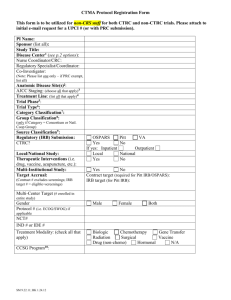
Materials and methods
advertisement

Characteristics of submucosal gastric carcinoma with lymph node metastatic disease H J Son, S Y Song,1 S Kim,3 J H Noh,2 T S Sohn,2 D S Kim1 & J C Rhee Histopathology 2005, 46, 158–165. Presented by intern 張家維 Introduction 2nd most common cause of cancer deaths East Asia and south America Korea and Japan early detection Early Gastric Carcinoma Mucosa or Submucosa 5-year survival rate Lymph node metastasis prognosis, submucosal invasion Introduction Depth of submucosal layer viaries The depth of submucosal gastric carcinoma (SMGC) Lymph node metastasis macroscopic appearance, location, size, tumor area, differentiation, invasion depth, submucosal vascularity, fibrosis near the tumor area Age- and Sex- matched Materials and methods Sampling: 248 patients SMGC Surgical resection Samsung Medical Centre (Seoul, Korea) 1995/Jan.~ 2002/Oct. Total 917 patients SMGC 124 LN metastasis (13.5%) Anticancer therapy X Evidence of metastatic disease X Materials and methods 124 SMGC with LN metastasis 124 SMGC without LN metastasis Age- and Sex- matched Specimens routinely examined 10% formalin Embedded in paraffin H & E stained Materials and methods Macroscopic: Japanese Endoscopic Society Classification Elevated, Depressed, Flat Microscopic: Lauren classification Materials and methods Depth of submucosal invasion 1.Ocular lens scale, distance between the lower edge of the muscularis mucosa and the deepest invading front of the tumor cells 2.sm3 method: sm1, sm2, sm3 3.sm2 method: smi , sme Materials and methods Tumor size Longest dimension of the tumor area Tumor area Longest dimension X its prependicular counterpart Tumor vessels vessels with a smooth muscle coat in the submucosa Materials and methods Statistical analysis: Log linear model, McNemar’s test, A paired t-test, Wilcoxon’s signed rank test P-value < 0.05 statistically significant SAS, version 6.12 Results Pathological parameters and lymphnode metastatic disease 124 SMGC with lymph node metastasis 69 males (55.6%), 55 females (44.4%) 31~83 y/o, the mean age 56.3 y/o The main locations of the tumors 60 lower, 61 middle, 3 upper 1/3 Tumor size 5~125 mm, the mean = 45 mm Tumor area 0.8~105.0 cm2, the mean = 17.1 cm2 Results Pathological parameters and lymphnode metastatic disease The gross types of the tumors 35 elevated (28.2%), 85 depressed (68.5%), 4 flat (3.2%) The histological differentiations (Lauren’s) 53 intestinal (42.7%), 65 diffuse (52.8), 6 mixed (4.8%) 111 N1 (89.5%), 13 N2 (10.5%) Results Pathological parameters and lymphnode metastatic disease Significantly associated with node-positive SMGC 1. presence of lymphatic tumor emboli 2. a larger tumor area 3. a larger tumor size 4. a non-flat gross type 5. an increased vascularity No significant relationship 1. location 2. Lauren classification 3. tumor related fibrosis Results Depth-related parameters and lymph node metastatic disease Ocular scale-measured depth 1. proved to have a significant correlation with node-positive SMGC 2. superficial invasive, deeply invasive (2mm) The sm3 method not well correlated The sm2 method not well correlated Results Multivariate analyses for possible indicators of LN metastatic disease Multivariate logistic regression analysis location, gross type, Lauren’s classification, lymphatic tumor emboli, increased vascularity, tumor-related fibrosis, tumor size, depth (sm2 method) The incidence of lymph node metastatic disease increased in the presence of lymphatic tumor emboli and in the tumors that invaded more than half of the submucosal layer Discussion EGC, the “early” horrible disaster curable disease early diagnosis and treatment programs The term of EGC has 2 innate defect 1. lymph node metastatic diseases 2. discriminate submucosal tumor call invasion 5-year survival rate 93~99% for node-negative EGC 73~90% for node-positive EGC 90~100% for intramucosal confinement 73~90% for submucosal invasion Discussion The treatment now for EGC conducting minimally invasive surgical procedures endoscopic mucosal resection, laparoscopic partial resection need careful and intensively subclassification Remove all metastatic lymph nodes ? chance of a cure↓ Factors related to lymph node metastatic disease Discussion SMGC lymph node metastasis rate 10~25% 917 SMGC in this tiral 13.5% LN metastasis The parameters related to LN metastasis lymphatic tumor emboli (uni- or multi- variate analysis) depth-related (accurate invasion depth, sm2 method) Discussion The best way to represent a submucosal tumor invasion Tsuchiya et al. = sm3 not appropriate for classifying tumor from endoscopic biopsy specimen Yasuda et al. = accurately the depth submucosal tumor invasion of locally resected tumor > 300μm gastrectomy + LN dissection Japanese Classification of Gastric Cancer criteria (0.5mm) depth of submucosal tumor invasion < 0.5mm sm1 depth of submucosal tumor invasion > 0.5mm sm2 Discussion Univariate analysis accurate depth of tumor invasion Multivariate analysis relative depth of tumor invasion Both accurate depth and relative depth of tumor invasion are important in predicting LN metastasis of SMGC A small group of superficial submucosal tumor invasions (even <1mm) presented LN metasitasis Discussion In general, EGC with LN metastasis large, depressed growth (or ulcer), poorly differentiated adenocarcinoma associated with peptic ulceration Tumor size contact with submucosal lymphatics and venules Vascularity higher incidence in node-positive SMGC LN metastasis might be associated with tumor cells coming into contact with submucosal lymphatic and venules Discussion Lymphatic tumor invasion and deeper tumor invasion into the submucosa simple and easy parameters for predicting LN metastasis from limited surgery specimens Small group of superficial involvement of submucosa LN metastasis Carefully selected patients for minimalizing operation Pathologist should carefully investigate the lymphatic invasion and the depth of tmor invasion Characteristics of intramucosal gastric carcinoma with lymph node metastatic disease S Y Song, S Park,2 S Kim,3 H J Son1 & J C Rhee1 Presented by intern 張家維 Results macroscopic appearance location size differentiation presence of ulceration vascularity presence of gastritis cystica profunda-like glandular proliferation disruption of the muscularis mucosae and invasion into the muscularis mucosae Results diffuse type histology (P < 0.001) and deep invasion into the muscularis mucosae (P < 0.05) were indicators of node-positive intramucosal EGCs Conclusions These histological indicators are easily accessible and seem to predict lymph node metastatic disease in limited surgical specimens. Patients should be carefully selected despite the recent trend toward less invasive resection of EGCs, especially for those apparently confined to the mucosa. Thank you for your attention