15 EDCs and earlier menopause; 2-4 years earlier • 9 PCBs, 3 pesticides, 1 dioxin and 2 phthalates • Cumulative exposure??? Grindler N, Allsworth J, Macones G, Kannan K, Roehl K, Cooper AR (2015) PLOS One Cytotoxic Therapies and ovarian damage May be temporary The majority of past studies focus on the risk of POF/POI or azoospermia Many women have diminished ovarian reserve despite normal menses Best estimates-risk of infertility 40-80% in females 30-75% in males Depends on age, cancer site, treatment type and dose and pretreatment fertility Lee S et al. J Clin Oncol 2006.; Schover L et al. Cancer 1999.; Sonmezer M and Oktay. Oncologist 2006.; Wallace W et al. Lancet Oncol 2005. ASCO guide: Permanent amenorrhea risk Lee S et al. J Clin Oncol 2006. Treatment effects on fertility Ovarian reserve biomarkers have allowed for further investigation in survivors Women with childhood cancer therapies show diminished ovarian reserve despite regular cycles AMH and AFC most promising markers Bath L et al. Hum Reprod 2003. Larsen et al. Hum Reprod 2003. AMH in cancer survivors: Dose-dependent decline Gracia et al. Fertil Steril 2012. Can we intervene? Intervention vs Prevention • Awareness is key!!! • Understanding the etiologies is the first step towards prevention • Need for better diagnostic tests to intervene prior to cessation of function •Fertility preservation options at an earlier age Nutrition and Ovarian Aging • Diet • Composition (fat/carbs) • Omega 6:3 fats ratio • Caffeine • Antioxidants • Obesity? • Alcohol, Tobacco • Exercise/Relaxation • Supplements • Environmental exposures… Oxidative stress • Reproductive aging associated with oxidative stress • Sources vary: illness, inflammation, smoking, alcohol, other processes, ?obesity/diet • May damage an already fragile aging oocyte or alter the follicular quality • In turn may affect fertilization and embryo growth processes • Antioxidants: Vitamins (A, C, E), nuts/seeds, fruits/vegetables (5+ servings), herbs (ginger, tumeric, cloves, cinnamon, oregano) • Recent Cochrane review would suggest data still lacking and poor DHEA • Metabolic intermediate Androgen Estrogen • Intrafollicular IGF-1 (potentiates gonadotropins?) • Own biologic affect? • Possibly improves oocyte quality, LBR in poor responders • DHEA(S) levels decline with age • JCEM 2013 RCT (China): 16 weeks 25 mg TID in POI patients (vs placebo), AMH primary outcome • Kara 2014: DHEA 12 weeks RCT IVF ICSI showed no increased preg rate. Casson 2005, Wiser 2010, Yeung et al 2013 JCEM; Kara 2014Eur J Ostet Gynecol Reprod Biol Co-enzyme Q10 • Important for cell energetics (mitochondrial) • Antioxidant • Past “youth drug” used in many subspecialties • Oocyte energetics Embryo quality • Study: Patients with more CoQ10 in follicular fluid at the time of IVF-more mature oocytes and better quality embryos (Turi et al; 2012) • Less aneuploidy too? (Casper’s data) • Best estimate: 600 mg/day Oocyte/Follicle development (not really a “monthly” process) Antral follicle recruitment Gougeon. Hum Reprod 1986 Other supplements • Myo-inositol (B-complex vitamin) • Myo + Melatonin antioxidant combo? • L-arginine amino acid? Mixed data • Vitamin D deficiencies and IVF? • Selenium? • Media supplements or patient diet? • Most stopped at retrieval, Duration needed for use to see effect unclear Ovarian aging and Tailored IVF Protocols • Priming with OCPs? • Less drug and days of FSH? • Priming with Estradiol? • Decreased cancellation? More oocytes? Increased PR? • Priming with Testosterone? • Increased sensitivity to FSH, oocytes, IR, PR, LBR? Ovarian aging and Tailored IVF Protocols • Stimulation regimen • Antagonist better? Or most equal? • “Mild” or “Mini” IVF-cost effective and patient friendly but data on benefit still lacking • Adding GH? …May be value; meta-analyses show co-treatment improves outcome (PR/LBR); ? Quality or endometrial improvement rather than response Ovarian aging and Tailored IVF Protocols • Oocyte retrieval • Delaying hCG trigger 0.5-1 hour? Reichman DE et al. Fertil Steril 2011 • FSH “boost” with hCG ? Lamb JD et al. Fertil Steril 2011 • Aneuploid screening? • Time-lapse photography? Future Intervention? Experimental options: Ovarian fragmentation / In vitro activation study; Kawamura et al Ovascience technology Augment; Ovature/OvaPrime “Ovarian Age” = AGE + Ovarian Reserve (oocyte quantity) “Reproductive Age” = Genetics (Epigenetics) AGE + Environment Transcriptome Ovarian Health THANK YOU!