cardiovascular
advertisement

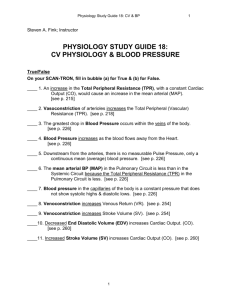
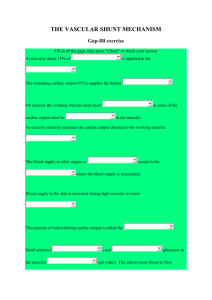
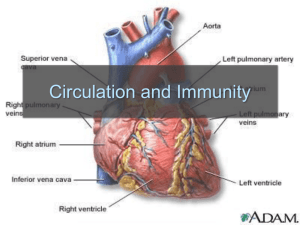
S1 Secretion Reabsorption Filtration S2 Circulatory System Circulates • • • • • Nutrients: glucose, amino acids, fatty acids, ketones, etc Wastes: Hormones: bound & free Gases: CO2 and O2 Formed Elements: Cells and Cell Fragments – Erythrocytes, Leukocytes, Thrombocytes = Platelets Other roles of the Cardiovascular System Thermoregulation Blood Clotting Reproduction (ex: penile erection) S3 Blood volume ~ 5 liters Figure 12.01 Serum = plasma – clotting factors Entering and Exiting the blood Components…… EPO and “The Scoop on Tissie” Discontinuous capillaries in bone marrow, spleen, & liver permit erythrocytes to enter and exit blood. Formed elements Hct = percentage of blood volume occupied by RBCs Anemia Blood doping & erythropoietin (hormone that stimulates erythrocyte production in bone marrow) to increase hematocrit S4 Fig. 12.02 Arteries..away from heart Veins..return to heart Resting Cardiac Output = 5L/min for each side! When left heart can’t pump all the blood it receives from pulmonary circuit (due to high aortic pressure and/or damage to left ventricle) blood accumulates in pulmonary circuit. This is congestive heart failure. Symptom: shortness of breath. Regional blood flow determined by arteries and arterioles. S5 Figure 12.04 CO = 5L/min for each circuit Up to 35 L/min in strenuous exercise S6 Pulmonary circuit CO = 5 liters/min Arterial Blood Pressure Systemic Circuit Exchange Vessels What’s missing? CO = 5 liters/min Recall Portal Systems! Resistance Vessels Microcirculation Capacitance vessels S7 Pulmonary circuit Pressure gradients makes fluids move. Moving fluids flow, but flow is limited by resistance. Resistance creates pressure. Systemic Circuit Arterioles establish Mean Arterial Pressure S8 Radius of arterioles regulates Q to organs F=Q=ΔP/R Flow = Pressure gradient/Resistance from Ohm’s Law (V=IR) Double radius … 16x flow R= 8Lη/πr4 Half radius….1/16th flow Q= ΔP πr4 8Lη Poiseulle’s equation Smooth muscles determine radius S 14 Mean Arterial Pressure = Cardiac Output x Total Peripheral Resistance MAP = CO x TPR MAP = (HR x SV) x TPR S1 Cardiac Output = Heart Rate X Stroke Volume What regulates heart rate? What regulates Stroke Volume? CO = HR x SV 5L/min = 72 beat/min x 70 ml/beat The Cardiac Cycle animation Problems with valves: Heart murmurs ≠ heart sounds ….Stenosis (narrowing) →Heart Murmurs (turbulent flow past a constriction) Figure 12.07 note: origin of neonatal heat murmurs (foramen ovale) ….Prolapse (eversion) allows backflow (also generates murmurs) S4 Tricuspid Heart sounds produced by valve closings Semilunar Valves Bicuspid =Mitral Animation S3 Cardiac Myofiber action potential Plateau phase Figure 12.13 Long refractory period prevents summation in cardiac myofibers Cardiac Myofiber S4 Figure 12.11 S5 SA node cells do not have stable resting membrane potential, spontaneously produce AP, are Pacemaker cells S5 Cardiac Pacemaker action potential Figure 12.14 Ectopic Pacemaker Pacemaker Cells in Conducting System: SA Node and Bundle of His Locations other than SA Node These cells set the rhythm & control Heart Rate. 1QQ # 14: Answer one. 1. A) Which vessels are classified as exchange vessels? B) Why are they called exchange vessels? 2. A) What produces a heart sound? B) What produces a heart murmur? 3. With all other factors held constant, how would blood flow be affected by a doubling of the pressure gradient? 4. A) Explain how a heart can continue to beat even if the SA node is not functioning. B) Would this heart rate be faster or slower than the rate produced by the SA node? S 15 Figure 12.22 Intrinsic Rate = 100 beat/min 2 effects of Parasymp: hyperpolarization & slower depolarization S6 Figure 12.23 NE Beta-adrenergic receptors Effect of “Beta blockers” EPI ACh mAChR Effect of atropine S7 What prevents the AP from being conducted from ventricles back to atria? Fibrous connective tissue between atria and ventricles prevents the conduction of action potential. Only route is via AV node, bundle of His, bundle branches, Purkinje fibers, and to ventriclular myofibers. S8 “Sis-toe-lee” 1st Heart Sound = Closure of Atrioventricular (AV) valves at beginning of Ventricular Systole “die-ass-toe-lee” 2nd Heart Sound = Closure of Semilunar valves at beginning of Ventricular Diastole S9 Figure 12.20 Systolic Diastolic Atrial Fibrillation Stroke Volume Ejection Fraction = SV/EDV Ventricular Fibrillation & Defibrillation Animation S 10 Events are same for Cardiac Cycle for Right Side of Heart; only difference is lower systolic pressures in right atrium and right ventricle. S1 So far, we’ve dealt with the factors that control Cardiac Output by changing heart rate. 3 CO = HR x SV 2 + sympathetic - parasympathetic 1 5L/min = 72 beat/min x 70 ml/beat 35L/min = ? beat/min x ? ml/beat S2 Figure 12.20 Stroke Volume Animation S3 Frank-Starling Law of the Heart Does not depend on hormones or nerves Assures that the heart adjusts its output based on VENOUS RETURN Ventricular Function Curve Ways to enhance Venous Return: 1) muscle contractions 2) “respiratory pump” 3) venoconstriction FS LoH = SV is proportional to EDV ↑VR→ ↑EDV → ↑SV S4 Length-tension “curve” for Cardiac muscle Fig. 09.21 High EDV Low EDV Overinflation of ventricles leads to less effective pumping S5 Overinflation of ventricles results in reduction in stroke volume Treatments? …..diuretics S6 NE from Symp postganglionics & EPI from Adrenal medulla Contractility Increase Ejection Fraction Note: cardiac myofibers NOT innervated by parasympathetic division S7 3 Effects of Sympathetic Stimulation 1: Increase rate of contraction 2: Increase peak tension 3: Decrease twitch duration Why should the contraction be shorter? Afterload is analogous to trying to pump more air into a tire that is already fully inflated (heart contracting to overcome diastolic pressure.) S9 High blood pressure increases the workload of the heart….. Cardiac hypertrophy….increase chance of irregular conduction of AP through heart Hypertrophic cardiomyopathy S8 Summary: Control of Stroke Volume FS LoH • End diastolic volume (preload) • Contractility (strength of ventricular contraction due to adrenergic stimulation) • Pressure in arteries that must be overcome = Afterload S 11 Factors that control Cardiac Output by changing heart rate and stroke volume. Afterload (MAP) CO = HR x SV EDV (FSLoH) + sympathetic - parasympathetic contractility 5L/min = 72 beat/min x 70 ml/beat 35L/min = ? beat/min x ? ml/beat Summary of Factors that Regulate Cardiac Output S 12 Fig. 12.28 Even persons with heart transplants can adjust CO in the absence of innervation of heart. S 13 Heart is pump that generates pressure gradient. Blood flows through vessels, which have resistance. Arterioles have greatest resistance and create “backpressure” in the arteries and aorta. Mean Arterial Pressure = diastolic +1/3(systolic – diastolic) = 70 + 1/3(120-70) = 70 + 17 = 87 mm Hg S 11 Factors that control Cardiac Output by changing heart rate and stroke volume. Afterload (MAP) CO = HR x SV EDV (FSLoH) + sympathetic - parasympathetic contractility 5L/min = 72 beat/min x 70 ml/beat 35L/min = ? beat/min x ? ml/beat S1 Properties of Blood Vessels All vessels and heart chambers lined with ENDOTHELIAL cells (simple squamous) • Arteries • Arterioles Variable Resistance vessels • Capillaries Exchange • Venules Capacitance vessels, high • Veins compliance, low pressure, Elastic, low compliance, large diameter, low resistance vessels Wall = simple squamous endothelium No smooth muscle; cannot change diameter valves for unidirectional flow S2 Aorta Brachial or Femoral artery Fig. 12.29 Damage to artery vs vein Pusatile flow S3 Fig. 12.39b Analogy: river width and flow S4 Fig. 12.30 Stretching elastic connective tissue Elastic recoil of stretched arterial walls during ventricular systole maintains arterial pressure during diastole as blood drains into arterioles. Atherosclerosis Recoil of elastic connective tissue Point of Confusion: Smooth muscles in arterial walls DO NOT rhythmically contract, do not pump! S5 Arteries and Arterial Pressure Mean Arterial Pressure Arterioles have two main functions: 1) regulate flow to tissues and organs and 2) responsible for Total Peripheral Resistance which influences Blood Pressure. MAP = CO x TPR Poiseulle’s Equation Arteriole S6 Fig. 12.50 Heart Arteries Mean Arterial Pressure Totol Peripheral Resistance CNS Skin Sk. Muscle Gut Arterioles Kidneys Cardiac Output S7 Receptors for other ligands Alpha receptors more common except in skeletal muscle arterioles which have more B2 receptors S8 Fig. 12.36 Metabolic vasodilators No parasympathetic innervation of arterioles! Importance of sympathetic “tone.” Metabolic autoregulation, flow autoregulation, myogenic autoregulation S4 Figure 12.02 Arteries = 10% of Blood Volume Veins = 60% of Blood Volume Arterioles = Resistance vessels Capillaries = 5% of Blood Volume S5 Capillaries: Continuous, discontinuous, and fenestrated capillaries: Ex: brain liver endocrine glands Figure 12.38 Generate vasodilators and vasoconstrictors Arterioles: 1) Extrinsic control by hormones and nerves 2) Intrinsic (local) control by …..a) metabolic autoregulation, …..b) flow autoregulation, and …..c) myogenic autoregulation. 1QQ # 15 Answer one. 1. Describe metabolic autoregulation and list four substances that are classified as metabolic vasodilators. 2. What is the main difference between flow autoregulation and metabolic autoregulation? 3. Explain why the pressure in a major artery doesn’t fall to 0 during ventricular diastole. S6 Capillary exchange by: Diffusion, vesicle transport, bulk flow, mediated transport S7 Fig. 12.40 Diffusion is the most important mode of exchange of nutrients S8 Figure 12.41 Colloids Crystalloids = colloids (impermeable proteins) Bulk Flow S9 Cell Membrane: selectively permeable Capillaries: highly permeable except to proteins S 10 Bulk Flow through aqueous channels and intracellular clefts Figure 12.42 Regulated by arterioles Starling Forces Net filtration = 4L/day Main difference in the Pulmonary circuit? S 11 Fig. 12.43 Pc Pc Pc S 12 Who Cares? Aunt Esther Cancer of the liver; Failure of hepatocytes to produce plasma colloids S 13 Figure 12.41 Colloids Crystalloids Bulk Flow S1 Figure 12.47 Fate of 4 L/d excess filtrate Mode of propulsion? Liver & Bone Marrow & Spleen S2 Veins are Capacitance vessels (high compliance) with valves for unidirectional flow Figure 12.44 Arteries are low compliance, so any increase in volume increases pressure. S3 MAP = CO x TPR Fig. 12.53 Negative feedback control: stimulus, receptors, afferent pathway(s), integrator, efferent pathway(s), effector(s) response(s) + other baroreceptors S4 Fig. 12.54 What happens to the set point for MAP during exercise? S2 Mean Arterial Pressure = Cardiac Output x Total Peripheral Resistance MAP = CO x TPR MAP = (HR x SV) x TPR S6 Test 3 Hemorrhage Diagram On one page, create a well-organized diagram for the following. Beginning with a loss of about 1 liter of blood from a vein, diagram the early events associated with hemorrhage and the negative feedback responses to hemorrhage in a well-organized diagram. Write legibly! Completeness, accuracy, and detail, together with the proper sequence earn maximal points. The following abbreviations can be used: ACE, AI, AII, Aldo (aldosterone), JGA, mAChR, Hct, Q, SV, EF (ejection fraction), RBC, HR, EDV, ACh, ANH, ADH, CO, TPR, EPO, VR, MAP, EPI, NE, SAN (SA Node), aAdR , bAdR, Symp (sympathetic), Parasymp (parasympathetic), PV (plasma volume), r (radius), Pc, fAP (frequency of action potentials.) Any other abbreviations must be defined. "If in doubt, write it out!" Use single headed arrows (→) to indicate sequential relationships and doubled-stemmed arrows to indicate increases or decreases.