Transplant - Atypical Hemolytic Uremic Syndrome
advertisement

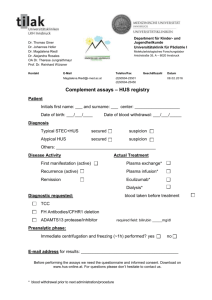
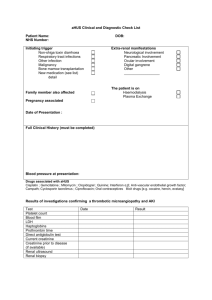
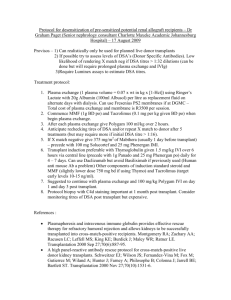
ESRD Management of Atypical Hemolytic-Uremic Syndrome (HUS) Jeffrey M. Saland, M.D. Department of Pediatrics Mount Sinai School of Medicine Conflicts / Disclosures Will discuss off label uses No financial interests in any agents discussed No financial interest in any healthcare-related entity Overview • A significant percentage of cases of atypical HUS are due to disorders of complement regulation. Overview • A significant percentage of cases of atypical HUS are due to disorders of complement regulation. • Empiric plasma therapy can delay or prevent ESRD in many of those cases Overview • A significant percentage of cases of atypical HUS are due to disorders of complement regulation. • Empiric plasma therapy can delay or prevent ESRD in many of those cases • Risk of post-transplant recurrence depends on the specific disorder of complement regulation. Overview • A significant percentage of cases of atypical HUS are due to disorders of complement regulation. • Empiric plasma therapy can delay or prevent ESRD in many of those cases • Risk of post-transplant recurrence depends on the specific disorder of complement regulation. • Emerging therapy may expand ESRD options Typical HUS Triad of : Microangiopathic hemolytic anemia Thrombocytopenia Acute renal failure Generally diarrhea-associated Shiga toxin produced by E coli serotype O157:H7 Shigella, Salmonella, others also Food borne disease: uncooked / unpasteurized products contaminated by animal wastes Or other infections (respiratory): Invasive S. Pneumoniae or viral infections Typical HUS A severe condition: acutely 2.5% mortality, often significant morbidity Long term results (10-20 years after HUS*) 63% Complete recovery 12% Recovery with proteinuria 6% Recovery with proteinuria and HTN 16% Recovery with low GFR ± proteinuria or HTN 3% ESRD * Diarrheal or URI- related only, pediatric Spizzirri et al. Pediatric Nephrology 1996 Atypical HUS Clinically very severe 15% died 25% ESRD 15% renal insufficiency 60% major sequelae 1/3 recover without significant renal disease most (75%) of these had a single episode few (25%) of these had recurrent aHUS (a pediatric series) Taylor et al Ped Neph 2004 A Classification of TMA (Thrombotic Microangiopathy) Typical / diarrheal (HUS or TTP) Complement defects Atypical HUS von Willebrand proteinase (ADAMSTS13) defeciency Generally TTP Cobalamin-C deficiency TMA + multiorgan failure Quinine-related Abrupt TMA, exposure related Post transplantation De-novo renal TMA (calcineurin inhibitior related) May be renal “isolated” Others: HIV, radiation, chemotherapy HELLP, antiphospholipid Ab syndrome, unclassified Besbas et al. Kidney International 2006 Complement and Atypical HUS Since the early 1970’s alternative pathway complement activation (low C3), has been recognized in some cases of atypical HUS 1981: 1st case of HUS with factor H deficiency described 1998: Linkage analysis in 3 families with HUS provided clear association with CFH Clin. Exp. Immunol. (1981), Kidney International (1998) Complement and Atypical HUS About 50%-60% of aHUS cases are associated with a mutation in a complement-related gene Protein Gene Source Location % of aHUS Factor H CFH Liver circulates ~ 15-30% Factor I CFI Liver circulates ~ 5-10% Membrane Cofactor Protein MCP Widespread Membrane bound ~ 10-15% Factor B CFB Liver, ? circulates <5% C3 Liver, ? circulates ~ 5-10% CFHR1/ CFHR3 Lymphocyte circulates ~ 10% C3 Anti-FH-Ab Unknown ~ 40-50% Jozsi et al. Blood 2008, Frémeaux-Bacchi V et al. Blood 2008, Goicoechea de Jorge 2007, Caprioli, et al Blood 2006, Kavanagh Curr Opin Nephrol Hypertens, 2007 C3 Levels By Mutation Sellier-Leclerc, A.-L. et al. J Am Soc Nephrol 2007;18:2392-2400 Recommended Initial Evaluation of HUS Because infections trigger both typical and atypical HUS, initial evaluation should encompass both Testing should include C3 level as well as classic evaluation (stool culture, LDH, smear, etc.) ADAMSTS13 / auto-Ab analysis if TTP not ruled out Save some plasma for later analysis Plasma Therapy Fluid phase complement proteins reside in plasma and are therefore subject to plasma therapy Caprioli, et al. Blood. 2006 Plasma Therapy Fluid phase complement proteins reside in plasma and are therefore subject to plasma therapy Plasma Infusion: • Repletes but does not remove mutant protein Plasma Exchange: • Removes mutant protein and repletes Caprioli, et al. Blood. 2006 Plasma Therapy Fluid phase complement proteins reside in plasma and are therefore subject to plasma therapy Plasma Infusion: • Repletes but does not remove mutant protein Plasma Exchange: • Removes mutant protein and repletes There are MANY anecdotes of prolonged preservation of kidney function in patients with CFH mutation, though most eventually suffer ESRD. Benefit is not clear for MCP mutations– most (single) episodes seem to recover with or without exchange Caprioli, et al. Blood. 2006 Detecting Complement-related HUS (Trying to Prevent ESRD) Criteria for empiric plasma therapy treatment of aHUS Presence of any of the following or Absence of the Following Patient age < 6 months Slow or insidius onset of HUS Multiple HUS Episodes or relapses Asynchronous family history of HUS Previous unexplained anemia HUS after any type of organ transplantation Prodromal diarhhea Invasive S. pneumoniae infection Saland, et al. JASN 2009, Ariceta et al. Ped Neph 2008 Diagnosis of HUS Atypical presentation Empiric Plasma Exchange Clinical Exceptions Plasma Exchange within 24 hrs 1.5 Volumes (60-75 ml/kg) per session FFP or Octaplas® Repeat Plasma Exhange Daily x 5 Then 5 sessions/week for 2 weeks Then 3 sessions/week for 2 weeks Assess Outcome at Day 33 Ariceta et al. Ped Neph 2009 Withdrawal Alternate Diagnosis Plasma Exchange Complication Early remission Summary #1 Key atypical features require empiric plasma exchange. Summary #1 Key atypical features require empiric plasma exchange. C3 levels should be part of every HUS evaluation Save blood from before plasma exchange Summary #1 Key atypical features require empiric plasma exchange. C3 levels should be part of every HUS evaluation Save blood from before plasma exchange Patients with aHUS should undergo genotyping for the most up-to-date list of complement-related disorders: Summary #1 Key atypical features require empiric plasma exchange. C3 levels should be part of every HUS evaluation Save blood from before plasma exchange Patients with aHUS should undergo genotyping for the most up-to-date list of complement-related disorders: CFH, CFI, MCP, C3, CFB, anti-FH-Ab – CFHR1/CFHR3 (more likely to be added) Summary #1 Key atypical features require empiric plasma exchange. C3 levels should be part of every HUS evaluation Save blood from before plasma exchange Patients with aHUS should undergo genotyping for the most up-to-date list of complement-related disorders: CFH, CFI, MCP, C3, CFB, anti-FH-Ab – CFHR1/CFHR3 (more likely to be added) Contacting one of the major registries is prudent ESRD Management of aHUS ESRD Management Do not diagnose ESRD too soon. Renal recovery may occur if TMA is halted. In dialysis dependent patients, native nephrectomy should be considered for: • Ongoing HUS (clinical or biochemical) • Severe hypertension ESRD Management: Dialysis aHUS is generally quiescent during ESRD Rare findings reported during dialysis: • Angioedema, complement activation (hemodialysis) • Hemolysis / thrombocytopenia • Subclinical hepatic (or other organ) involvement Jalanko, et al. AJT 2007, Saland, et al. CJASN 2009 Subclinical Hepatic Involvement Saland et al. CJASN 2009 ESRD Management: Dialysis Due to a high rate of transplant failures, aHUS patients have been faced with extremely long dialysis duration and its accompanying risks. Transplant Considerations Gray, Henry. Anatomy of the Human Body. Philadelphia: Lea & Febiger, 1918; Bartleby.com, 2000. www.bartleby.com/107/. Complement and Atypical HUS Risk of recurrence after “unmodified” kidney transplant Protein Gene Source Location Recurrence Rate Factor H CFH Liver circulates > 80% Factor I CFI Liver circulates > ~ 80% MCP MCP Widespread Membrane bound ~ 20% Factor B CFB Liver, ? circulates ? C3 Liver, ? circulates ? CFHR1/ CFHR3 Lymphocyte circulates ? C3 Anti-FHAb No known mutation Loirat, C et al. Pediatric Transplantation 2008, Saland et al. JASN 2009 30% Post-Transplant HUS Recurrence Most are within 1 month Plasma responsiveness of the underlying defect is often retained. If untreated, most result in graft loss Chronic plasmapheresis may be required Seitz, B et al. Transplantation Proceedings 2007, Options for Transplantation Kidney transplantation* Options for Transplantation Kidney transplantation* Combined liver-kidney transplantation* Complement and Atypical HUS Risk of recurrence after “unmodified” kidney transplant Protein Gene Source Location Recurrence Rate Factor H CFH Liver circulates > 80% Factor I CFI Liver circulates > ~ 80% MCP MCP Widespread Membrane bound ~ 20% Factor B CFB Liver, ? circulates ? C3 Liver, ? circulates ? CFHR1/ CFHR3 Lymphocyte circulates ? C3 Anti-FHAb No known mutation Loirat, C et al. Pediatric Transplantation 2008, Saland et al. JASN 2009 30% Combined Liver Kidney Transplant For aHUS Secondary to CFH Mutation First 3 Experiences not Encouraging Auxiliary liver, several month function followed by acute decompensation, death Hepatic graft failure* with neurological deficits, 2nd liver transplant at 1 month Primary hepatic non-function*, death * Complement mediated injury to liver vasculature Cheong HI. (Abstract) ASN/ISN World Congress 2001, Remuzzi G, et al. Lancet 2002, Remuzzi G, et al. AJT 2005, Cheong HI et al. Pediatr Nephrol 2004 Surgery is a trigger for complement activation Preparative plasma exchange before transplant followed by serial plasma exchange is recommended Liver-Kidney Transplant Protocol Modified by Plasma Exchange • • • • • • • Hemodialysis (if needed) session no heparin Plasma exchange with FFP (minimum 1.5 volumes) < 6 hours of surgery 10- 20 ml/kg FFP intraoperatively Additional FFP if clinically indicated Post-operative LMW heparin prophylaxis Low dose aspirin prophylaxis Plasma exchange removes mutant FH, replaces normal LMW heparin used empirically Hold anticoagulation for bleeding or coagulopathy Saland, J et al. JASN 2009 Combined Liver Kidney Transplant For aHUS Secondary to CFH Mutation A Modified* Approach is Potentially Successful, Though Risky. 1. 2. 3. 4. 5. 6. 7. 8. 9. NYC #1: whole liver Helsinki #1: whole liver Helsinki #2: whole liver NYC #2: split liver Helsinki #3: adult, whole liver UK #1: whole liver* Boston #1: whole liver NYC #3: split liver, death (hepatic artery thrombosis) NYC #4: split liver, death (SVC syndrome complication)) * Native kidney function preserved, liver tx only Saland et al, AJT 2006, Jalanko et al. AJT 2008, Saland et al. CJASN 2009 and verbal communications: Jalanko 2007, Milford 2008, Milner 2008 Options for Transplantation Kidney transplantation* Combined liver-kidney transplantation* Kidney transplantation* followed by chronic plasma exchange prophylaxis Not yet … followed by chronic anti-complement therapy followed by specific factor replacement (eg. FH) Transplant Decisions MCP Mutation Transplantation Reasonable Current consensus for now is to provide pre-operative plasma exchange and at least one month of tapering plasma exchange protocol LMW heparin anticoagulation Loirat, C et al. Pediatric Transplantation 2008, Saland,et al. JASN 2009 Transplant Decisions MCP Combined with other Mutations No consensus, isolated kidney may be reasonable If transplanted, provide preoperative plasma exchange and at least one month of tapering plasma exchange protocol LMW heparin anticoagulation Loirat, C et al. Pediatric Transplantation 2008, Saland,et al. JASN 2009 Transplant Decisions CFH or CFI Mutation* Wait for new Rx • FH concentrate • Complement inhibitors Combined Liver-Kidney Tx Pre-operative Plasma exchange LMW heparin anticoagulation Renal Tx * Plasma exchange before and chronically after LMW heparin anticoagulation * Especially if kidney transplant in family members with same mutation was successful Loirat, C et al. Pediatric Transplantation 2008, Saland,et al. JASN 2009 Transplant: Anti-FH-Autoantibodies One Successful Case Reported Pretransplant preparation using: plasma exchanges over several weeks (the response was not complete) 4 weekly doses of rituximab added Anti-FH Autoantibodies Anti-FH-Ab levels were monitored Fairly routine transplant protocol: Basiliximab, prednisone, cyclosporine Resulted in sustained antibody supression for over 4 months Kwon et al, NDT 2008 Transplant Decisions CFB, C3 Mutations Case by Case: Unclear impact of: Non-hepatic protein sources Complement activating potential of residual protein Therapeutic potential of future anti-complement Rx Saland et al. JASN 2009 Transplant Decisions No Known Mutation Transplantation Reasonable Current consensus for now is to provide pre-operative plasma exchange and at least one month of tapering plasma exchange protocol LMW heparin anticoagulation Loirat, C et al. Pediatric Transplantation 2008 Saland, J et al. JASN 2009 Final Summary Atypical HUS has a high risk of ESRD Transplantation options depend on the specific cause Transplant surgery triggers complement activation For high-recurrence risk conditions: Current options are risky and limited Emerging treatments are promising Acknowledgments Foundation for Children with Atypical HUS Censensus Group, Liver-Kidney Transplantation for HUS Bergamo: Drs. Giussepe Remuzzi & Piero Ruggenenti Newcastle: Dr. Timothy Goodship U. Iowa: Dr. Richard Smith