Neuroanatomy Meds IV
advertisement

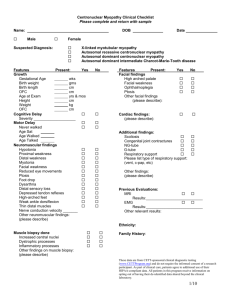
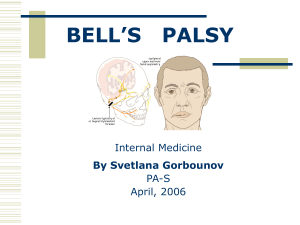
Neuroanatomy Meds IV Shannon L Venance, MD PhD Objectives: 1. 2. At the end of this session, provided with a history and exam, participants will be able: Localize the lesion to the appropriate part of the nervous system Compare and contrast vascular with demyelinating or neoplastic presentations of brainstem lesions. Case 1 A 47 year old man presents with a decreased level of consciousness (LOC). He complained of an sudden posterior occipital headache with R face tingling and drooping and then collapsed to knees(1130 hrs) while remaining alert. On route to hospital, seizure activity noted and he was intubated on arrival to the community ER and loaded with dilantin. He was transferred to Victoria Hospital as there were no ICU beds available locally. Case 1 continued….. PMHx: brief episodes of vertigo, dysarthria, collapsing (seconds to minutes only) for 8 months; otherwise healthy Med: ASA NKDA Soc Hx: married with 3 children Case 1 24 hrs after presentation hemodynamically stable intubated and fully ventilated, no sedating drugs unresponsive to voice no spontaneous eye opening pupils were pinpoint and reactive no horizontal eye movements with oculocephalic maneuver (OCM) absent corneal reflexes, no response to nasal tickle weak gag, constant hiccoughing ~ 1-2/min tone was reduced with brisk withdrawal to noxious stimuli in the legs bilaterally reflexes present, left > right; toes ↓↓ patient normal Case 1 48 hrs after presentation intubated, no breathing over the vent pupils were fixed and dilated no eye movements with OCM corneals and nasal tickle absent no gag, no hiccoughs flaccid tone no response to noxious stimuli all 4 extremities reflexes left > right; toes ↑↑ http://www.med-ed.virginia.edu/courses/rad/headct/index.html Case 2 32 yo male presents with a 6 month history of intermittent bifrontal headache with progressive symptoms 3 months of intermittent diplopia on looking right or left (no improvement with prism glasses) headache became constant, associated with mild nausea, worse in the mornings 2 months of right side weakness and incoordination (dropping glasses, r leg buckling, falling to the right) 1 month right facial numbness choking on liquids and had nasal regurgitation with coffee, tea symptoms worsened 1 week prior with a viral illness and fever Case 2 normal mental status pupils 8 mm OS and 6 mm OD, reactive, no APD restriction of right eye abduction with nystagmus vertical nystagmus on upgaze reduced pinprick right V1, V2, V3 right lower motor neuron type facial palsy palate deviated to the right, tongue midline flaccid, hypophonic dysarthria right arm/leg spasticity with ankle clonus R>L hyperreflexia with extensor plantar response bilaterally mild pyramidal weakness on the R dysmetria right > left “control” patient Case 3 Francois, a 48 yo right handed man woke this morning with weakness involving the entire left side of his face. Two days prior he noticed pain behind the left ear which continues. His breakfast tasted “strange” this morning. He has no other symptoms and he has otherwise been well. Your focused exam reveals normal tympanic membranes, full extraocular movements, a left lower motor neuron facial weakness (reduced forehead wrinkling, eye closure and grimace) with a midline tongue and palate. He hears sounds more loudly in his left ear. No pronator drift. Deep tendon reflexes are 2+ symmetrical with flexor plantar responses. Which of the following statements about facial weakness is true? A. B. C. D. E. Ramsay-Hunt syndrome is a cranial nerve VII palsy associated with lateral rectus paralysis. Prednisone is the treatment of choice for Bell’s palsy when started within 48 hours of onset. Lower motor neuron facial palsy involves paresis/paralysis of the lower facial quadrant only. There is no risk of recurrence with a Bell’s palsy. Cranial nerve nuclei located in the pons along with the facial nucleus include CN III, IV and VI Case 4 53 yo woman develops sudden onset of left sided weakness, right facial weakness and double vision 2 weeks after an MI treated with angioplasty PMHx also includes hypertension, stopped smoking 2 weeks ago (prev 25 ppy hx) her medications include ASA, ramipril, metoprolol and lipitor Case 4 abnormal eye movements on looking left – right eye does not adduct but convergence is spared (right eye adducts and pupil constricts) – left eye abducts with left-beating nystagmus vertical eye movements are normal weakness of the right face including the forehead weakness of the left arm and leg ~4/5 in a pyramidal distribution reflexes, L brisker than R with an upgoing L toe http://upload.wikimedia.org/wikipedia/en/thumb/b/b0/Internuclear_ophthalmoplegia.jpg/180px-Internuclear_ophthalmoplegia.jpg Some pathology 82 year old had been followed for many years, on levodopa/carbidopa for a degenerative process causing a rest tremor, slowness and stiffness of movement, soft voice with drooling and dysphagia; he had been falling more recently died of complications after sustaining a hip fracture from a fall control Parkinsonism Case 55 yo emaciated and dishevelled woman was found wandering on the streets and brought to the ER on Christmas Day she knew her name but was not oriented to date or time and could not give her age or address but provided a rich story which could not be corroborated language was normal but she was unable to recall 3 items after 2 minutes; 5 minutes later she denied having seen you before; otherwise reading, writing and higher mental functions were normal her neurologic exam was otherwise normal while waiting for the neurology resident, she was given a tray of holiday goodies which she devoured No known medical history, medications, allergies on examination 2 hours later, she was slightly drowsy but rousable, not oriented to month or year and thought the resident was her boyfriend she had nystagmus in all directions of gaze and her gaze was dysconjugate when looking right or left normal strength, reflexes 2+ except ankles 1+ and her toes were upgoing bilaterally mild reduction in vibration at the toes she was unable to heel-shin bilaterally and her gait is wide-based and markedly ataxic http://medlib.med.utah.edu/WebPath/CNSHTML/CNS083.html http://www.urmc.rochester.edu/neuroslides/slide157.html Summary: clinical brainstem CN III – XII symptoms and signs crossed sensory or motor findings coordination, ocular, vertigo acute onset – abrupt is vascular; if over hours – toxic, metabolic – if LOC, remember reticular activating system (RAS) within brainstem is responsible for alertness chronic – over weeks to months; neoplastic, demyelinating, degenerative http://www.meddean.luc.edu/lumen/MedEd/Images/NeuroLab/nl35sl.jpg http://www.meddean.luc.edu/lumen/MedEd/Images/NeuroLab/nl35sl.jpg http://www.meddean.luc.edu/lumen/MedEd/Images/NeuroLab/nl35sl.jpg http://www.meddean.luc.edu/lumen/MedEd/Images/NeuroLab/nl35sl.jpg Questions?