Social Factors
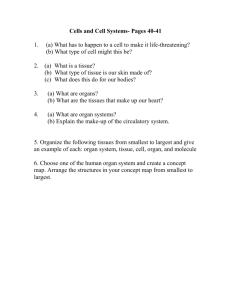
advertisement

The Biopsychsosocial Model Introduction to Primary Care: a course of the Center of Post Graduate Studies in FM PO Box 27121 – Riyadh 11417 Tel: 4912326 – Fax: 4970847 1 2 Aim-Objectives • Aim: At the end of this presentation, the participants will have knowledge of biopsychosocial medicine and believe on the importance of this model in PC. • Objectives: – – – – Can define systems approach Can define holistic health care model Can define biopsychosocial model Is aware of the importance of social, psychological and existential factors on health 3 A random case • A young women of 19 injured her knee while playing baseball and was admitted to hospital for surgery. When seen for follow-up by the surgeon, she showed weakness and muscle wasting in the leg and complained of a number of general symptoms (fatigue, sweating, pain in the neck). When the surgeon suggested that she was not doing her exercises, she became hostile and angry. Eventually she returned to her family physician, who found her with severe muscle wasting and still complaining of the same general symptoms. After excluding some physical causes of her symptoms, the doctor encouraged her to talk about the impact of the illness on her life. She had had a strongly religious upbringing, with emphasis on academic and athletic achievement. Having siblings with high academic abilities, she had based her self esteem on athletic achievements, which she now saw threatened by her injury. Given some insight into her problem and an opportunity to discuss it with the doctor, she began to cooperate with 4 her physiotherapist and returned to fully activity. Ages of medicine • • • • • • Symptomatic era Laboratory era Clinical era Social medicine Systems approach Biopsychosocial medicine 5 Symptomatic era • Hippocrates (460-377 BC) • Aristotle (384-322 BC) Warmth AIR FIRE Dry Humidity WATER SOIL Cold 6 Symptomatic era • Claudius Galenus (M 130-231) • Abubekir Razi (M 865-962) • Ibn-i Sina (M 980-1037) 7 Laboratory era • • • • • • • Andreas Vesalius (1514-1564) Anatomy Marcello Malpighi (1628-1698) Histology G.B.Morgagni (1628-1771): Patology Claude Bernard (1813-1878) Physiology Roudolph Virchow: (1821-1902) Cell path. Louis Pasteur (1825-1895): Bacteriology Emil Fischer (1852-1919) and Paul Ehrlich (1854-1915) Biochemistry 8 Clinical era • “It is more important to have information on the person who has the disease rather than the type of the disease.” Sir William Osler (1904) • Treat the patient, not the disease! 9 Social medicine • “Social medicine deals with investigating the relationships between medicine and the population and uses medical services for the wellness of the population without depending on any doctrine or ideology." Dr. Jules Rene Guerin, 1848 10 Systems approach • The human is in fact a very complex creature. • It is not always possible to find a single causative factor for human diseases. 11 Systems hierarchy (Engel 1980) Population Family, small groups, culture Individual Neuro-endocrine Immune system Organ systems Tissues Cells Melecules 12 Patients life before knee trauma Population Family, small groups, culture Individual Conservative Religious education with a brother of academic success Transition to adulthood, selfesteem due to success in athletism Neuro-endocrine Immune system Organ systems Tissues Cells Melecules 13 Effect of knee trauma Population Event Knee trauma Family, small groups, culture Doctor-Patient Individual Neuro-end. Immune sys. Organ systems Tissues Cells Melecules System changes Release of medical resources Crisis Disagreement, loss of communication Disrupture of life plan, immobility, pain, anger, depression, irritability Excess autonomic nervous system activity Tachycardia, sweating, weight loss Joint trauma, muscle injury Reaction to trauma 14 Effect of change Event Establishing therapeutic relationship System changes Population Release of rehabilitative resources Family, small groups, culture Resolving of crisis, understanding Doctor-Patient Establishing communication, therapy Individual Understanding the real reason of the problem, rearranging life objectives Neuro-end. Immune sys. Return of weight and heart rate, improvement of knee functions Organ systems Return of weight and heart rate, improvement of knee functions Tissues Cells Melecules Surgical intervention, release of muscle tension Improvement 15 Systematic Thinking • Systematic thinking is often used by scientists. • It makes it easy to understand • For example: – an occupational trauma may be due to inadequate tools (social), loss of attention (psychological) or drop of blood glucose (biological); – causing organ injury (biological), stress (psychological) or loss of income (economical). • However, isolating the problem is not applicable to general practice. A GP has to consider the complex relationship of problems 16 Biomedical model • Aim: to treat the knee problem and remove the physical pathology underlying the symptoms. • Which is important but not enough • What is needed?: understanding of the patients internal world 17 Is medicine really improving? • Number of laboratory tests increased 33% from 1967 to 1972 – McGinnis 1976 • What about patient satisfaction?? 18 The Holistic Health Care Model • Emphasizes personal development assuming – All types of health and disease are psychosomatic – There is a communication between body, mind and soul – Diseases arise from inability to adapt to different situations • Gives importance to personal care, education and prevention – – – – Natural nutrition, Herbal therapy, Acupuncture … 19 The Biopsychosocial Model (Engel 1977) • It encourages the clinician to observe the feelings, life objectives, attitude towards the disease, social environment, biochemical and morphologic changes. • The person is a complex of body, mind and social environment. Environmental and psychological conflicts are potential pathologies for the individual. • Feelings can affect physiological functions of the body (Zegans, 1983). • Instead of dealing primarily with biological factors, considering psychological and social factors as well will enable understanding disease processes. 20 Bio-Psycho-Social Factors Biologic Factors •Immune System •Endocrine System •Organ Systems •Tissues •… ORG ANI SM Social Factors •Community •Family •Culture •... Psychological Factors •Anxiety •Depression •... 21 Another case • • • • • • 35 y, male Married 3 kids Laborer in a factory Gets injured at work Unable to work for 3 months 22 Inadequate organized environment (social) Drop in blood glucose (biologic) Inattentive (psychological) Drop in income (social) Occupationa l injury Organ trauma (biologic) Stress (psychological) 23 LOSS of JOB (A social factor) DEPRESSION (Psychological) P. ULCER AGGREVATION (Biological factor) For an effective patient management, the interaction between all factors should be taken into acount 24 The LEARN Model - Listen with empathy the patients view to his/her problem - Explain the patient on his/her words the view and opinions of the doctor - Acknowledge the differences between the doctor and patients thoughts - Recommend a model integrating the patients as well as doctors opinions - Negotiate to a common solution with medical, ethic, legal acceptability covering the patients expectations 25 Berlin and Fowkes (1983) Summary • a) b) c) d) Which of the below is wrong regarding the psychosocial model? The person is evaluated with his family and environment There are multiple ethiologic dimenstions It evaluates the person with his body, soul and social environment It has a disease centered approach 26 • What is the main reason medicine moved from the laboratory era to the clinical era? • What is the main idea of the systems approach and how can GPs use it in patient care? • Can you explain the LEARN acronym developed by Berlin and Fowkes? 27