Mapping Professional Competencies: WGV
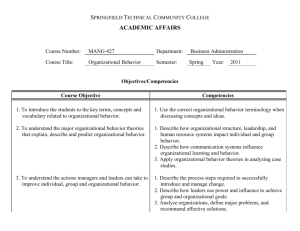
advertisement

From Learning Outcomes to Competencies EXBO: Brussels 11 July 2012 What is a Competency? Competencies encompass knowledge, skills, attitudes, and behaviours necessary for a particular set of tasks or objectives. Professional Competence is defined as ‘the array of abilities across multiple domains or aspects of professional performance in a certain context…is multidimensional and dynamic. It changes with time, experience and setting’. (Frank, 2010) A competent professional is one possessing the required abilities in all domains in a certain context at a defined stage of education or practice. Issues in Bio-Medical Education There is a perceived mismatch between graduates from health care professions and the health system needs. Why? : New roles, new demands, technology, evidence-based medicine, professional fragmentation, globalisation. Heightens the need for reform. Growing interest in outcomes-based education, with government/regulatory support. Change in educational practices in health professions education Outcomes-based/competency-based education improves performance, enhances communication, provides an impetus for faculty development, curricular reform and leadership in educational innovation. (IOM,2005) Competency-based education has begun to redefine accreditation and certification across the health professions. (Am.J.Pub Health, 2004) Traditional Vs Outcomes Based education TRADITIONAL EDUCATION OUTCOMES BASED EDUCATION Inputs are important Outcomes are important Time fixed Outcomes based Learners grouped in classes and move together Learners advance in various ways to achieve outcomes Teachers are responsible for a course Teachers are responsible for a set of outcomes Learners accumulate courses and grades leading to a credential Learners demonstrate achievement of outcomes at their own pace Defined competencies are important Defined competencies are fundamental Topics Outcomes based education: Why? How? Statement of competence and professional relevance Alignment of competencies: (IFAPP/CEPM/WGV Vs Faculty of Pharmaceutical Medicine Vs PharmaTrain Learning Outcomes-based) Competencies for Medicines Development Professionals / Clinical Investigators / Clinical Research Team: opportunities for synergies and collaboration Key messages Competency-Based Education (CBE) is here to stay Core Competencies for Pharmaceutical Physicians and Medicines Development Professionals have been defined for professional and education purposes A Statement of Competence is available for professional use The PharmaTrain Learning Outcomes and the Core Competencies (Cognitive level) are fully aligned Opportunities for development and collaboration of competencies in clinical research CBE well-suited to adult education, part-time, modular, learner-centred, multi-modal, flexible, international E&T programme. What is a ‘Competency’? Competencies encompass knowledge, skills, attitudes, and behaviours necessary for a particular set of tasks or objectives. Professional Competence is defined as “the array of abilities across multiple domains or aspects of professional performance in a certain context…is multidimensional and dynamic. It changes with time, experience and setting”. (Frank, 2010) A competent professional is one possessing the required abilities in all domains in a certain context at a defined stage of education or practice. Traditional Vs Competency based education Hierarchy of competencies Competencies in Pharmaceutical Medicine/Drug Development Sciences Professional Groups expect to have defined competencies. On the other hand, the stakeholders expect professional groups to have defined Competencies. PharmaTrain and E&T programmes in Pharmaceutical Medicine / MDS intend to be Outcomes-Based. Revision: The Previous Task: Align the proposed competencies (CEPM-WGV) with those from the Specialty Training Curriculum (FPM) and the Learning Outcomes from the PharmaTrain Curriculum. Restrictions/Boundaries: 6 or 7 domains Vs 12 domains < 10 general competencies for each domain Feasibility of mapping to the PharmaTrain syllabus /curriculum Maintain internal/external validity Prepare a Statement of Competence for professional purposes. BASE COURSE LEARNING OUTCOMES SYLLABUS TOPICS (KNOWLEDGE) LO1 LO2 APPLIED KNOWLEDGE SKILLS ATTITUDES PP/MDS COMPETENCY From Learning Outcomes to Competencies LOx Domain Benchmarking: I- Drug Development and Clinical Trials WGV-CEPM FPM PharmaTrain •Drug Discovery, Development & Clinical Pharmacology •Clinical Pharmacology •Discovery of Medicines & Development Planning •Clinical Research and Clinical Trials •Clinical Development •Non Clinical Testing, pharmaceutical & early clinical development •Statistics & Data Management •Exploratory & Confirmatory clinical development •Clinical Trials Domain Benchmarking: II- Regulatory Affairs and Safety of Medicines WGV-CEPM FPM •Medicines Regulation: Drug •Medicines Regulation safety & Pharmacovigilance PharmaTrain •Regulatory Affairs, Drug Safety & Pharmacovigilance •Drug Safety Surveillance •Ethics and Subject Protection • NA •NA Domain Benchmarking: III- Health Care and Professionalism WGV-CEPM FPM PharmaTrain •Health Care Market Place •Health Care Market Place •Healthcare Market Place: Economics of Health Care •Communication & Information in Health care •Interpersonal & Management Skills •NA •Leadership, Management & Professionalism Final proposal for consideration for Pharmaceutical Physicians /Medicines Development Professionals 3 AREAS 7 CORE DOMAINS Competence framework AREA 1. DRUG DEVELOPMENT & CLINICAL TRIALS CORE DOMAIN ( competencies) I Discovery of Medicines & Early Development (n=9) II Clinical Development & Clinical Trials (n=10) 2. REGULATORY AFFAIRS & SAFETY OF MEDICINES III Medicines Regulation (n=10) IV Drug Safety Surveillance (n=8) V 3. HEALTH CARE & PROFESSIONALISM Ethics & Subject Protection (7) VI Health Care Market Place (n=6) VII Communication & Management (n=9) Statement of Competence for: Pharmaceutical Physicians Medicines Development Professionals Statement of Competence: Sources PharmaTrain Curricula; Pharmaceutical Medicine Specialty Training Curriculum, Faculty of Pharmaceutical Medicine (FPM); Consortium of Academic Programs in Clinical Research (CoAPCR); US Accreditation Council for Graduate Medical Education (ACGME); American Society of Public Health (ASPH); Academy of Pharmaceutical Physicians & Investigators (APPI; now APCR); Clinical and Translational Science Awards/US National Institute of Health (CTSA); Medical Leadership Forum/Faculty of Pharmaceutical Medicine (MLF). I-The Pharmaceutical Physician/ Medicines Development Professional is able: To identify unmet therapeutic needs, evaluate the evidence for a new candidate for clinical development and design a Clinical Development Plan for a Target Product Profile. (Domain I) To design, execute & evaluate exploratory & confirmatory clinical trials and prepare manuscripts or reports for publication & regulatory submissions. (Domain II) II- The Pharmaceutical Physician/ Medicines Development Professional is able: To interpret effectively the regulatory requirements for the clinical development of a new drug through the product life-cycle to ensure its appropriate therapeutic use & proper risk management. (Domain III) To evaluate the choice, application & analysis of post-authorisation surveillance methods to meet the requirements of national/international agencies for proper information & risk minimisation to patients & clinical trial subjects. (Domain IV) III-The Pharmaceutical Physician/ Medicines Development Professional is able: To combine the principles of clinical research & business ethics for the conduct of clinical trials & commercial operations within the organisation. (Domain V) To appraise the pharmaceutical business activities in the healthcare environment to ensure that they remain appropriate, ethical & legal to keep the welfare of patients & subjects at the forefront of decision making in the promotion of medicines & design of clinical trials. (Domain VI) IV- The Pharmaceutical Physician/ Medicines Development Professional is able: To interpret the principles & practices of people management & leadership, using effective communication techniques & interpersonal skills to influence key stakeholders & achieve the scientific & business objectives. (Domain VII) Competencies by Domain Desired Competencies by Domain Cognitive Level (Bloom’s taxonomy) Mapping to PharmaTrain Learning Outcomes The desired competency (cognitive level) was mapped to the related PharmaTrain Learning Outcomes (as described in the Base Course curriculum) For Example……………………… Example of mapping competences to Learning Outcomes Desired Competency (Cognitive level) • Evaluates and analyses a disease area within the industry clinical development environment and identifies unmet therapeutic needs • Designs and executes confirmatory studies and evaluates the resulting data as applied to the CDP and the TPP Source FPM/CLD1 FPM/CLD4, SDM1 Related PharmaTrain Learning Outcome •Role of patho-physiology and molecular pharmacology in drug development (M1) •Principles of Translational research and its role in drug development (M1) •Function and elements (including business aspects) involved in the integrated development of a new drug (M1) •Principles and practices of Medical Marketing (M1a) Key operational and strategic issues in the clinical development plan (M4) Various types of clinical studies and the methods used to choose the appropriate design (M4) Main statistical methods used in clinical research (M4) Task was completed successfully! Aligned the proposed competencies (WGV-CEPM) with those from the Specialty Training Curriculum (FPM) and the learning outcomes from the PharmaTrain Curriculum 7 domains ~ 10 general competencies for each domain Mapped to the PharmaTrain Curriculum and Syllabus Maintained internal/external validity Prepared a Statement of Competence for professional purposes Conclusions Competency Based Education is here to stay. Core Competencies for Pharmaceutical Physicians and Medicines Development Professionals have been defined for professional and education purposes. A Statement of Competence is available for professional use. The PharmaTrain Learning Outcomes and the Core Competencies (Cognitive level) are aligned. Opportunities for development and collaboration of competencies in clinical research. Competence framework AREA 1. DRUG DEVELOPMENT & CLINICAL TRIALS CORE DOMAIN I DISCOVERY OF MEDICINES & EARLY DEVELOPMENT II CLINICAL DEVELOPMENT & CLINICAL TRIALS 2. REGULATORY AFFAIRS & SAFETY OF MEDICINES III MEDICINES REGULATION IV DRUG SAFETY SURVEILLANCE V 3. HEALTH CARE & PROFESSIONALISM ETHICS & SUBJECT PROTECTION VI HEALTH CARE MARKET PLACE VII COMMUNICATION & MANAGEMENT Competency achievement: On the successful completion of the module / programme / (interactive) course the Pharmaceutical Physician / Medicines Development Professional should be able to: >>>>>>>>>>> Competencies (Cognitive Level) Area 1: DRUG DEVELOPMENT & CLINICAL TRIALS Domain I: DISCOVERY OF MEDICINES & EARLY DEVELOPMENT Evaluate and analyse a disease area within the industry clinical development environment and identify unmet therapeutic needs. Evaluate the clinical and non-clinical pharmacology and toxicology evidence for a new candidate for clinical development. Evaluate and apply the regulatory and ethical aspects underpinning clinical development. Create a Clinical Development Plan for a new candidate including a Target Product Profile (TPP). Design and execute exploratory studies and evaluates the resulting data as applied to the Clinical Development Plan. Contrast the advances made in the clinical pharmacology of a new medicine in a stepwise manner with the overall Clinical Development Plan and the TPP. Defend the statistical principles for the design, conduct and assessment of exploratory studies. Justify the various end-points used in the clinical development programme. Appraise suspected adverse events during exploratory development. BASE COURSE LOs: 1. INTRODUCTORY MODULE & DEVELOPMENT PLANNING On successful completion of this Module the student should be able to: 1. Outline the process of drug development and identity of critical factors and decision points. 2. Explain the importance of the patient in drug development. 3. Describe the background to the development of the regulation of medicines and the role of the competent authorities. 4. Outline the monitoring of drug safety. 5. Describe the principles & practice of medical marketing. 6. Outline the role of pathophysiology and molecular biology-based pharmacology in drug development. 7. Describe the principal steps in discovering, modifying, assessing and patenting new chemical and biological compounds (including advanced therapies) according to their therapeutic indication. 8. Discuss the resource planning (in terms of project management, budgeting and cost-control) involved in the management of a drug development programme. 9. Describe the principles of translational research and its role in drug development. 10. Outline the functions and elements (including business aspects) involved in the integrated development of a new drug. BASE COURSE LOs: 2. NON-CLINICAL TESTING, PHARMACEUTICAL AND EARLY CLINICAL DEVELOPMENT On successful completion of this Module the student should be able to: 1. Discuss the choice & predictive value of the non-clinical testing programme as part of the overall drug development plan for chemical & biological compounds. 2. Describe the integration of non-clinical tests into the overall drug development plan (including scheduling of toxicology tests with respect to clinical trials). 3. Outline the steps in the pharmaceutical development of a drug substance and final drug product (including chemical and biological compounds). 4. Describe the planning of clinical trial supplies for test substance(s) and comparators (active and placebo). 5. Provide an overview of non-clinical study requirements prior to First-in-Man studies. 6. Discuss the molecular and cellular basis of toxic reactions. 7. Outline the principles and practical application of pharmacokinetics & toxicokinetics. 8. Outline the early exploratory development in man. 9. Discuss the principles of clinical pharmacology and their application to clinical development. 10. Describe the influence of genetic factors in drug development & drug response. Competencies (Cognitive Level) Area 1: DRUG DEVELOPMENT & CLINICAL TRIALS Domain II: CLINICAL DEVELOPMENT AND CLINICAL TRIALS Evaluate the conduct & management of clinical trials within the context of the Clinical Development Plan & working as part of a Team. Design & execute confirmatory studies and evaluate the resulting data as applied to the Clinical Development Plan & the TPP. Evaluate & interpret the principles for the development of a clinical trial protocol applying principles of GCP in clinical pharmacology. Summarise the principles of Case Record Form Design & clinical data management, including CDISC, EDC & MedDRA. Interpret & explain the outcomes of clinical studies. Support & provide the clinical input into the design & review of a Statistical Analysis Plan. Appraise & review relevant literature & other sources and write manuscripts for publication. Create & constructively evaluate clinical study reports & regulatory submissions. Appraise & design the management of essential documents as defined under GCP guidelines. Organise the activities & processes related to the selection & management of sites for individual or multi-centre clinical trials. Competencies (Cognitive Level) Area 2: DRUG DEVELOPMENT AND CLINICAL TRIALS Domain V: ETHICS AND SUBJECT PROTECTION Evaluate the impact of cultural diversity & the need for cultural competency in the conduct of clinical trials & other business activities . Describe the ethical & professional issues (conflicts of interest, plagiarism, authorship & intellectual property) associated with clinical research, drug development & commercialisation on the production of scientific knowledge. Describe the significance of historical abuses on the evolution of principles of human subject protection. Evaluate the key documents related to the ethical conduct of clinical trials & pharmaceutical marketing operations. Describe the ethical issues involved when dealing with vulnerable populations, and the need for additional safeguards. Compare the requirements for human subject protection & privacy under different national & international regulations. Summarise the principles of Corporate Social Responsibility. BASE COURSE LOs: 3. EXPLORATORY AND CONFIRMATORY CLINICAL DEVELOPMENT On successful completion of this Module the student should be able to: 1. Describe the early studies in patients: dose-finding / proof of concept studies and their impact on drug development plan. 2. Outline the design of clinical trials, including legal, regulatory, ethical & practical aspects and Good Clinical Practice (GCP). 3. Discuss the principles and application of statistics in clinical trials. 4. Describe the procedures for clinical trial data collection (paper & electronic) and data management (including validation processes) to ensure optimal quality data. 5. Identify the key strategic and operational issues in the clinical trial process, in terms of legislative requirements and Good Clinical Practice (GCP). 6. Describe the role of the Investigator Drug Brochure (IDB). 7. Discuss the principles and practical relevance of ethical issues in biomedical research. 8. Outline the legal and ethical provisions for protection of clinical trial subjects. BASE COURSE LOs: 4. CLINICAL TRIALS On successful completion of this Module the student should be able to: 1. Describe the various types of clinical studies & the methods used to choose the appropriate design. 2. Describe the main statistical methods used in clinical research. 3. Identify the key issues involved in the conduct of a clinical study including investigator & site recruitment, investigative site management & conflict resolution. 4. Discuss the collection, evaluation & reporting of adverse event data in clinical trials. 5. Outline the various quality management issues in clinical trials. 6. Describe the impact of emerging results on the drug development plan. 7. Outline the key operational and strategic issues in the clinical development plan. 8. Explain the evaluation of the outcome of drug development: final therapeutic profile / usage of a medicine. 9. Describe the role of the Target Product Profile (TPP) & Target Product Claims (TPC). 10. Explain the role of the Drug Safety Monitoring Board (DSMB) & other relevant study committees. 11. Discuss the statistical issues in statistical report writing. 12. Describe the evaluation & interpretation of clinical trial results. 13. Illustrate the principles & practical application of critical appraisal. Competencies (Cognitive Level) Area 2: REGULATORY AFFAIRS AND SAFETY OF MEDICINES Domain III: MEDICINES REGULATION Summarise the legislative framework supporting the development & registration of medicines, ensuring their safety, efficacy & quality. Describe the regulations related to post-authorisation safety monitoring & reporting procedures. Justify the significance of regular product Safety Update Reports to the regulatory agencies and participate in their preparation & review. Evaluate the unlicensed use of medicines and ensure patient safety is paramount. Describe procedures in the development & renewal of Marketing Authorisations. Design, prepare, review & evaluate Clinical Overviews for regulatory submission. Describe the legal framework for clinical trials and the requirements in different regions, and perceived problems associated with global drug development. Describe the mechanisms for wider availability of medicines, and undertake or contribute to product deregulation. Organise the investigation of product defects, counterfeit products and other miscellaneous pharmaceutical procedures and requirements. Describe the principles and process of regulation of medical devices and biotechnology formulations. Competencies (Cognitive Level) Area 2: REGULATORY AFFAIRS AND SAFETY OF MEDICINES Domain IV: DRUG SAFETY SURVEILLANCE Contrast the key regulatory requirements for pharmacovigilance, both in the major ICH regions & locally, and their historical background. Organise the medical assessments required to meet the requirements for drug safety reporting both at the level of the individual patient (case report) & aggregate report. Summarise the spontaneous reporting & signal detection methodologies & assess medically Adverse Event/Adverse Drug Reaction reports as part of causality assessment. Summarise the principles & methods of evaluation of risk & benefit balance & the principles & methods for managing risk to patient & clinical trial subjects. Discriminate the variety of regulatory actions possible to address concerns about patient safety. Describe the importance of communication of safety issues, the variety of formats required to meet audience needs and contribute to the development of such communications. Evaluate a safety issue and establish a crisis management team, recognising the key functional areas to be represented and their roles & responsibilities. Appraise the areas of progress, likely major advances & future challenges in drug safety & pharmacovigilance. BASE COURSE LOs: 5. REGULATORY AFFAIRS; DRUG SAFETY & PHARMACOVIGILANCE On successful completion of this Module the student should be able to: 1. Describe the general principles of medicines regulation (both pre- & post-approval) at EU & global level. 2. Discuss the impact of medicines legislative requirements on regulatory activities within a pharmaceutical company. 3. Explain the role of national agencies and international bodies in medicines regulation. 4. Describe the national provisions for management of: (1) off-label / unlicensed use of medicines, and (2) controlled drugs. 5. Discuss the place of the International Conference on Harmonisation (ICH) in medicines regulation (including Common Technical Document [CTD]). 6. Explain the regulatory processes in the EU / EEA areas. 7. Describe the regulation & legal considerations of Product Information. 8. Outline the principles & practical application of medical devices regulation. 9. Discuss the roles of the various stakeholders (including pharmaceutical and other healthcare professionals, investigators, regulatory authorities) in drug safety and pharmacovigilance. 10. Outline the classification of adverse events / adverse drug reactions. 11. Describe the safety reporting requirements (according to the type of adverse event / reaction) pre- & postapproval. 12. Discuss the ongoing management of drug safety issues pre- & post-approval (including Risk Management Plans [RMPs], Periodic Safety Update Reports [PSURs]); ongoing benefit / risk assessment throughout the life-cycle of a medicine. 13. Discuss the role of pharmacoepidemiology in the life-cycle management of a medicine. 14. Describe the factors influencing medication safety from the perspective of each stakeholder. Competencies (Cognitive Level) Area 3: HEALTHCARE AND PROFESSIONALISM Domain VI: HEALTHCARE MARKETPLACE Describe the commercial healthcare environment in which pharmaceutical medicine operates, identifying the contribution of laws & of regulators & other stakeholders in the decision making for prescribing medicines. Summarise the key elements involved in medical/marketing communication in the healthcare environment, and explainsthe importance of compliance with regulation in this context. Describe the pharmaceutical industry: internal environment, structure & function, key stakeholders & commercial drivers, and explain how these business elements impact on the broader healthcare market place. Describe the information required to undertake a commercial analysis of the market potential for a pharmaceutical product/candidate within the industry business environment. Appraise the commercial competitor environment when evaluating the opportunity for a new medicine under development or a currently marketed product. Describe the interface between pharmaceuticals & the external stakeholder environment, and the challenges balancing the commercial & professional aspects in making ethical judgments within the legal/regulatory framework . BASE COURSE LOs: 6. HEALTHCARE MARKETPLACE; ECONOMICS OF HEALTHCARE On successful completion of this Module the student should be able to: 1. Illustrate the life-cycle management (clinical, regulatory and marketing) of medicines. 2. Describe the processes of production and review of product information to ensure adherence to ethical and legal principles pertaining to marketing activities (Good Promotional Practice). 3. Discuss the role of patient organisations. 4. Discuss the principles & practical application of health economics and patient-reported outcomes within the pharmaceutical industry. 5. Outline the principles of health technology assessment (HTA) and its role in the supply of medicines to the marketplace. 6. Discuss the principles and practice of marketing within the pharmaceutical industry. 7. Discuss drug budget control; pricing mechanisms. Competencies (Cognitive Level) Area 3: HEALTHCARE AND PROFESSIONALISM Domain VII: COMMUNICATION AND MANAGEMENT Describe the principles & practices of people management & leadership to apply them within their own working environment; set learning & improvement goals. Ensure that the knowledge, skills & behaviours associated with the competent practice of pharmaceutical medicine are communicated effectively, using the best techniques & practices whilst participating in the education of colleagues & stakeholders. Organise networks and builds & maintains relationships, encouraging contribution to & working with inter-professional teams to meet the business objectives. Support the success of the organisation by actively contributing to develop strategic plans to achieve goals, manage resources & people, and leverage performance. Ensure organisational excellence by developing critical evaluation skills, encouraging improvement & innovation in managing change. Identify strengths, deficiencies & limits in one’s knowledge & expertise. Work effectively as a member or leader of a healthcare team or other professional group. Explain his/her accountability to key stakeholders, society & the profession of pharmaceutical medicine. Apply quality & performance improvement concepts to address organisational performance issues. A model of competency (Miller 1990) DOES Performance SHOWS HOW KNOWS HOW KNOWS Simulation Applied knowledge Knowledge DOES SHOWS HOW KNOWS HOW KNOWS Assessing the practical modules COMPETENCY Does the trainee have the knowledge, skills and behaviours to be able to do the task or project in question to the required standard? Level One - Fully competent Level Two - Understands the underlying principles DOES SHOWS HOW KNOWS HOW KNOWS Assessing competency Outcome Real world assessment of activity Did it achieve its aim? Outputs Review results of activity (documents, targets achieved) Has trainee demonstrated competence? Observation Review activity being done Is the trainee demonstrating competence? Example Competency (Area 1; Domain 1: Discovery of Medicines & Early Development). (Able to) evaluate the clinical and non-clinical pharmacology and toxicology evidence for a new candidate for clinical development. Learning Outcomes (PharmaTrain Base Course): M2.1 Choice & Predictive value of the non-clinical programme as a part of the overall drug development plan. M2.2 Integration of non-clinical tests into the overall drug development plan (including scheduling of toxicology tests with respect to clinical trials. M2.3 Steps in the pharmaceutical development of a drug substance and the final drug product (including chemical and biological compounds). M2.5 Overview of non-clinical study requirements prior to FIM studies. Syllabus topics: (1.7, 3.2, 3.3, 3.4, 3.5, 3.6, 3.9) In Vitro & in vivo testing of new compounds (1.7). Differences in non-clinical safety & toxicity packages between small molecules and biologicals (3.2). The fundamental differences and similarities between the pharmacology and toxicology of compounds and their metabolites in animals and man, and their qualitative and quantitative assessment (3.3). The purpose of descriptive and quantitative in vitro and in vivo testing (3.4). The choice of and the predictive value of these tests for acute, chronic, reproductive, genetic and immune toxicology and carcinogenicity (3.5). Common mechanisms of damage to organs and their detection or elucidation (3.6). The regular review of toxicology, its inclusion into clinical trial protocols and investigator brochures, and the appropriate planning and correlation with the clinical evaluation of potential and observed toxicity in patients (3.9). Competency (Area 1; Domain 1): (Able to) evaluate the clinical and non-clinical pharmacology and toxicology evidence for a new candidate for clinical development. Knowledge: Syllabus topics: 1.7, 3.2, 3.3, 3.4, 3.5, 3.6, 3.9 (as described). Applied Knowledge: Demonstrate knowledge of: Relevant and current regulations. How, in particular, the pharmacology and toxicology data necessary for Phase 1 studies must be designed, reviewed and approved in readiness for clinical trials. Components of the Clinical Development Plan required in Europe. Components of a regulatory licensing (marketing) submission required in Europe. Awareness of, and how to obtain advice on, US and Japanese regulatory needs. Competency (Area 1; Domain 1): (Able to) evaluate the clinical and non-clinical pharmacology and toxicology evidence for a new candidate for clinical development. Skills: Demonstrate ability to: Define or review the planned clinical pharmacology of the candidate investigational product before clinical trials are begun. Anticipate possible disease-related variations in drug handling in patients compared with normal healthy subjects. React to unexpected findings promptly and , if necessary, suspend further work while other expert opinions are obtained and the issue is clarified. Describe past problems in this clinical or therapeutic area that have led to regulatory refusal of trials or their modification. Competency (Area 1; Domain 1): (Able to) evaluate the clinical and non-clinical pharmacology and toxicology evidence for a new candidate for clinical development. Behaviours / Attitudes: The Pharmaceutical Physician / Medicines Development Professional: Accepts a pivotal role in preparation of a development plan that requires knowledge & judgement. Recognises the value of liaison with other experts in related fields in the design and interpretation of studies. Exhibits strict compliance with regulations and guidelines. Understands the need to keep senior management informed. BASE COURSE LEARNING OUTCOMES SYLLABUS TOPICS (KNOWLEDGE) LO1 LO2 APPLIED KNOWLEDGE SKILLS ATTITUDES PP/MDS COMPETENCY From Learning Outcomes to Competencies LOx Specialist vocational path Diploma-level programme (30 ECTS) Knowledge, Applied Knowledge Assessment, Examination Workplace-centred, competency-based experience (CBE) Modular (specialty + general IPM module) Educational Supervision Framework of assessment, appraisal, review Certification, accreditation QMS Combination Academic / Vocational paths........ Combination academic/vocational paths (1+2, or 1+3, or 1+2+3) 1. PharmaTrain Base Course (6 Modules) Assessments Integrated examination Diploma (30 ECTS) 2. Extension Modules (4), Elective Modules (2) Assessments Dissertation / Thesis MSc (30+ ECTS) 3. Workplace-centred, Competency-based E&T (CBE) ES, assessment, appraisal, review Specialty Certificate; specialist title & accreditation (30+ ECTS) PharmaTrain: Workplace-centred, Competency-based Education & Training Platform for Pharmaceutical Physicians and Medicines Development Professionals Competency-based Programme ~55 Learning Outcomes = Base Course Curriculum ~60 Competencies = Curriculum How Delivered? All core competencies (~60) Core-core competencies (~30) Competencies of training experience (~20) Job-defined Modules (min. 2/6) (~20 CC); supplementary courses (~40) Additional General core competencies: Interpersonal & Management Skills Requirements for Competency-based programme Professional / vocational track (not academic) Training Plan (job/project orientation) Educational Supervision ES training, approval, standards Assessment of competency Outcomes, Outputs, WPBAs (tools) Evidence of Competency (validated, authenticated, realistic) Portfolio, Training Record, e-Portfolio Requirements for Competency-based programme Appraisal (Educational & Annual Performance) Review of progress & achievement (e.g. Annual) Competency-based Courses Interactive, multi-modal, assessments (to Miller level of simulation), course QMS QMS of programme Outcome / qualification (e.g. European MS-CCT) Specialist in Pharmaceutical Medicine; Medicines Development Certification / Accreditation body Legal, recognised, sets standards for good practice