Natural History of Schizophrenia
advertisement
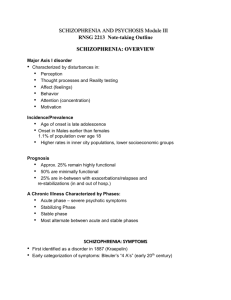
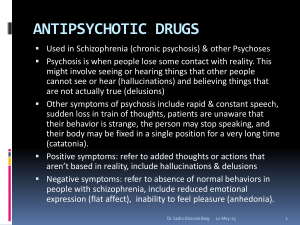
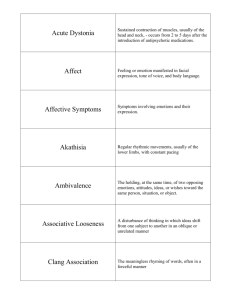
Adapted from: Treatment of Schizophrenia (and Related Psychotic Disorders) Scott Stroup, MD, MPH 2004 Psychosis • Generally equated with positive symptoms and disorganized or bizarre speech/behavior • Impaired “reality testing” • A syndrome present in many illnesses – remove known cause or treat underlying illness – treat symptomatically with antipsychotic medications Schizophrenia is a heterogeneous illness • Defined by a constellation of symptoms, including psychosis • Multifactorial etiology, variable course • Social/occupational dysfunction a required diagnostic criterion • Good treatment must address symptoms and social/occupational dysfunction DSM-IV Schizophrenia • 2 or more of the following for most of 1 month: – – – – – Delusions Hallucinations Disorganized speech Grossly disorganized or catatonic behavior Negative symptoms • Social/occupational dysfunction • Duration of at least 6 months • Not schizoaffective disorder or a mood disorder with psychotic features • Not due to substance abuse or a general medical disorder Features of Schizophrenia Positive symptoms Delusions Hallucinations Functional Impairments Work/school Interpersonal relationships Self-care Cognitive deficits Attention Memory Verbal fluency Executive function (eg, abstraction) Disorganization Speech Behavior Negative symptoms Anhedonia Affective flattening Avolition Social withdrawal Alogia Mood symptoms Depression/Anxiety Aggression/Hostility Suicidality Common needs of people with schizophrenia • • • • • • Symptom control Housing Income Work Social skills Treatment of comorbid conditions Challenges in the Treatment of Schizophrenia • • • • • • • Stigma Impaired “insight”– no agreement on problem Treatment “compliance” Substance abuse very common Violence risk Suicide risk Medical problems common, often unrecognized Schizophrenia Treatment • Therapeutic Goals • minimize symptoms • minimize medication side effects • prevent relapse • maximize function • “recovery” • Types of Treatment • pharmacotherapy • psychosocial/psychotherapeutic Treatments for schizophrenia: Strong evidence for effectiveness • Antipsychotic medications • Family psychoeducation • Assertive Community Treatment (ACT teams) The First Modern Antipsychotic Chlorpromazine (Thorazine) • Antipsychotic properties discovered in 1952 • Studied originally for usefulness as a sedative • Found to be useful in controlling agitation in patients with schizophrenia • Introduced in U.S. in 1953 Show Video Tape Augustine The Dopamine Hypothesis of Schizophrenia • All conventional antipsychotics block the dopamine D2 receptor • Dopamine enhancing drugs can induce psychosis (e.g., chronic amphetamine use) “Typical” antipsychotic medications (aka first-generation, conventional, neuroleptics, major tranquilizers) • High Potency (2-20 mg/day) (haloperidol, fluphenazine) • Mid Potency (10-100 mg/day) (loxapine, perphenazine) • Low Potency (300-800+ mg/day) (chlorpromazine, thioridizine) Dopamine blockade effects • Limbic and frontal cortical regions: antipsychotic effect • Basal ganglia: Extrapyramidal side effects (EPS) • Hypothalamic-pituitary axis: hyperprolactinemia Typical Antipsychotic limitation: Extrapyramidal side effects (EPS) • • • • Parkinsonism Akathisia Dystonia Tardive dyskinesia (TD)-- the worst form of EPS-- involuntary movements Parkinsonian side effects • Rigidity, tremor, bradykinesia, masklike facies • Management: – Lower antipsychotic dose if feasible – Change to different drug (i.e., to an atypical antipsychotic) – Anticholinergic medicines: • benztropine (Cogentin) • trihexylphenidine (Artane) Akathisia • Restlessness, pacing, fidgeting; subjective jitteriness; associated with suicide • Resembles psychotic agitation, agitated depression • Management: – lower antipsychotic dose if feasible – Change to different drug (i.e., to an atypical antipsychotic) – Adjunctive medicines: • propanolol (or another beta-blocker) • benztropine (Cogentin) • benzodiazepines Acute dystonia • Muscle spasm: oculogyric crisis, torticollis, opisthotonis, tongue protrusion • Dramatic and painful • Treat with intramuscular (or IV) diphenhydramine (Benadryl) or benztropine (Cogentin) Tardive Dyskinesia (TD) • Involuntary movements, often choreoathetoid • Often begins with tongue or digits, progresses to face, limbs, trunk • Etiologic mechanism unclear • Incidence about 3% per year with typical antipsychotics – Higher incidence in elderly Show Tardive Dyskinesia Videotape Abnormal Involuntary Movement Scale (AIMS) training tape Neuroleptic Malignant Syndrome (NMS) • Fever, muscle rigidity, autonomic instability, delirium • Muscle breakdown indicated by increased CK • Rare, but life threatening • Risk factors include: – High doses, high potency drugs, parenteral administration • Management: – stop antipsychotic, supportive measures (IV fluids, cooling blankets, bromocriptine, dantrolene) Typical Antipsychotic limitation: Other common side effects • Anticholinergic side effects: dry mouth, constipation, blurry vision, tachycardia • Orthostatic hypotension (adrenergic) • Sedation (antihistamine effect) • Weight gain • “Neuroleptic dysphoria” Typical Antipsychotic limitation: Treatment Resistance • Poor treatment response in 30% of treated patients • Incomplete treatment response in an additional 30% or more