Cultural and Social Issues in Injury Prevention
advertisement

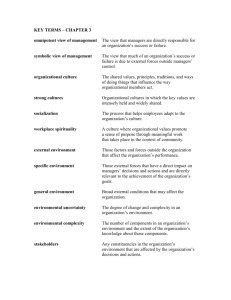
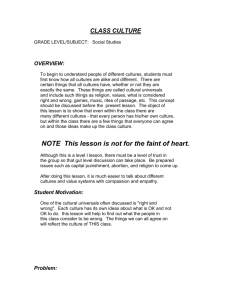
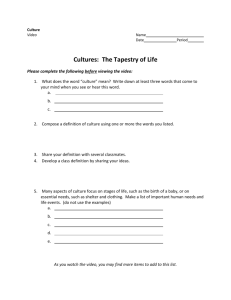
Maria Veronica Svetaz, MD MPH 5th Annual MN Childhood Injury Summit Workshop Objectives For our diverse communities, basic needs for food, shelter, protection from violence and prevention of self-harm may be paramount. How do we address unintentional injury effectively in this context? Dr. Svetaz will explore 1) How to build an agenda that includes prevention of unintentional injuries. The role of fatalism within certain communities as a barrier to injury prevention and how to help individuals reclaim power. 2) How to craft meaningful messages for teenagers and for diverse communities in general. First Stop: Who is most at risk? For children, teens and young adults, unintentional injuries are the leading cause of death. Children aged 1–4 have the highest rate of emergency department treatment for unintentional injury, followed by 15–19 year-olds, 10–14 year-olds and people in their early 20s. Preventing Unintentional Injury in Minnesota: A Working Plan for 2020 Second Stop: Trends and Challenges Increasing cultural diversity. Perceptions and definitions of safety may vary by culture. Minnesota’s diverse population requires cross-cultural sensitivity, competence and effective partnerships, and engagement on the terms of other cultures. Just providing information doesn’t work; traditional methods of reaching those at risk are not effective across all ages or cultures. The challenge is not only outreach, but also inclusion. Preventing Unintentional Injury in Minnesota: A Working Plan for 2020 SAFETY Safety is the state of being "safe" (from French sauf), the condition of being protected against physical, social, spiritual, financial, political, emotional, occupational, psychological, educational or other types or consequences of failure, damage, error, accidents, harm or any other event which could be considered non-desirable. Safety can also be defined as the control of recognized hazards to achieve an acceptable level of risk. Health Equity and your world Social Determinants and Your Community Social Determinants and Race Health Disparities: A type of difference in health that is closely linked with social or economic disadvantage. Health disparities negatively affect groups of people who have systematically experienced greater social or economic obstacles to health. These obstacles stem from characteristics historically linked to discrimination or exclusion such as race or ethnicity, religion, socioeconomic status, gender, mental health, sexual orientation, or geographic location. Other characteristics include cognitive, sensory, or physical disability [4]. Social determinants of Health- CDC Social Determinants and You Culture Identity and your view of the world Your LENSES, the way you learned to see the world, what is acceptable or unacceptable, what is expected or not All those unwritten rules that form cultural values and cultural norms. From Western Cultures From Eastern Cultures created byYang Liu, who was born in China and educated in Germany From Western Cultures From Eastern Cultures 1. created byYang Liu, who was born in China and educated in Germany From Western Cultures From Eastern Cultures 1. created byYang Liu, who was born in China and educated in Germany From Western Cultures From Eastern Cultures created byYang Liu, who was born in China and educated in Germany The “KOA” ephyfany: Your reality may not be my reality! PART OF BEING INCLUSIVE IS ASKING THESE QUESTIONS: What you are seeing/living/needing is NOT the same as what I am seeing/living/needing due to social differences and completely different realities How you are seeing/living/needing is NOT PERCEIVED in the same way I am perceiving them due to different cultural identity formation. Discourses and Messages: And how to impact Motivation cross culturally How to start seeing that unknown/foreign reality that certain families are going through? Awareness of different agendas and unmet needs II. Creation of Empathy III. Realization that safety means a very different thing in a wealthy community than in a community enduring poverty IV. Creating real patient-provider partnerships I. Discourses and Messages: And how to impact Motivation cross culturally How to start realizing that my world view might be different than others? I. II. III. IV. Asking Exploring (listening) Open/ended questions Non judgmental questions/answers Where Fatalism sits in all of this? Freeman's poverty-cancer spiral concept offers insights into why traditionally underserved populations articulate and employ fatalistic perspectives (Freeman 1989). Freeman notes that poverty and its associated ills— undereducation, lack of employment, poor housing, lack of health care access, poor health outcomes—create a downward spiral, a self-fulfilling prophecy, and, ultimately, adverse health outcomes. Freeman describes the process by which poverty intersects with medical care and creates fatalism. First, unless there are discernible symptoms, poverty oftentimes forces people to focus on a day-to-day existence that stands in sharp contrast to a health prevention mode. By the time cancer symptoms are present, the disease has progressed beyond the localized stage, which necessarily limits treatment options and leads to poorer outcomes. Poor outcomes decrease the likelihood of survival and increase suffering, ultimately reinforcing fatalistic perspectives, as families and community members witness this cycle of late stage cancer diagnosis, more complicated, disfiguring, and painful treatments, poor outcomes, and, ultimately, death (Shankar et al. 2002). Deconstructing Fatalism: Ethnographic Perspectives on Women's Decision Making about Cancer Prevention and Treatment Elaine M. DrewDepartment of Family and Community Medicine Medical College of Wisconsin Fatalism and Patient Activation “In Western mainstream culture, where the expectation is to be autonomous, independent, self-directed and a manager over ones future, expressions of fatalism strike many as benighted, irrational, and counterproductive.Yet as our case studies reveal, “fatalism is an entirely rational way of coping with a world in which one feels powerless and has potential benefits, such as enhanced enjoyment of the present that Western, achievement oriented cultures tend to discount” Deconstructing Fatalism: Ethnographic Perspectives on Women's Decision Making about Cancer Prevention and Treatment “Indeed, we argue that fatalism in the context of our two case studies represents a form of what medical anthropologist Mark Nichter refers to as “cultural idioms of distress,” which “are socially and culturally resonant means of experiencing and expressing distress in local worlds … evocative and index past traumatic memories as well as present stressors, such as anger, powerlessness, social marginalization and insecurity, and possible future sources of anxiety, loss and angst.” (2010:405) Deconstructing Fatalism: Ethnographic Perspectives on Women's Decision Making about Cancer Prevention and Treatment “Our work and others indicates that people actually do express fatalistic ideas. What we propose is that there is good reason why they express these ideas, and that such a reason tends to be located within resource-constrained conditions, such as those found in the Appalachian context. Furthermore, our narratives suggest that such rhetoric is not the primary determinant of health behavior but rather a culturally acceptable idiom of distress. Seeking a middle ground, we reject attempts to either toss out this frequently used idiom or to use the construct as an explanatory factor in supposed irrational health decisions. Instead, we advocate for a great appreciation of the complexities and nuances of fatalism” Deconstructing Fatalism: Ethnographic Perspectives on Women's Decision Making about Cancer Prevention and Treatment INCLUSIVITY: The PRACTICE A word on Patient Activation Most of our Models in HCH measure patient centeredness and part of that is Patient Activation But most indicators that measure Health Patient Activation, and the model seems VERY “mainstream”: see next picture int Slide for Teaching INCLUSIVITY: The PRACTICE A word on Patient Activation Racial/Ethnic Disparities And Consumer Activation In Health Health Affairs, 27, no. 5 (2008): 1442-1453 doi: 10.1377/hlthaff.27.5.1442 © 2008 by Project HOPE What preventions mean in light of current adversity? How to create powerful awareness of the need of prevention in the midst of current adversity? = Sharing the agenda: “What is the most oppressing/urgent thing that is in your mind today?” = framing prevention as a way of decreasing potential future stress and feeling pro-active = Meeting human beings where they are, and not judging. = Using their strengths and their resources as a starting point: “you are really family oriented, how can we make your home more safe for all your family to enjoy?” = When providers start seeing strengths, the families served by them will too, an unknown feeling for most, and they will start feeling power-full , and able to create stronger safer futures. TEENS!!! And young adults (think brain development :11-24) = Present oriented = Powerful? INVINSIBLE!!! =Concrete thinkers, the younger. Under development abstract thinking for most of them, but do not generalize!! =They need to belong! So be aware of peer pressure =They are wired to take risks, help them to be savvier on that (risk reduction) TEENS: The How To = Listen, don’t judge! Poker Face! = Add fun and humor to your recommendations: make it real for their world! Their world is today, and it has to be cool! = Discuss with them invincibility and how it feels, to start creating insight around that = Discuss with them how their behaviors will change with peers, and make them reflect about this (Have you noticed that you do different things when you are around friends? And make different decisions? With time, I had!), and work with them on how to resist pressure and how to say no. TEENS!!! Parents of teens were “left behind”, don’t have the tools they need to continue to parent in a developmentally appropriate way: SUPPORT PARENTS of TEENS!!! Work with parents to create Teen “Coaches” The coach concept for parents C reate confidence O bserve A dvise (reflect) C almly let them go to play, sorry, live! H elp them debrief the experience 28