СL_Pharmacy_Pulmonology_2
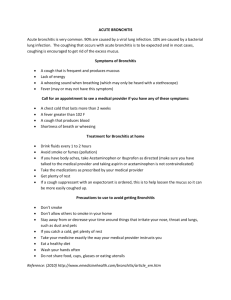
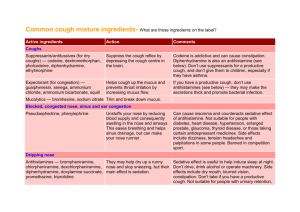
advertisement
• 1) Inflammation of the mucous membrane of the bronchial tubes 2) asthmatic bronchitis, bronchitis which causes or aggravates bronchospasm. 3) chronic bronchitis, a condition of the bronchial tree characterized by cough, hypersecretion of mucus, and expectoration of sputum over a long period of time, associated with frequent bronchial infection; usually due to inhalation, over a prolonged period, of air contaminated by dust or by noxious gases of combustion. 4) Acute bronchitis is usually a short, severe illness that may show up along with a cold or follow other viral infections such as measles or whooping cough. • The top left illustration shows the normal pulmonary tree, while the lower right illustration at the bottom shows what happens during an attack of bronchitis. The inflammation of the bronchi and bronchial tubes produces a buildup of mucus. The thickened mucus forms a plug that can block bronchial tubes, the passages that carry air from the trachea (windpipe) to the alveoli (air sacs) of the lungs. This results in the difficult breathing characteristic of bronchitis • Routine antibiotic treatment of uncomplicated acute bronchitis is not recommended, regardless of duration of cough. If pertussis infection is suspected (an unusual circumstance), a diagnostic test should be performed and antimicrobial therapy initiated • Both bronchitis and pneumonia are serious diseases affecting the lower respiratory tract. They can lead to a lot of discomforts and, if left untreated, may cause other serious conditions. There are a number of differences between the two. • Pneumonia manifests itself in the • Bronchitis manifests itself form of high fever, cough and as a cough with headache, chills. It is accompanied by rapid breathing and a certain amount of chills and a slight fever. A wheezing. The patient often patient may also experience complains of chest pain. Some a shortness of breath. patients also feel extremely exhausted and nauseous. The symptoms of viral pneumonia often resemble those of ordinary flu. There are chills and high fever. It is often accompanied by chattering teeth. It may also produce sputum that is green, yellow or rust colored. Pneumonia becomes apparent when the patient experiences a shortness of breath. • The treatment for bronchitis is relatively simple. Once identified the reasons for the infection, a course of antibiotics will be administered. Patient will be advised rest and will need to avoid pollution and smoke. • Pneumonia is more of a serious affliction. If the patient have been diagnosed with this disease, will be prescribed a strong antiviral or antibiotics. If the condition worsens, the patient may be hospitalized anywhere between one and three days, depending on the seriousness of condition. Medications: • Dozens of antibiotics are available for treating pneumonia, but selecting the best drug is sometimes difficult. Patients with pneumonia need an antibiotic that is effective against the organism causing the disease. When the organism is unknown, "empiric therapy" is given, meaning the doctor chooses which antibiotic is likely to work based on factors such as the patient's age, health, and severity of the illness. • Joint guidelines issued in 2007 by the Infectious Disease Society of America and the American Thoracic Society (ITSA/ATS) recommend that mild CAP in otherwise healthy patients be treated with oral macrolide antibiotics (azithromycin, clarithromycin, or erythromycin). • Many patients with heart disease, kidney disease, diabetes, or other co-existing conditions may still be treated as outpatients. However, they should be given a fluoroquinolone (moxifloxacin, gemifloxacin, or levofloxacin) or a beta-lactam (preferably high-dose amoxicillin or amoxicillin-clavulanate), plus a macrolide, unless they live in an area with high S. pneumoniae resistance to macrolides. • • There are not as many choices for treating viral pneumonia. Oseltamivir (Tamiflu) and zanamivir (Relenza) have been the recommended drugs for influenza A or B infections, but many strains of influenza A have become resistant. Their use is only recommended if they are started in the first 48 hours of symptoms. Taken early, these medications may be effective in reducing symptoms and duration of illness. • Patients with viral pneumonias are at risk for what are called "superinfections," which generally refers to a secondary bacterial infection, usually caused by S. pneumoniae, S. aureus, or H. influenzae. Doctors most commonly recommend treatment with amoxicillin-clavulanate, cefpodoxime, cefprozil, cefuroxime, or a respiratory fluoroquinolone if these secondary infections occur. • Patients with pneumonia caused by varicella-zoster and herpes simplex viruses are usually admitted to the hospital and treated with intravenous acyclovir for 7 days. • No antiviral drugs have been proven effective in adults with RSV, parainfluenza virus, adenovirus, metapneumovirus, the SARS coronavirus, or hantavirus. Treatment is largely supportive, with patients receiving oxygen and ventilator therapy as needed. • Treatment of RSV in Children. Ribavarin is the first treatment approved for RSV pneumonia, although it has only modest benefits. The American Academy of Pediatrics recommends this drug for children who are at high risk for serious complications of RSV. Expectorants, more accurately known as bronchomucotropic agents, are drugs used to assist in the removal of secretions or exudate from the trachea, bronchi, or lungs. They act by liquifying viscid mucus or mucopurulent exudates, i.e., they are decongestants. Therefore, they are used in the treatment of coughs to help expel these exudates and secretions. Antitussives are agents that specifically inhibit or suppress the act of coughing. They should not be used to suppress productive cough ing. Expectorants and antitussives are most commonly used in the symptomatic treatment of the common cold or bronchitis. • Coughing is the forceful expulsion of air from the lungs. A cough may be productive or nonproductive. With a productive cough, secretions from the lower respiratory tract are expelled. A nonproductive cough is a dry, hacking one that produces no secretions. An antitussive is a drug used to relieve coughing. Many antitussive drugs are combined with another drug, such as an antihistamine or expectorant, and sold as nonprescription cough medicine. Other antitussives, either alone or in combination with other drugs, are available by prescription only. ACTIONS Some antitussives depress the cough center located in the medulla and are called centrally acting drugs. Codeine and dextromethorphan are examples of centrally acting antitussives. Other antitussives are peripherally acting drugs, which act by anesthetizing stretch receptors in the respiratory passages, thereby decreasing coughing. An example of a peripherally acting antitussive is benzonatate (Tessalon), libexin. USES Antitussives are used to relieve a nonproductive cough.When the cough is productive of sputum, it should be treated by the primary health care provider who, based on a physical examination, may or may not prescribe or recommend an antitussive. ADVERSE REACTIONS Use of codeine may result in respiratory depression, euphoria, lightheadedness, sedation, nausea, vomiting,and hypersensitivity reactions. The more common adverse reactions associated with the antitussives When used as directed, nonprescription cough medicines containing two or more ingredients have few adverse reactions. However, those that contain an antihistamine may cause drowsiness. CONTRAINDICATIONS Antitussives are contraindicated in patients with known hypersensitivity to the drugs. The narcotic antitussives (those with codeine) are contraindicated in premature infants or during labor when delivery of a premature infant is anticipated. Codeine is a Pregnancy Category C drug except in the pregnant woman at term or when taken for extended periods, when it is considered a Pregnancy Category D drug. • Classification: 一.Central antitussives 1. Dependent central antitussives 2. Independent central antitussives 二.Peripheral antitussives • Opioid alkaloids. • Morphine is the most effective drug for the suppression of cough, but have addiction. • Mechanism: suppressing of cough center • Selectively suppress cough center in medulla oblongata • Potency: • Suppression of cough: ≈1/10 of morphine • Analgesia: ≈1/7 of morphine • Respiratory depression, constipation, tolerance, dependence < that of morphine • Pharmacokinetics: • Well absorbed from oral and injection. • 10% converted to morphine through demethylation • Clinical Uses: • Dry cough • Adverse Reactions: • Respiratory suppression in high dose; • Tolerance and physical dependence with frequently repeated administration; • Suppress secretion of bronchial gland and movement of cilia. • • Stereoisomers of opioid molecules that are devoid of analgesic effects and addiction liability. Classification: 1) 2) 3) 4) 5) -orphan-antitussives : dextromethorphan amido-antitussives: pentoxyverine, clofedanol piperidine-antitussives: cloperastine morpholine-antitussives: promolate, fominoben; others: eprazinone, zipeprol. • Dextrorotatory stereoisomers of a methylated derivative of levorphanol • Clinical Use: • Dry cough. Often + Antihistamine drug • Suppression of cough: ≈1/3 of codeine. • Direct suppression of cough center • Atropine-like action and local anesthesia action. • Derivative of diphenhydramine • Suppression of cough center • Blocking H1-receptor • Inhibiting receptor, afferent nerve, efferent nerve of cough reflex arc → cough suppression. 1. 2. local anesthesia action: narcotine, benzonatate; Alleviative action: extractum glycyrrhizae liquidum, Syrup • • I. Mucokinetic drugs Classification: By the mechanism of action: 1. 2. Mucus secretagogue drugs: stimulating gastric mucosa → reflex secretion of bronchial gland↑ → dilution of sputum: ammonium chloride. Mucolytic drugs: 1) 2) 3) 4) break acid mucin: bromhexine drug-SH S-S of mucin → Fragmentation: acetylcysteine Enzymolysis: α-chymotrypsin Surfactant: tyloxapol----Fog inhalation