Collaborative Prospective Studies of Cardiovascular Disease
advertisement

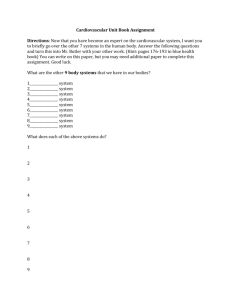
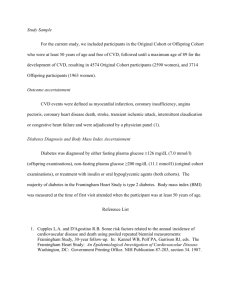
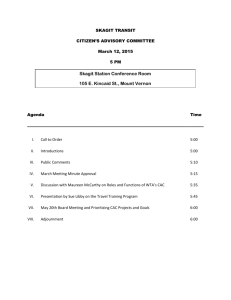
Collaborative Prospective Studies of Cardiovascular Disease Nathan D. Wong, PhD Professor and Director Heart Disease Prevention Program, Division of Cardiology Objectives • Understand the design and structure of the major ongoing NIH and CDC-supported prospective epidemiologic studies of cardiovascular disease • Understand opportunities for research projects and collaboration for residents, cardiology fellows, and faculty. Framingham Heart Study • Longest running study of cardiovascular disease in the world • Began in 1948 with original cohort of 5,209 subjects aged 30-62 at baseline • Biennial examinations, still ongoing, most of original cohort deceased • Offspring cohort of 5,124 of children of original cohort enrolled in 1971, and more recently and still being enrolled to better understand genetic components of CVD risk are up to 3,500 grandchildren of the original cohort. • Routine surveillance of cardiovascular disease events adjudicated by panel of physicians Measurements • Standard risk factors since inception of study, except HDL-C began around 1970. • Serial ECGs (first to document high rate of unrecognized MIs) • M-mode echocardiograms in 1980’s, first large study to show prognostic importance of increased LV mass • Newer measures done in subsets include: Carotid ultrasound, bone denistometry, coronary artery calcium, and other novel risk factors and biomarkers (e.g. natriuretic peptides) Framingham Most Significant Milestones • 1960 Cigarette smoking found to increase the risk of heart disease • 1961 Cholesterol level, blood pressure, and electrocardiogram abnormalities found to increase the risk of heart disease • 1967 Physical activity found to reduce the risk of heart disease and obesity to increase the risk of heart disease • 1970 High blood pressure found to increase the risk of stroke • 1976 Menopause found to increase the risk of heart disease • 1978 Psychosocial factors found to affect heart disease • 1988 High levels of HDL cholesterol found to reduce risk of death • 1994 Enlarged left ventricle (one of two lower chambers of the heart) shown to increase the risk of stroke • 1996 Progression from hypertension to heart failure described ____________________________________________________________ Smoking Statement Issued in 1956 by American Heart Association ___________________________________________________________ “It is the belief of the committee that much greater knowledge is needed before any conclusions can be drawn concerning relationships between smoking and death rates from coronary heart disease. The acquisition of such knowledge may well require the use of techniques and research methods that have not ___________________________________________________________ hitherto been applied to this problem.” CHD Risk by Cigarette Smoking. Filter Vs. Non-filter. Framingham Study. Men <55 Yrs. 14-yr. Rate/1000 250 Non-Smoker Reg. Cig. Smoker Filter Cig. Smoker 200 206 210 150 100 210 119 112 50 59 0 Total CHD Myocardial Infarction 9 Doubts about cholesterol as late as 1989 Relative Risk of CHD by HDL and LDLCholesterol Men 50-70 Years of Age Framingham Study 4-Year Follow-up, The Framingham Study Morbidity Ratio: 3.5 25 mg/dl 3 55 mg/dl 2.5 85 mg/dl 1.9 2 1.5 1.2 1 1 0.5 2.9 0.6 0.4 0.1 0.2 0.3 100 mg/dl 160 mg/dl 220 mg/dl 0 LDL-Cholesterol WB Kannel Am Heart J. 1985;110:1100-1107. Risk factors for long-term coronary prognosis after initial myocardial infarction: the Framingham Study. Wong ND, Cupples LA, Ostfeld AM, Levy D, Kannel WB. Am J Epidemiol. 1989 Sep;130(3):469-80. Links • Age-adjusted analyses showed the risk of reinfarction to be positively associated with blood pressure and serum cholesterol. Risk of coronary death was strongly associated with blood sugar level, systolic blood pressure, serum cholesterol, heart rate, diabetes, and interim reinfarction. In multivariable analyses, systolic pressure, serum cholesterol, and diabetes were predictive of reinfarction; relative weight was inversely associated with reinfarction. Systolic pressure, serum cholesterol, and the prevalence of diabetes persisted as independent predictors of coronary death. When adjustments were made for the effects of these variables, women were at only half the risk of coronary death compared with men. _______________________________________________________________________________ Lifetime Risk of CHD Increases with Serum Cholesterol ___________________________________________________________________________ 60 50 Cholesterol <200 mg 200-239 mg 57 >240 mg Percent 40 44 30 34 29 20 33 19 10 0 Men Women Framingham Study: Subjects age 40 years DM Lloyd-Jones et al Arch Intern Med 2003; 1966-1972 ________________________________________________________ CK Friedberg on Hypertension: Diseases of the Heart 1996 ___________________________________________________________ “There is a lack of correlation in most cases between the severity and duration of hypertension and development of cardiac complications.” _______________________________________________________________ Relation of Non-Hypertensive Blood Pressure to Cardiovascular Disease Vasan R, et al. N Engl J Med 2001; 345:1291-1297 10-year Age- Adjusted Cumulative Incidence 12% Hazard Ratio* <120/80 mm Hg 120-129/80-84 mm Hg 130-139/85-89 mm Hg 10% SBP 10.1 8% 7.6 6% 2% 4.4 2.8 1.9 0% Women 1.0 1.5 2.5 1.0 1.3 1.6 H.R. adjusted for age, BMI, Cholesterol, Diabetes and smoking *P<.001 5.8 4% <120/80 120-129 130-139 Women Men Men Framingham Study: Subjects Ages 35-90 yrs. Risk of Myocardial Infarction with Isolated Systolic Hypertension Annual Incidence Per 10,000 Framingham Study 24 Yr. Follow-Up WB Kannel Prev Cardiol 1998; 1:32-39 Men ages 45-54 yrs. Joint Influences of SBP and Pulse Pressure on CHD Risk Franklin SS….Wong ND et al, Circulation 1999 Franklin SS et al. Circulation. 1999;100:354-360. Franklin SS, Lopez VA, Wong ND, et al. Single Versus Combined Blood Pressure Components and Risk for Cardiovascular Disease. The Framingham Heart Study. Circulation Jan 2009 • • BACKGROUND: -The utility of single versus combined blood pressure (BP) components in predicting cardiovascular disease (CVD) events is not established. We compared systolic BP (SBP) and diastolic BP (DBP) versus pulse pressure (PP) and mean arterial pressure (MAP) combined and each of these 4 BP components alone in predicting CVD events. Methods and Results-In participants in the original (n=4760) and offspring (n=4897) Framingham Heart Study who were free of CVD events and BP-lowering therapy, 1439 CVD events occurred over serial 4-year intervals from 1952 to 2001. In pooled logistic regression with the use of BP categories, combining SBP with DBP and PP with MAP improved model fit compared with individual BP components (P<0.05 to P<0.0001). Significant interactions were noted between SBP and DBP (P=0.02) and between PP and MAP (P=0.01) in their respective multivariable models. Models with continuous variables for SBP+DBP and PP+MAP proved identical in predicting CVD events (Akaike Information Criteria=10 625 for both). Addition of a quadratic DBP(2) term to DBP and SBP further improved fit (P=0.0016). • Conclusions-Combining PP with MAP and SBP with DBP produced models that were superior to single BP components for predicting CVD, and the extent of CVD risk varied with the level of each BP component. The combination of PP+MAP (unlike SBP+DBP) has a monotonic relation with risk and may provide greater insight into hemodynamics of altered arterial stiffness versus impaired peripheral resistance but is not superior to SBP+DBP in predicting CVD events. Diseases of The Heart Charles K Friedberg MD, WB Saunders Co. Philadelphia, 1949 “The proper control of diabetes is obviously desirable even though there is uncertainty as to whether coronary atherosclerosis is more frequent or severe in the uncontrolled diabetic” ________________________________________________________________ ______________________________________________________________ Risk of Cardiovascular Events in Diabetics Framingham Study _________________________________________________________________ Age-adjusted Cardiovascular Event Coronary Disease Stroke Peripheral Artery Dis. Cardiac Failure All CVD Events Biennial Rate Age-adjusted Per 1000 Risk Ratio Men Women Men Women 39 21 1.5** 2.2*** 15 6 2.9*** 2.6*** 18 18 3.4*** 6.4*** 23 21 4.4*** 7.8*** 76 65 2.2*** 3.7*** _________________________________________________________________ Subjects 35-64 36-year Follow-up **P<.001,***P<.0001 Risk of Coronary Heart Disease by Diabetic Status According to Level of Risk Factors Framingham Study 60 Wilson PWF, Kannel WB. Nutr. In Clin Care 1998 57.7 Women age 50 yrs. 50 Nondiabetic Diabetic 44.9 40 % 29.7 30 20 16.5 12.9 10 10 5.9 1.8 3.5 5.2 6.8 3 0 Risk Factors HBP (160) Chol (240) Cig Smoker HDL-C (34) ECG-LVH No (120) No (165) No No (58) No Yes No No No No Yes Yes No No No Yes Yes Yes No No Yes Yes Yes Yes No Yes Yes Yes Yes Yes _______________________________________________________________ CVD Risk Imposed by ECG-LVH Framingham Study 36-yr. Follow_______________________________________________________________ up Age-adjusted Risk Excess Risk Rate per 1000 Ratio per 1000 Age Men Women Men Women Men Women 35-64 164 135 4.7*** 7.4*** 129 117 _____________________________________________________________ 65-94 234 235 2.8*** 4.1*** 151 178 Biennial Rate per 1000. CVD=CHD, stroke, peripheral vascular disease, heart failure ***P<0.001 _____________________________________________________________ CVD Risk by Plasma Natriuretic _______________________________________________________________ Peptides Multivariate Hazard Ratio per SD Increment Outcome BNP N-ANP Death 1.27 (1.06-1.52)** 1.41 (1.14-1.74)*** Major CVD 1.28 (1.03-1.59)* 1.30 (1.02-1.67)* Heart Failure 1.77 (1.31-2.41)*** 1.94 (1.37-2.75)*** AF 1.66 (1.30-2.11)*** 1.72 (1.302.28)*** Stroke/TIA 1.53 (1.16-2.02) ** 1.37 (0.99-1.89) CHD 1.10 (0.89-1.37) 1.12 (0.88-1.42) Framingham Offspring Study Obesity-promoted natriuretic peptides are secreted from cardiomyocytes: They play a fundamental role in CV remodeling, volume homeostasis, and response to ischemia. TJ Wang et al. N Engl J Med 2004; 350:655-663. ____________________________________________________________ Lifetime Risk of Coronary Heart Disease in the Framingham Study ______________________________________________________________ Men At age 40 years: 48.6% At age 70 years: 34.9% Women 31.7% 24.2% _________________________________________________________________ Lloyd-Jones et al. Lancet 1999; 353:89-92 Cardiovascular Health Study • 5,201 Medicare eligible individuals aged 65-102 at baseline enrolled beginning 1992 at six field centers. • Assessment of newer and older risk factors. • Ongoing follow-up of cardiovascular events and mortality • Subclinical disease measures included: – carotid B-mode ultrasound for carotid IMT at Year 2, Year 7, and Year 11 – m-mode echocardiographic measures of left ventricular mass and dimensions, left atrial dimension done at baseline (Year 2) (at UC Irvine) and follow-up (Year 7) examinations. – Ankle brachial index (ABI) for measurement of PAD – Pulmonary function (FVC and FEV1) Procedure BAS E Call B YR 3 Call 3 YR 4 Call 4 Tracking Update X X X X X X Stressful Life Events X X X X X X Depression Scale X X X Quality of Life X X X Social Support and Network X X X Medications - Prescription X X X Physical Function: ADL/IADL X X Cognitive Function MMSE X OTC 3MSE Digit Symbol Substitution X X X X X X X X X Benton Visual Retention Phlebotomy X Anthropometry - Weight X Standing Height X Waist Circumference X Hip Circumference X Arm Span X Procedure BAS E Call B YR 3 Call 3 YR 4 Bioelectric Impedance X Seated Blood Pressure X Performance Measures: 15-ft Walk X X Chair Stands X X Grip Strength X X X Finger Tapping X X Nutrition X Resting 12-Lead ECG X Physical Activity X Supine Ankle-Arm Blood Pressure X Orthostatic Blood Pressure X Vascular Ultrasound Carotid X X X Aortic Pulmonary Function X Peak Flow Six-Minute Walk/Oximetry Holter Monitor X Cerebral MRI Echocardiography Spot Urine Collection X X Call 4 Procedure YR 5 Call 5 YR 6 Call 6 YR 7 Call 7 Tracking Update X X X X X X Stressful Life Events X X X X Depression Scale X X X X Quality of Life X X X X Social Support and Network X X Medications Prescription X X X X X X X OTC Physical Function: ADL/IADL X X X X YR 8 X X X X X Cognitive Function MMSE 3MSE Digit Symbol Substitution X X X X X X X X X X X ch ol ch ol opt Benton Visual Retention Phlebotomy X Procedure YR 5 Call 5 YR 6 Call 6 YR 7 Call 7 YR 8 Seated Blood Pressure X X X casu al Performance Measures: 15ft Walk X X X X Chair Stands X X Grip Strength X X X X Finger Tapping X X X X X Nutrition X Resting 12-Lead ECG X Physical Activity X Supine Ankle-Arm Blood Pressure X Orthostatic Blood Pressure X Vascular Ultrasound Carotid X Aortic X X X Pulmonary Function X Peak Flow X Six-Minute Walk/Oximetry Holter Monitor Cerebral MRI X (X X) Echocardiography X Bone Density/Body Composition X X Summary of Events • Combined Cohort at Baseline (N=5888) • Mean Age = 72 years 58% Women 16% African American 31% had Cardiovascular Disease at entry Number of Events through June 30, 2002 • Angina 1064 • MI 696 • Heart Failure 1262 • Claudication 789 • Stroke 789 • TIA 212 • Death 2658 Cardiovascular Health Study: Combined intimal-medial thickness predicts total MI and stroke Cardiovascular Health Study (CHS) (aged 65+): MI or stroke rate 25% over 7 years in those at highest quintile of combined IMT (O’Leary et al. 1999) Ankle Brachial Index as a Predictor of Cardiovascular Mortality in the CHS Study Newman A et al ATVB 1999 CHS Representative Recent Publications • Association of carotid artery intima-media thickness, plaques, and C-reactive protein with future cardiovascular disease and all-cause mortality: the Cardiovascular Health Study. Circulation. 1;116 (3238). 7-3-2007 • Brachial Flow-Mediated Dilation Predicts Incident Cardiovascular Events in Older Adults. The Cardiovascular Health Study. Circulation. 4-23-2007 • Relationship between brachial flow-mediated dilation and carotid intima-media thickness in an elderly cohort: The Cardiovascular Health Study. Atherosclerosis. 9-3-2007 CHS publications continued • The association of alcohol consumption and incident heart failure: the Cardiovascular Health Study. J Am Coll.Cardiol. 2;48 (305-311). 7-18-2006 • Usefulness of aortic root dimension in persons > or = 65 years of age in predicting heart failure, stroke, cardiovascular mortality, all-cause mortality and acute myocardial infarction (from the Cardiovascular Health Study). Am J Cardiol. 2;97 (270-275). 1-15-2006 • Left atrial volume, geometry, and function in systolic and diastolic heart failure of persons >/=65 years of age (the cardiovascular health study). Am.J.Cardiol. 1;97 (83-89). 1-1-2006 CHS publications (continued) • Blood pressure level and outcomes in adults aged 65 and older with prior ischemic stroke. J Am Geriatr Soc. 9;54 (1309-1316). 2006 • 10-year follow-up of subclinical cardiovascular disease and risk of coronary heart disease in the Cardiovascular Health Study. Arch.Intern.Med. 1;166 (71-78). 1-9-2006 • Metabolic syndrome and cardiovascular disease in older people: The cardiovascular health study. J Am Geriatr Soc. 9;54 (1317-1324). 2006 • Mortality and cardiovascular risk across the anklearm index spectrum: results from the Cardiovascular Health Study. Circulation. 3;113 (388-393). 1-242006 CHS publications (cont.) • The association of microalbuminuria with clinical cardiovascular disease and subclinical atherosclerosis in the elderly: The Cardiovascular Health Study. Atherosclerosis. 10-19-2005 • Increased left ventricular mass is a risk factor for the development of a depressed left ventricular ejection fraction within five years: the Cardiovascular Health Study. J.Am.Coll.Cardiol. 12;43 (2207-2215). 6-16-2004 • The association between lipid levels and the risks of incident myocardial infarction, stroke, and total mortality: The Cardiovascular Health Study. J.Am.Geriatr.Soc. 10;52 (1639-1647). 2004 Possible Topics for Future Papers • Prognosis associated with echo left atrial dimension—e.g., in relation to stroke • Papers examining relation of progression of LV mass in relation to future risk of cardiovascular events (CHD, CHF, stroke) • Predictors of progression of LV mass • Combination of increased CIMT and LV mass in relation to CHF or CHD events. Multiethnic Study of Atherosclerosis • 6,814 adults aged 45-80 enrolled at 6 field centers, including Caucasians, African-Americans, Hispanics, and Chinese beginning 2000. • Extensive assessment of standard and novel risk factors, unique blood cohort among 1000 subjects. • Multiple evaluations of carotid IMT, ABI, and coronary calcium. Ancillary studies of LV size and extracoronary measures of calcification (HarborUCLA) and abdominal aortic calcium (UC San Diego) in full or partial cohorts. MESA Study Design Features Four examinations approximately two years apart, exam 4 just completed Major risk factors measured at each exam Coronary calcium measured in entire cohort at Exam 1, ½ cohort at Exam 2, ½ cohort at Exam 3, and in about 1000 pts in Exam 4. Carotid IMT measured at Exam 1 and 2-3. Cardiac MRI measured at Exam 1 and 2-3 Ankle Brachial Index Pulse wave analysis Endothelial function measures Follow-up for CVD events and incident DM, mortality MESA Key Subclinical Disease Measures • Coronary calcium Agatston score and volume • LV size, thoracic aortic calcium, aortic valve calcium (ancillary study) • Abdominal aortic calcium (ancillary study), including aortic diameter • Ankle brachial index • ECG variables (LVH, Q-waves, long QT, AFIB) • Carotid Ultrasound (Common and Internal CIMT, max carotid stenosis) • Cardiac MRI (LV end diastolic mass, volumes, LVEF, stroke volume, aortic distensibility, cardiac output) MESA laboratory variables • Glucose, insulin, TG, HDL (including 8 subfractions), LDL (incl very small to large subfractions), mean LDL and HDL size, • Urinary albumin, creatinine, microalbuminuria, homocysteine • CD40 ligand, E-selectin, IL-2, IL-6, HS-CRP, MMP3, 9, TNF-alpha, PAI-1, HSV, CMV, H.Pylori, C. Pneumoniae • CETP activity and mass, SI-cam, Ox-LDL, Ddimer Other MESA Variables • Family history of MI, stroke • Cigarette, cigar, pipe, and chewing tobacco • Total light, moderate, and vigorous physical activity in minutes/wk and MetS • Medications: Statins, Anti-arrhythmics by class, beta-blockers, CCBs, Cox2 inhibitors, estrogen replacement therapy, oral anticoagulants Cumulative Incidence of Any Coronary Event: MESA Study (Detrano et al., NEJM 2008) Risk Factor-Adjusted Hazard Ratios by Coronary Calcium Score: MESA Study (Detrano et al., NEJM 2008) MESA ongoing papers in progress here at UCI • Metabolic syndrome, diabetes, and progression of coronary calcium • Abdominal aortic calcification and systemic atherosclerosis (relation to CAC, CIMT, and ABI) • Value of CAC vs. CIMT in predicting CHD events over FRS in Metabolic Syndrome and Diabetes (with Dr. Malik) Multiethnic Study of Atherosclerosis (MESA): CAC and CHD Events (Malik, Wong et al, AHA Nov 2007) Adjusted Hazard Ratios No MetS/DM (HRs) (95% CI) (n= 3,800 ) MetS without DM (n =1,996) DM (n=1018 ) CHD Events 30 21 20 CAC 1-99 vs. 0 2.4 (0.6-9.2) 2.3 (0.4-14.1) 4.4 (0.9-21.5) CAC 100-399 vs. 0 9.7 (2.9-31.7) 11.2 (2.4-53.2) 5.2 (1.0-27.8) CAC 400+ vs. 0 13.6 (3.9-47.0) 8.2 (1.5-44.1) Adjusted for Framingham Risk Score and Ethnicity 6.8 (1.3-34.8) Multiethnic Study of Atherosclerosis (MESA): Common CIMT and CHD Events (Malik, Wong et al AHA Nov. 2007) Adjusted Hazard No MetS/DM MetS without Ratios (HRs) (95% CI) (n= 3,800 ) DM (n =1,996) DM (n=1018 ) CHD Events 30 20 CIMT 2nd quartile vs 1st quartile 0.8 (0.2-2.4) 0.5 (0.1-3.0) 2.1 (0.2-20.6) CIMT 3rd quartile vs 1st quartile 0.9 (0.3-2.7) 2.0 (0.6-7.5) 3.9 (0.5-32.2) CIMT 4th quartile vs 1st quartile 1.7 (0.6-4.7) 0.7 (0.2-3.1) 3.6 (0.5-28.3) 21 Adjusted for Framingham Risk Score and Ethnicity Results for Internal CIMT were similar. 1.00 ROC Curve Analyses for CVD Events: FRS alone, FRS plus CIMT, or FRS plus CAC in those with Mets (without DM): MESA Study (Malik, Wong et al., AHA 2007) 0.75 ROC FRS alone ROC FRS + CIMT 0.00 0.25 0.50 ROC FRS + CAC 0.00 0.25 0.50 1-Specificity FRS2 ROC area: 0.6967 CAC2 ROC area: 0.7539 0.75 1.00 CIMT2 ROC area: 0.6925 Reference ROC area FRS+CAC (0.7539) vs. FRS alone (0.6967), p = 0.0017 ROC area FRS + CIMT (0.6926) vs FRS alone (0.6967), p =0.6354 ROC area FRS+ CAC (0.7539) vs. FRS + CIMT (0.6925), p = 0.002 1.00 ROC Curve Analyses for CVD Events: FRS alone, FRS plus CIMT, or FRS plus CAC in those with DM: MESA Study (Malik, Wong et al., AHA 2007) 0.75 ROC FRS alone ROC FRS + CIMT 0.00 0.25 0.50 ROC FRS + CAC 0.00 0.25 0.50 1-Specificity FRS3 ROC area: 0.6669 CAC3 ROC area: 0.7285 0.75 1.00 CIMT3 ROC area: 0.6809 Reference ROC area FRS+CAC (0.7285) vs. FRS alone (0.6669), p = 0.0001 ROC area FRS + CIMT (0.6809) vs. FRS alone (0.6669), p =0.3258 ROC area FRS+ CAC (0.7285) vs. FRS + CIMT (0.6809), p = 0.0037 Incidence and Progression of Coronary Calcium (mean 2.4 years between scans): Multiethnic Study of Atherosclerosis (n=5570) (Wong et al., AHA 2006) P<0.01 to p<0.001 between each group 158 160 140 110 120 P<0.001 across groups 100 80 60 P<0.001 across groups 40 20 12 21 56 90 No MetS/DM MetS w/o DM DM 64 45 24 0 A. New CAC (%) B. Progression (%) C. Progression w/baseline CAC A. % with new CAC among those free of CAC at baseline B. % with progression of CAC (score change >0) C. Mean adjusted change in CAC score among those with CAC at baseline Abdominal Aortic Calcium (5cm from iliac bifurcation) Prevalence of AAC (>0), CAC (>0), ABI (<0.9), and common and internal IMT (>1mm) by Age in Men (Wong et al., AHA 2006) 96 Prevalence (%) 100 89 75 80 86 73 59 60 64 45.7 40 51 39 34 22 20 36 20 8 45-54 AAC 8 6 1 0 50 CAC 1 55-64 CCA-IMT 65-74 75-84 ICA-IMT ABI P<0.001 across age groups, n=971 (except 969 for common IMT) Prevalence of AAC (>0), CAC (>0), ABI (<0.9), and common and internal IMT (>1mm) by Age in Women (Wong et al., AHA 2006) Prevalence (%) 100 93 88 76 80 67 60 50 55 42 49 34 40 20 26 24 14 14 1 0 13 11 6 45-54 AAC 39 CAC 3 1 55-64 CCA-IMT 65-74 75-84 ICA-IMT P<0.001 across age groups (n=933 except 931 for common IMT) ABI Prevalence of CAC, Increased CIMT, and Low ABI by Presence of AAC – Men (Wong et al., AHA 2006) 70 70 Prevalence (%) 60 48 50 40 30 28 30 20 11 11 10 4.2 0 0 CAC CCA-IMT No AAC ICA-IMT Any AAC Prevalence of CAC >0, CCA-IMT or ICA-IMT >1mm, or ABI <0.9 P<0.001 for those with vs. without AAC for all measures ABI Prevalence of CAC, Increased CIMT, and Low ABI by Presence of AAC – Women (Wong et al., AHA 2006) 60 Prevalence (%) 51 50 42 40 30 20 23 11 10 6 10 1.4 3.8 0 CAC CCA-IMT No AAC ICA-IMT ABI Any AAC Prevalence of CAC >0, CCA-IMT or ICA-IMT >1mm, or ABI <0.9 P<0.001 for those with vs. without AAC for all measures except p=0.06 for ABI Counts of Events MI CHF Stroke Hard CHD All CHD All CVD Currently Available 73 74 59 91 165 230 Available 12/07 90 89 59 118 205 269 All recorded 91 90 59 119 210 274 Other possible ideas for papers • Hypertension and BP categories and progression of MRI LV mass or LVEF • Progression of CIMT vs. progression of MRI LV mass or LVEF • Alcohol intake and MRI LV dimensions, mass, and LVEF • LDL and HDL subfractions and subclinical atherosclerosis Other Prospective Epidemiologic Studies • Atherosclerosis Risk in Communities – approximately 10,000 adults aged 45-64 years, half African-American enrolled at 4 field centers, ongoing follow-up for CVD events and mortality • Epidemiology of Diabetes Interventions and Complications (EDIC) – Follow-up of original DCCT cohort of approximately 1,400 adults with Type 1 diabetes. Standard and novel risk factor assessments and measures of carotid IMT (2 measures), ABI, and coronary calcium by CT. Coronary Artery Risk Development in Young Adults (CARDIA) – 5,115 adults (half African-American) aged 18-30 at baseline in 1985 enrolled at 4 field centers. – Ongoing evaluation (Year 20 exam recently completed). – Echocardiographic M-mode and 2D measures available at Year 5 and Year 10 exams (UC Irvine Echo Reading Center) – CT Coronary Calcium at Years 15 (HarborUCLA) and 20 (Wake Forest University) Other Studies Antihypertensive Lipid-Lowering to Prevent Heart Attack Trial (ALLHAT) • Blood Pressure Control in Hispanics in the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. • Margolis KL, Piller LB, Ford CE, Henriquez MA, Cushman WC, Einhorn PT, Colon PJ Sr, Vidt DG, Christian R, Wong ND, Wright JT Jr, Goff DC Jr; Antihypertensive Lipid-Lowering Treatment to Prevent Heart Attack Trial Collaborative Research Group. Women’s Health Initiative Observational Study and Clinical Trial • Panic Attacks and Risk of Incident Cardiovascular Events Among Postmenopausal Women in the Women's Health Initiative Observational Study. • Smoller JW, Pollack MH, Wassertheil-Smoller S, Jackson RD, Oberman A, Wong ND, Sheps D. NHANES Cross-Sectional and Mortality Follow-up Studies • NHANES 2003-2004 (and 2005-2006 becoming available) cross-sectional health survey and clinic exam data • NHANES 3 Mortality Follow-up – Abdominal obesity and mortality from CHD, CVD, all-causes – Combined HTN – Dyslipidemia and mortality – Pulmonary function (% predicted FVC), Creactive protein, and mortality Distribution of HTN Subtypes in the untreated Hypertensive Population in NHANES III by Age ISH (SBP 140 mm Hg and DBP <90 mm Hg) SDH (SBP 140 mm Hg and DBP 90 mm Hg) IDH (SBP <140 mm Hg and DBP 90 mm Hg) 100 17% 16% <40 40-49 16% 20% 20% 11% 50-59 60-69 Age (y) 70-79 80+ 80 Frequency of hypertension 60 subtypes in all untreated 40 hypertensives (%) 20 0 Numbers at top of bars represent the overall percentage distribution of untreated hypertension by age. Franklin et al. Hypertension 2001;37: 869-874. Cardiovascular Disease (CVD) and Total Mortality: US Men and Women Ages 30-74 (age, gender, and risk-factor adjusted Cox regression) NHANES II Follow-Up (n=6255)(Malik and Wong, et al., Circulation 2004; 110: 12451250) 7 *** Relative Risk 6 *** 5 *** 4 *** *** *** 3 *** *** *** 2 * ** 1 0 CHD Mortality CVD Mortality Total Mortality * p<.05, ** p<.01, **** p<.0001 compared to none None MetS Diabetes CVD CVD+Diabetes Odds of CVD Stratified by CRP Levels in U.S. Persons (Malik and Wong et al., Diabetes Care 2005; 28: 690-3) 6 O d d s R a t i o *** 5 4 3 2 *** * * ** 1 0 High CRP No Metabolic disease Syndrome Low CRP Diabetes –*p<.05, **p<.01, **** p<.0001 compared to no disease, low CRP –CRP categories: >3 mg/l (High) and <3 mg/L (Low) –age, gender, and risk-factor adjusted logistic regression (n=6497) Diabetes Care 2008; 31: 1405-9 Estimated CHD Risk by Gender and Ethnicity (Hoang, Wong et al., Diabetes Care 2008) Control (all treated) (%) of HTN in US Adults, by Disease Status (Wong et al., Arch Intern Med 2007) Control of HTN (%) 100 80 60 64.6 * 63.7 61.2 49.3 48.8 ** 42.2 40 ** ** 46.7 50.3 34.9 20 0 No-Disease Dyslipidemia Mets DM CKD Stroke **P<0.05**P<0.01 when compared to No-Disease Group Control is in persons with HTN defined as BP < 140/90 If DM and CKD is based on BP<130/80 control is **35.3% and **23.2%, respectively. If MetS is based on BP<130/85 control is **46.7% CHF PAD CAD Mean BP and Distance to Goal Among HTN Pts Not at Goal (Wong et al., Arch Intern Med 2007) No Disease Dyslipidemia MetS DM CKD Stroke CHF PAD CAD SBP mm Hg DBP mm Hg (Distance to Goal) (Distance to Goal) 154 (14) 93 (3) 154 (19) 90* (7) 154 (16) 94 149* (14) 87** (6) 155 (18) 87** (7**) 155 (22*) 87** (6) 154 (22**) 89** (6) 157 (23**) 89* (7) 155 (21*) 90 (5) (6) Minimum BP distance from goal of < 140/90 in parenthesis, even with DM & CKD *p<0.05 **p<0.01 compared to no disease UCI Heart Disease Prevention Program Resources • SAS and Stata Statistical Software and computing resources • Affiliated faculty: Stanley Franklin, MD, FACC, John Zamarra, MD, FACC, and Shaista Malik, MD • Statistical Staff: Heli Ghandehari, Victor Lopez • Research Student Staff: Alejandro Perez, May Song, Vy Le