m5zn_9e38121393c021a
advertisement

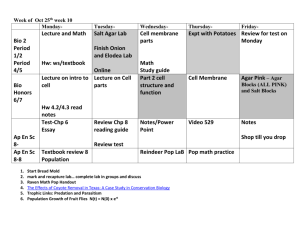
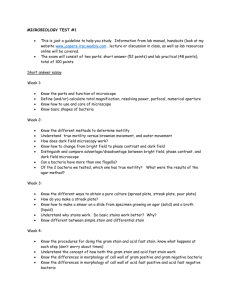
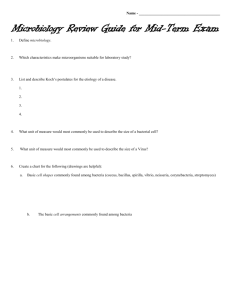
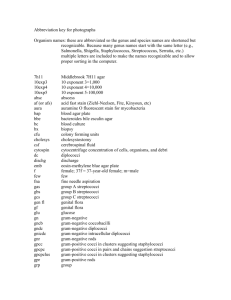
Practical Medical Microbiology PHT313 By Dr. Mohamed Al-Agamy Assistant Professor of Microbiology Department of Pharmaceutics & Microbiology College of Pharmacy King Saud University 2010/1431 Classification of Bacteria Bacteria Gram-Positive Cocci Acid fast bacteria Gram-negative Bacilli Staphylococci Streptococci Spore forming Aerobic Bacillus species Anaerobic Clostridium species Non-spore forming Other bacteria e.g. Mycoplasma, Spirochetes Staphylococci • Three important species of staphyloccoci have medical importance – S. aureus : pathogenic and commensally found in nose – S. epidermidis: non pathogenic and commensals in skin – S. saprophyticus: causes UTI in sexually active women • Rarely found in healthy humans but is commonly isolated from animals and their carcasses – S. haemolyticus: Frequently found as a commensal organism on humans and animals • It occurs infrequently as a cause of soft-tissue infections, usually in immunocompromised patients General characteristics • General characteristics • Characteristics of S. aureus – Gram Positive Cocci – Production of coagulase – Grape-like – Production of phosphatase – Non Motile – Non Spore Forming – Non Fastidious – Production of DNase – Ferment Mannitol – Facultative Anaerobes – Gelatin liquefied – Fermentative (O+/F+) – β-hemolysis on blood agar – Halotolerant – Acidification & clotting of – Catalase positive litmus milk Gram stain of Staphylococci Virulence Factors • Antigens – Protein A – Capsule – Adhesins • Enzymes – – – – – Coagulase Lipase Hyaluronidase Staphylokinase Nuclease • Toxins – – – – – – – α-Toxin β-Toxin δ-Toxin P-V Leukocidin Enterotoxin Exfoliative Toxin Toxic Shock Syndrome Toxin Laboratory Diagnosis • I- Specimen: – Pus, Urine, Stool, Blood, CSF • II- Gram Stain: – Gram positive cocci, arranged in cluster • III- Culture: – A. Blood agar (Non-Selective Media) • Colonies of S.aureus are golden yellow and -hemolytic • Colonies of S. epidermidis are non-pigmented and non-hemolytic Colonies of S. aureus showing beta hemolysis Colonies of s. epidermidis (up) showing porcelinwhite colonies as compared to S. aureus (down) the golden appearance of the colonies. This clear distinction in colony color is not seen at all times. Mannitol Salt Agar • 2. Mannitol Salt Agar (MSA) – MSA is selective and differential medium for staphylococci – MSA contains – NaCl (7.5%), as selective agent – Mannitol as a differential agent – Phenol Red (pH indicators) • turns yellow in acidic pH and turns red in alkaline pH – S. aureus ferment mannitol and give yellow colonies – S. epidermidis and S. saprophyticus do not ferment mannitol and appear red on MSA. IV- Biochemical tests 1. Catalase test • Catalase test is used to distinguished between staphylococci (positive) from streptococci (negative) • Flood the culture with drops of 3% H2O2 • Catalase-positive cultures give air bubble at once Catalase H2O + O2 (gas, ↑) H2O2 Staphylococci • The test should not be done on blood agar because blood itself will produce bubbles Catalase test Positive Negative Microcococcaceae Staphylococci Streptococcaceae Streptococci 2- Coagulase Test Principle: • This test is used to differentiate between S. aureus (CPS) & other Staphylococcus species (CNS) • This test is done by tube method or slide method Fibrinogen (Plasma) Coagulase Fibrin (Clot) Coagulase test Coagulase Positive Staphylococus aureus Coagulase-Negative S. epidermidis & S. saprophyticus • The tube coagulase test (Free): • • • Procedure: – Mix 0.1 ml of culture + 0.5 ml of plasma – Incubate at 37C for 4 h – Observing the tube for clot formation – Any degree of clotting constitutes a positive test Advantage – More accurate Disadvantage – Time consumed • The slide coagulase test • • • S. aureus Procedure: S. epidermidis – Used to detect bound coagulase or clumping factor – Add one drop heavy bacterial suspension and one drop of plasma on slide – Mixing well and observing for clumping within 10 seconds Advantage – Rapid diagnosis Disadvantage – Less accurate 3- Deoxyribonuclease (DNAase) test DNase test Positive Staphylococus aureus • • Negative S. epidermidis & S. saprophyticus Principle: – DNA is hydrolyzed into oligonucleotides by the action of DNase – S. aureus produces DNase while S. epidermidis and most staphylococci have not DNase – DNA is insoluble in acid – Nucleotides are soluble in acid Procedure & result: – Inoculate DNA agar plate with tested organism in circular motion (Spot) – Incubate at 37C for 24 h – Observe DNase activity by adding 1N HCl to the agar surface, a zone of clearing indicates a positive test – The zone represents the absence of DNA – The medium around colonies not producing DNase remains opaque, which is a reflection of the precipitation of DNA by the added acid. 4- Novobiocin Sensitivity Novobiocin test Sensitive Resistant S. aureus, S. epidermidis S. saprophyticus • Novobiocin resistance is intrinsic to S. saprophyticus but uncommon in other clinically important species. • A simple disk diffusion test for estimating novobiocin susceptibility is used to distinguish S. saprophyticus from other clinically species • Inoculated overnight culture on Mueller-Hinton agar or MSA • Add novobiocin disk on inoculated plate • Incubate at 37C overnight Differentiation between Staphylococcus species S. aureus S. epidermidis S. saprophyticus Gram stain Gram +ve cocci Gram +ve cocci Gram +ve cocci Catalase Positive Positive Positive Blood agar β-hemolysis Non-hemolytic Non-hemolytic Mannitol fermentation (MSA) Ferment mannitol Does not ferment Does not ferment Coagulase Positive Negative Negative DNAase Positive Negative Negative Novobiocin sensitivity Sensitive Sensitive Resistant Preparation of Smear and Staining • Preparation of smear – – – – – – Solid culture Liquid culture Distribute culture in slide Air dry Heat fix Ready to stain • Gram Stain – – – – – – – – – Primary Dye (C.V.) Mordant (iodine) Decolorizer (Alcohol) Counterstain (Safranin) All applied for 1 min After each step wash with water Blot dry Add one drop of immersion oil Examine under oil immersion lens Practical Work • Gram stain • Catalase test • Mannitol fermentation on MSA • DNAase Test • Tube Coagulase Test (Demo) • Novobiocin sensitivity (Demo) Streptococci • General Characteristics of Streptococci – Gram positive cocci – Chains or pairs – Usually capsulated – Non motile – Non spore forming – Facultative anaerobes – Fastidious – Fermentative (O+/F+) – Catalase negative (Staphylococci are catalase positive) Classification of Streptococci • Streptococci can be classified according to: – Oxygen requirements • Anaerobic (Peptostreptococcus) • Aerobic or facultative anaerobic (Streptococcus) – Hemolysis on Blood Agar (BA) – Serology (Lanciefield Classification) Classification Based on Hemolysis •Hemolysis on blood agar – -hemolysis • Partial hemolysis • Green discoloration around the colonies • e.g. non-groupable streptococci -hemolysis -hemolysis – S. pneumoniae & S. viridans – -hemolysis • Complete hemolysis • Clear zone of hemolysis around the colonies • e.g. Group A & B – S. pyogenes & S. agalactiae) – -hemolysis • No lysis • e.g. Group D – Enterococcus spp -hemolysis Serology: Lancefield Classification Streptococci Lanciefield classification Group A S. pyogenes Group B S. agalactiae Group C S. equisimitis Group D Enterococcus • Streptococci classified into many groups from A-K & H-U • One or more species per group • Classification based on C- carbohydrate antigen of cell wall – Groupable streptococci • A, B and D (more frequent) • C, G and F (Less frequent) – Non-groupable streptococci • S. pneumoniae (pneumonia) • viridans streptococci – e.g. S. mutans – Causing dental carries Other groups (E-U) Differentiation between -hemolytic streptococci • The following tests can be used to differentiate between hemolytic streptococci – Lancefield Classification – Bacitracin susceptibility Test • Specific for S. pyogenes (Group A) – CAMP test • Specific for S. agalactiae (Group B) Bacitracin sensitivity Test • Principle: – This test is used for presumptive identification of gp A – To distinguish between S. pyogenes (susceptible to B) & non group A such as S. agalactiae (Resistant to B) – Bacitracin will inhibit the growth of gp A Strep. pyogenes giving zone of inhibition around the disk • Procedure: – Inoculate BAP with heavy suspension of tested organism – Bacitracin disk (0.04 U) is applied to inoculated BAP – After incubation, any zone of inhibition around the disk is considered as susceptible CAMP test • Principle: – Group B streptococci produce extracellular protein (CAMP factor) – CAMP act synergistically with staph. -lysin to cause lysis of RBCs • Procedure: – Single streak of Streptococcus to be tested and a Staph. aureus are made perpendicular to each other – 3-5 mm distance was left between two streaks – After incubation, a positive result appear as an arrowhead shaped zone of complete hemolysis – S. agalactiae is CAMP test positive while non gp B streptococci are negative CAMP test Differentiation between -hemolytic streptococci • The following definitive tests used to differentiate between S. pneumoniae & viridans streptococci – Optochin Test – Bile Solubility Test – Inulin Fermentation Optochin Susceptibility Test • Principle: – Optochin (OP) test is presumptive test that is used to identify S. pneumoniae – S. pneumoniae is inhibited by Optochin reagent (<5 µg/ml) giving a inhibition zone ≥14 mm in diameter. • Procedure: – Blood agar plate is inoculated with organism to be tested – OP disk is placed on the center of inoculated BAP – After incubation at 37oC for 18 hrs, accurately measure the diameter of the inhibition zone by the ruler – ≥14 mm zone of inhibition around the disk is considered as positive and ≤13 mm is considered negative • S. pneumoniae is sensitive (S) while S. viridans is resistant (R) Optochin Susceptibility Test Optochin resistant S. viridans Optochin susceptible S. pneumoniae Bile Solubility test • Principle: – S. pneumoniae produce a self-lysing enzyme to inhibit the growth – The presence of bile salt accelerate this process • Procedure: – Add 10 parts (10 ml) of the broth culture of the organism to be tested to one part (1 ml) of 2% Na deoxycholate (bile) into the test tube – Negative control is made by adding saline instead of bile – Incubate at 37oC for 15 min – Record the result after 15 min Bile Solubility test • Results: – Positive test appears as clearing in the presence of bile while negative test appears as turbid – S. pneumoniae soluble whereas S. viridans insoluble in bile Differentiation between -hemolytic streptococci Hemolysis Bacitracin sensitivity CAMP test S. pyogenes Susceptible Negative S. agalactiae Resistant Positive Differentiation between -hemolytic streptococci Hemolysis Optochin Bile sensitivity solubility Inulin Fermentation S. pneumoniae Sensitive (≥ 14 mm) Soluble Not ferment Viridans strep Resistant (≤13 mm) Insoluble Ferment Outline of differentiation between Gram-Positive cocci e.g. S. epidermidis Practical Work • Gram stain of Streptococcus species • Hemolysis on blood agar (S. pyogenes, S. pneumoniae and Enterococcus faecalis) • Bacitracin susceptibility test (S. pyogenes and S. agalactiae) • CAMP test (S. agalactiae and S. pyogenes ) • Optochin susceptibility test (S. pneumoniae and S. viridans) • Bile solubility test (demo) Aerobic Spore Forming Bacillus spp Classification of Bacteria Bacteria Gram-Positive Cocci Acid fast bacteria Gram-negative Bacilli Staphylococci Streptococci Spore forming Aerobic Bacillus species Anaerobic Clostridium species Non-spore forming Corynebacterium Listeria Other bacteria e.g. Mycoplasma, Spirochetes Aerobic Spore Forming Bacillus spp Bacillus species Pathogenic Bacillus anthracis Bacillus cereus Non-pathogenic Bacillus subtilis Bacillus species • General Characteristics • • • • • Very large Gram positive bacilli 1-1.2 µm in width x 3-5µm in length Arranged in long chains Motile except B. anthracis Spore forming (outside the host) – Spores are central and oval Capsulated (inside the host) Non fastidious Aerobic Fermentative i.e. O+/F+ Catalase positive Natural Habitats It is found in soil habitats • • • • • • • Anthrax • Anthrax is caused by B. anthracis • Types of Anthrax – Cutanoues Anthrax (Malignant Pustule) (20% fatal) – Intestinal Anthrax – Pneumonic Anthrax (Woolsorters disease) • Virulence factors • Poly-D-glutamyl Capsule – Mediates the invasive stage of the infection – Antiphagocytic • Anthrax Exotoxins – Mediates the toxigenic stage Bacillus cereus B. cereus is a normal inhabitant of soil Isolated from foods (Grains and spices) B. cereus causes food poisoning B. cereus deposits its spores in food Bacteria germinates in food & begin releasing their exotoxins Spores are not killed during cooking The following table differentiates between Bacillus sp. Motility B. anthracis Non-motile B. cereus motile Capsule Hemolysis capsulated Non-hemolytic Non-encapsulated β-hemolytic Resistance to Penicillin S R (produce β-lactamase) Identification of Bacillus Spp. • Specimen – Pastular exudates in malignant pustule – Sputum in pneumonic anthrax – Stool in intestinal anthrax (also in food poisoning by B. cereus) • Stool specimen is emulsified and heated to 80 C to kill non spore forming microorganism • Morphology – Macroscopical (Cultural characteristics) – Microscopical (Gram Stain, Spore Stain) • Cultural Characteristics • Grow on nutrient Agar • On ordinary medium • Grow aerobically at 37C with characteristic mucoid or smooth colonies, which indicates the pathogencity of organism (presence of capsule) • Rough colonies are relatively avirulent • Stab culture on gelatin medium results in inverted fire tree appearance. • Growth on Blood Agar Bacillus anthracis colonies are non hemolytic B. cereus colonies are β-hemolytic B. subtilis colonies are β-hemolytic • Microscopical examination • Gram Stain, Capsule stain and motility – Gram positive bacilli – Found in chains – B. anthracis is not motile – B. cereus is motile – B. anthracis is capsulated inside the host • Spore Stain Bacillus spores are oval & central By spore staining (Malachite green & safranin), the spore appears green while the vegetative cells appear red. Biochemical tests 1- Catalase Test Broth Cultutre & H2O2 on the slide H2O2 added on culture grown on nutrient agar • All Bacillus species are catalase positive • Remember: staphylococci are catalase positive 2- Starch Hydrolysis (Amylase Activity) • Principle – Starch + Iodine – Glucose + Iodine • blue color No reaction Nutrient Agar containing 1% Starch + M.O Amylase Glucose Iodine Appearance of colorless zone around the growth • Procedure – Inoculate nutrient agar plate containing 1% Starch with the M.O. – Incubate the plate at 37 for overnight – After incubation, flood the plate with Iodine solution • Result – Activity of amylase is indicated by a clear zone around the growth while the rest of the plate gives blue color after addition of iodine solution Spore Stain Procedure 1. Make a heat fixed smear of Bacillus 2. Place the slide on the slide rack 3. Cover the smear with malachite green stain 4. Apply heat for 3-5 min without boiling and drying of the slide 5. Wash the slide gently in running water about 20 S 6. Counterstain with safranin for one minute 7. Gently rinse with water 8. Gently blot the slide dry, no rubbing, and let it air dry and examine with oil immersion optics. 9. Observe red vegetative cells and sporangia, and green endospores and free spores Practical Work • Gram Stain • Spore Stain • Catalase Test • Starch hydrolysis Clostridia • General Characteristics of Clostridia – Large Gram positive – Straight or slightly curved rods with slightly rounded ends – Anaerobic – Spore bearing – Fermentative, or proteolytic or both – Catalase and oxidase are negative • Natural Habitats – Their habitats are soils and animal & human gut which invade the blood and tissue when host die and initiate the decomposition of the corpse (dead body) Clostridium • Diseases – Their pathogenesis by producing potent exotoxins and enzymes which attack the neurons pathways – Rapid diagnosis is crucial or patient will die Clostridium causing Tetanus Cl. tetanii Gas gangrene Sacchrolytic Cl. perfringens Mixed Cl. histolyticus Botulism Cl. botulinum Proteolytic Cl. sporogenes Antibiotic associated diarrhea Cl. difficile Clostridium tetani causing tetanus • General characteristics of Cl. tetani – Gram positive, straight, slender rod with rounded ends – All species form endospore – Spores are terminal • drumstick with a large round end) – Fermentative – Obligate anaerobe – Motile by peritrichous flagella – Grows well in cooked meat broth and produces a thin spreading film when grown on enriched blood agar – Spores are highly resistant to adverse conditions Clostridium tetani • Causative agent • Cl. tetani is the causative agent of tetanus (Lockjaw) • Virulence factors • The patheogenis of Cl. tetani is due to potent exotoxins • Cl. tetani produces two types of toxins: • Tetanolysin, which causes lysis of RBCs • Tetanospasmin is neurotoxin Laboratory Diagnosis of Tetanus • The diagnosis of tetanus depends primarily upon the clinical manifestation of tetanus including muscle spasm & rigidity. • Specimen: – Wound exudates using capillary tube • Culture: – On blood agar and incubated anaerobically • Growth appears as a fine spreading film and β-hemolytic • Gram stain is a good method for identifying Clostridium – Cl. tetani is Gram positive rod, motile with a round terminal spore giving a drumstick appearance Clostridium Causing Gas Gangrene Clostridia causing gas gangrene Saccharolytic organisms Cl. perfringens Ferment carbohydrates Acid and gas are produced Proteolytic organisms Cl. sporogenes Digest proteins with blackening bad smell production Mixed saccharolytic & proteolytic Cl. histolyticum Clostridium perfringens • General characteristics – Large Gram-positive bacilli with stubby (short) ends – Spore forming • Spores are oval and subterminal and not bulging • Seldom to see – Capsulated – Non motile (Cl. tetani is motile) – Anaerobic • Natural habitats – Animal and human excreta – Soil Cl. perfringens Causing Gas gangrene Food poisoning (Enterotoxin) Pathogenesis (Virulence factor) • • • • Toxins of Cl. perfringens There are five different toxin types (A-E) Each type of toxin composed of different components All types of toxin contain toxin • Distribution of major toxins among types of Cl. perfringens Types of Toxins A B C D E + + + + + Components of Toxins Epsilon Iota Enterotoxin + + + + + + Laboratory Diagnosis of gas gangrene Specimen: Histological specimen or wound exudates Specimens of exudates should be taken from the deeper areas of the wound Microscopical examination (Gram, Spore stain etc) Gram-positive bacilli with blunt (not sharp) ends occurring singly or in pairs, non motile, capsulated & sporulated The spore is large, oval, central to sub-terminal & non bulging (non swelling) Spores are rarely observed Culture: Anaerobically at 37C On Robertson's cooked meat medium → blackening of meat will observed with the production of H2S and NH3 On blood agar → double zones of β-hemolytic colonies Biochemical Tests Fermentation of many sugars with acid & gas Saccharolytic organism Acidification litmus milk with stormy clot production Nagler reaction 1- Reaction on Litmus Milk Litmus Milk Contains Skimmed Milk (Without Fat) Lactose Sugar Casein Protein Litmus indicator Acid Base and Redox indicator Reaction on Litmus Milk 1- Acidic Reaction Fermentation Lactose Acid Litmus Indicator Pink Color (Milk Sugar) 2- Basic Reaction Digestion Casein (Milk Protein) Litmus Indicator Alkaline amines Blue Color Reaction on Litmus Milk Stormy Clot Formation Lactose Milk Sugar Fermentation Acid + Gas Stormy Clot Coagulation Casein Milk Protein Clot Reaction on Litmus Milk Nagler’s Reaction • This test is done to detect the lecithinase activity – The M.O is inoculated on the medium containing human serum or egg yolk (contains lecithin) – The plate is incubated anaerobically at 37 C for 24 h – Colonies of Cl. perfringens are surrounded by zones of turbidity due to lecithinase activity and the effect is specifically inhibited if Cl. perfringens antiserum containing antitoxin is present on the medium Nagler Reaction Procedure of Nagler Reaction Positive Nagler Reaction Clostridium botulinum • General Characteristics – Gram positive bacillus – Spore forming • Spores are oval and sub-terminal – Motile with peritrichous flagella – Strict anaerobic – Formidable pathogen due to; • Production of a potent neurotoxin in food • Resistance of its spores to inactivation • Natural habitats • It is widely distributed saprophyte occurring in soil, vegetables, fruits etc • Causative agent – Cl. botulinum is the causative agent of botulism – Botulism is a severe, often fatal, form of food poisoning – Botulinal toxins are among the most poisonous natural substances known – During the growth of the microorganism, toxin is liberated into the food – Toxins is classified into seven antigenic types (A-G) with types A, B and E most frequently associated with human disease • Mode of infection – Botulism results from ingestion of preformed toxin in the food – Insufficient heating in the process of preserving foods is an important factor in the causation of botulism and great care must be taken in canning factories to ensure that adequate heating is achieved in all parts of the can contents Laboratory diagnosis • The diagnosis must be suspected on clinical manifestation • The diagnosis may be confirmed by demonstration of – Organism and/or its toxin may be detected in the patient's stool or gastric contents – Organism and/or its toxin may be detected in the suspected food – Toxin may be demonstrated in the patient's blood • Samples of vomit or feces may also yield such evidence • Food or stool specimens are emulsified, heated at 80 C & inoculated on blood agar • Gram stain of the suspected colonies revealed that the organism is gram positive bacilli, motile, and sporulated – The spores are oval and sub-terminal • Toxin is detected in either food or blood by toxin-antitoxin neutralization test in mice Clostridium difficile • Cl. difficile is part of the normal intestinal flora in a small proportion of healthy persons & hospitalized patients • Exposure to antibiotics alerts the normal enteric flora, permeating overgrowth of Cl. difficile or making the patient more susceptible to exogenous acquisition of Cl. difficile. • Proliferation of Cl. difficile with localized production of their toxins in the colon leads to disease Clostridium difficile • General characteristics – Gram positive rod – Oval spores – Motile – Quite commonly in the faces of neonates, but is not generally regarded as a normal commensals of adults • Toxins – Toxin A causes diarrhea – Toxin B is cytotoxic • Disease – Antibiotic associated diarrhea – Pseudomembranous colitis Laboratory diagnosis • When a patient develops while antibiotics, Cl. difficile must be considered as a possible cause • Cl. difficile can be isolated from faces on selective media (CCFA) • Toxin can be detected in the patient's faces by immunological methods such as ELISA • Culture without demonstration of toxin has little diagnostic value • Observation of colonic pseudomembranes (white exudates on the surface of large intestine) by colonoscopy is diagnostic for pseudomembranous colitis, in which case laboratory confirmation is unnecessary Anaerobic Cultivation • 1- Anaerobic Jar • Most frequently used system for creating anaerobic atmosphere • Removal of oxygen & replacing it with inert gas • It is especially plastic jar with a tightly fitted lid • Anaerobic condition can be set up by use a commercially available H2 and CO2 generators envelop that is activated by adding water • Hydrogen and carbon dioxide will release and react with oxygen in the presence of catalyst to form water droplet • Production of heat within few minutes (detected by touching the top of the jar) and subsequent development of moisture on the wall of the jar are indications that the catalyst and generators envelop are functioning properly •Anaerobic indicator (Methylene blue) is placed in the jar •Methylene blue is blue in oxidized state (Aerobic condition) while turns colorless in reduced state (Anaerobic condition) Anaerobic Jar Candle Jar • 2. Culture Media (containing reducing agent) – Thioglycollate broth • Nonselective for cultivation of anaerobic bacteria as well as facultative anaerobes and aerobes • It contains – Pancreatic digest of casein, soy broth and glucose that enrich growth of bacteria – Sodium thioglycollate (Reducing agent) – Low percentage of agar to increase viscosity of medium – Thioglycollate and agar reduce Eh – Resazurin (redox indicator) – Cooked Meat Medium • It contains – Meat particles (prepared from heart muscles) which contain hematin & glutathione that act as reducing agent Growth on Fluid Thioglycolate Clostridium sporogenes Growing in Thioglycolate Medium Reducing agents in the medium absorb oxygen and allow obligate anaerobes to grow Reaction on Cooked Meat Medium • Saccharolytic reaction – It causes fermentation of glycogen of muscles – Production of acid and gas – Meat particles remain intact – e.g. Cl. perfergines • Proteolytic Reaction – It causes digestion of meat particles – Formation of black, foul smelling due to sulfur compounds Corynebacterium spp • General Characteristics – Gram positive bacilli, with pleomorphic, characteristic morphology (club shaped and beaded) & Chinese letters arrangement – Non motile – Non spore forming – Non capsulated – Facultative anaerobic – Breakdown glucose by oxidative and fermentative i.e. O+/F+ – C. diphtheriae is fastidious while diphtheriods are non-fastidious – Catalase positive – Oxidase negative • Habitats – C. diphtheriae inhabits nasopharynx but only on carrier state – Isolation from health human is not common – C. xerosis is normal flora of human conjuctiva, skin & nasopharynx Species of Corynebacterium Corynebacterium Pathogenic C. diphtheriae Causative agent of diphtheria Commensal "Diphtheriods" C. hofmannii, C. xerosisacne Normal flora of RT, urethra, vagina, Skin Corynebacterium diphtheriae • Diphtheria toxin • C. diphtheriae produce powerful exotoxin • The toxin inhibits protein synthesis which results in cell death • Diphtheria toxin consists of 2 subunits • The cells more affected are cardiac and nerve cells Laboratory Diagnosis Diagnosis of diphtheria Clinical Diagnosis Case Symptomatic patient Carrier Asymptomatic patient Clinical symptoms Diagnosis by Physician Laboratory diagnosis of case – Specimen: • A throat swap by gentle touch the membrane to avoid bleeding – Culture: • The swap is inoculated on – Loeffler's serum medium (serum +glucose 3:1) broth) – Blood Tellurite Agar [(BTA)(Blood + Potassium tellurite)] • The inoculated plate incubated aerobically at 37C for 24. • On Loeffler's serum medium (Non-selective media): • This medium used to stimulate; • The growth of C. diphtheriae • Production of the metachromatic granules within the cells • Cultural characteristics on BTA – It is selective medium for isolation of C. diphtheriae – 3 biotypes of C. diphtheriae are characterized on BTA – i.e. Gravis, mitis and intermedius biotypes – The most severe is the gravis biotype • Colony of gravis biotype is large, grey, non-hemolytic • Colonies of mitis biotype are small, black and hemolytic • Colonies of intemedius biotype are intermediate in size, non-hemolytic with black center & grey margin. • Morphology – Gram-positive, nonspore forming, nonmotile bacilli – Club-shaped (Coryne= club) arranged at acute angles or parallel to each other (Chinese letters appearance) – Beaded (metachromatic granules) • Stain – Gram stain: • C. diphteriae are gram positive bacilli arranged in Chinese letters form often club shaped – Polychrome methylene blue stain: • C. diphteriae appears beaded due to the presence of intercellular “Metachromatic or volutin" granules • By stain, the granules appear red while the rest of organism appears blue Loeffler’s seum Gram stain of C. diphtheriae C. diphtheriae on BTA Biochemical Reaction Catalase test • All Corynebacterium species are catalase positive (Also, Staphylococcus and Bacillus species are catalase positive) 2. Carbohydrate Fermentation Test • Principle Each species of corynebacteria has its specific carbohydrate fermentation pattern C. diphtheriae can be differentiated from other Corynebacterium species by fermentation of glucose and maltose (with production of acid only) but not ferment sucrose • Procedure • Inoculate three tubes of carbohydrate fermentation medium (broth containing one type of sugar and phenol red as the pH indicator) with the test organism • Incubate the tubes at 37 C for 24 hrs Glucose Maltose Sucrose • Result Sugar fermentation can be indicated by change of color of the medium from red to yellow due to formation of acid which decrease the pH C. diphtheriae can not ferment sucrose C. xerosis can ferment sucrose Glucose Maltose +ve Glucose +ve Maltose C. xerosis +ve +ve +ve Sucrose -ve Sucrose C. diphtheriae 3. Test for detection of toxigenicity of C. diphtheriae In Vitro: Elek’s Test • Principle: – It is toxin/antitoxin reaction – Toxin production can be demonstrated by a precipitation of exotoxin with diphtheria antitoxin • Procedure: • A strip of filter paper impregnated with diphtheria antitoxin is placed on the surface of serum agar • The organism is streaked at right angels to the filter paper • Incubate the plate at 37C for 24 hrs • Results: • After 48 hrs incubation, the Lines of precipitations antitoxin diffusing from filter paper strip and the toxigenic strains produce exotoxin, which diffuses and resulted in lines four precipitation lines radiating from intersection of the strip and the growth of organism Inoculated M.O. Positive Elek’s Test Bacteria Cocci Acid fast bacteria Gram-positive Gram-negative Bacilli Neiserria gonorrhoeae Oxidase negtaive Neisseria meningitidisi Enterobactericeae Oxidase positive Pseudomonadaceae Vibrionaceae Other bacteria e.g. Mycoplasma, Spirochetes Gram negative bacteria O/F Test Oxidative (O+/F-) Pseudomonas Fermentative (O+/F+) Enterobacteriacae Vibrioionaceae Gram negative bacteria Oxidase Test Oxidase positive Pseudomonas Vibrioionaceae Oxidase negative Enterobacteriacae General Characteristics of Enterobacteriaceae • All Enterobacteriaciae – – – – – • • • • • Gram-negative rods Ferment glucose with acid production Reduce nitrates into nitrites Oxidase negative Catalase positive Facultative anaerobic Motile except Shigellaand Klebsiella Non-capsulated except Klebsiella Non-fastidious Grow on bile containing media (MacConkey agar) Enterobacteriaceae • Some Enterobacteriaceae are true pathogens – Salmonella spp. – Shigella spp. – Yersinia spp. – Certain strains of E. coli (ETEC, EPEC, EIEC, EHEC) • Most members of the Enterobacteriaceae are opportunistic or cause secondary infections of wounds, the urinary and respiratory tracts, and the circulatory system e.g. E. coli. Classification of Enterobacteriaceae Enterobacteriaceae Lactose fermenters E. coli, Citrobacter, Klebsiella, Enterobacter Non-lactose fermenter Salmonell, Shigella Proteus, Yersinia There are several selective and differential media used to isolate distinguishes between LF & LNF The most important media are: MacConkey agar Eosin Methylene Blue (EMB) agar Salmonella Shigella (SS) agar In addition to Triple Sugar Iron (TSI) agar Identification of Enterobacteriaceae • Gram stain – All Enterobacteriaceae are Gram-negative rods – Arranged in single Biochemical reactions • Oxidase test – All members of Enterobacteriaceae are oxidase negative – Pseudomonas is oxidase positive – This test found in Pseudomonas Lab • O/F test – All members of Enterobacteriaceae are O+/F+ – Pseudomonas is O+/F– This test found in Pseudomonas Lab Differentiation between LF & NLF by Growth on MacConkey agar MacConkey agar is selective & differential medium for Enterobacteriaceae Contains Bile salts Crystal violet Inhibit growth of G+ve bacteria Cause of selectivity Lactose feremnters Pink colonies Lactose Cause of differential Neutral red pH indicator Acidic: Pink Lactose non feremnters colorless colonies Classification of Enterobacteriaceae according to lactose fermentation (growth on MacConkey Agar) Lactose Fermenters Acid Lactose Non-Fermenters No acid Neutral red Pink colonies Escherichia coli Klebsiella spp Enterobacter spp Citrobacter spp Colorless colonies Salmonella spp Shigella spp Proteus spp Yersinina spp Identification of Enterobacteriaceae by Growth on MacConkey agar • Method: – MacConkey agar is inoculated with tested organism using streak plate technique – Incubate the plate in incubator at 37 C/24 hrs • Results: – LF organism appears as pink colonies (e.g. E. coli) – NLF organism appears as colorless colonies (e.g. Shigella) MacConkey Agar Lactose non ferementers Salmonella, Shigella, Proteus Lactose ferementers E. coli, Klebsiella Reaction on Salmonella Shigella (SS) agar • • • • • • SS agar is a selective & differential medium for Salmonella and Shigella It contains Bile salts, and brilliant green dye as selective agents (inhibit G +ve) Lactose as a differential agent Neutral red as a pH indicator The formation of acid on fermentation of lactose causes the neutral red indicator to make pink colonies • Non lactose fermenting organisms are colorless on the medium • SS agar contains sodium thiosulfate and ferric ammonium citrate allows the differentiation of organisms that produce H2S – Lactose fermenters, such as E. coli, have colonies which are pink – Shigella appears transparent or amber (NLF/H2S -ve) – Salmonella appears transparent with black centers (NLF/H2S +ve) Identification of Enterobacteriaceae by Growth on SS agar • Method: – SS agar is inoculated with tested organism using streak plate technique – Incubate the plate in incubator at 37 C/24 hrs A .Klebsiella pneumoniae (LF/H2S-ve) B .Escherichia coli (LF/H2S-ve) C :Salmonella sp. (LF/H2S+ve) D :Proteus mirabilis (NLF/H2S+ve) E :Ps. aeruginosa (NLF/H2S-ve) . Growth of Enterobacteriaceae on EMB agar Coli-type colonies are very dark, almost black e.g. E. coli Reaction on Triple Sugar Iron (TSI) Agar • TSI contains – – Three different types of sugars • Glucose (1 part) • Lactose (10 part) • Sucrose (10 part) Phenol red (acidic: Yellow) • TSI dispensed in tubes with equal butt & slant • Principle – To determine the ability of an organism to attack a specific carbohydrate incorporated into a basal growth medium, with or without the production of gas, along with the determination of possible hydrogen sulphide production. • Method: – – • Inoculate TSI medium with an organism by inoculating needle by stabbing the butt and streaking the slant Incubate at 37°C for 24 hours Result: Example Reaction on TSI Result Butt color Slant color H2 S Red Red - ve Alk/Alk/(No action on sugars) - ve A/Alk/(Glucose fermented without H2S) A/Alk/+ (Glucose fermented with H2S) Yellow Yellow Yellow Red Red + ve black in butt Yellow - ve A/A/(All sugars are fermented) Non fermenter e.g. Pseudomonas LNF e.g. Shigella LNF e.g. Salmonella & Proteus LF e.g. E. coli, Klebsiella, Practical Work • Gram stain • Oxidase test • O/F test • Growth on MacConkey’s agar • Growth on EMB agar • Growth on SS agar • Reaction on TSI Identification of Enterobacteriaceae Biochemical Reactions • Indole, Methyl Red, Voges-Prosakaur, Citrate (IMViC) Tests: – The following four tests comprise a series of important determinations that are collectively called the IMViC series of reactions – The IMViC series of reactions allows for the differentiation of Enterobacteriaceae. the various members of IMViC: Indole test Principle Certain microorganisms can metabolize tryptophan by tryptophanase The enzymatic degradation leads to the formation of pyruvic acid, indole and ammonia The presence of indole is detected by addition of Kovac's reagent. Tryptophane Tryptophanase amino acids Indole + Pyurvic acid + NH3 Kovac’s Reagent Red color in upper organic layer` Method: Inoculate tryptone water with the tested microorganism Incubate at 37°C for 24 hours Result: A bright pink color in the top layer indicates the presence of indole The absence of color means that indole was not produced i.e. indole is negative After incubation interval, add 1 ml Kovacs reagent, shake the tube gently and read immediately Results of IMViC Indole test Negative Methyl Red test Positive Citrate utilization test Positive Negative Voges-Proskauer test IMViC test Methyl Red-Voges Proskauer (MR-VP) Tests Glucose (MRVP medium) Acidic pathway (MR test) Neutral pathway (VP test) Mixed Acids, pH less than 4.4 Acetylmethylcarbinol (Acetoin) Acidity is detectd by adding Methyl red indicator Acetoin is detected by adding Barrit’s reagent Method Inoculate the organism into One tube of MRVP broth Incubate the tubes at 37°C for 24 hours Pour 1/3 of the suspension into a clean tube Run MR test in the tube with 2/3 & VP test in the open tube with 1/3. Methyl red tube: Add 6-8 drops of methyl red reagent. Voges-Proskauer tube: Add 12 drops of Barritt's A (-naphthol), mix, 4 drops of Barritt's B (40% KOH) and mix Let sit, undisturbed, for at least 1hour Result MR test: Red color indicates positive test (e.g. E. coli) Yellow or orange indicates negative test (e.g. Klebsiella) VP test Appearance of crimson red color indicates positive test (Klebsiella) E. coli isolates give negative VP test Principle: Citrate Citrate Utilization Test Pyruvate CO2 + Na + H2O Na2CO3 Alkaline,↑pH Simmone’s Citrate media Contains Citrate as a sole of C source The color of medium is green Methods Streak a Simmon's Citrate agar slant with the organism Incubate at 37°C for 24 hours. Results Examine for growth (+) Growth on the medium is accompanied by a rise in pH to change the medium from its initial green color to deep blue Positive Negative Klebsiella, Enterobacter E. coli Urease Test Principal Urea Urea agar contains urea and phenol red Urease is an enzyme that catalyzes the conversion of urea to CO2 and NH3 Ammonia combines with water to produce ammonium hydroxide, a strong base which ↑ pH of the medium. ↑ in the pH causes phenol red r to turn a deep pink. This is indicative of a positive reaction for urease Urease H2O CO2 + NH3 NH4 OH ↑ in pH Phenol Red Method Streak a urea agar tube with the organism incubate at 37°C for 24 h Pink Positive test • • • Result If color of medium turns from yellow to pink indicates positive test. Proteus gives positive reaction after 4 h while Kelebsiella and Enterobacter gave positive results after 24 h Positive test Negative test Summary of morphology, cultural characteristics, and biochemical reactions of Enterobacteriaceae Gram Oxidase stain Nitrate reductase O/F MacCo nkey SS EMB E. coli -ve rod -ve +ve O+/F+ LF LF Metallic sheen Citrobacter -ve rods -ve +ve O+/F+ LF LF Dark Klebsiella -ve rods -ve +ve O+/F+ LF LF Dark Enterobacter -ve rods -ve +ve O+/F+ LF LF Dark Salmonella -ve rods -ve +ve O+/F+ NLF NLF/ H2S Colorles s Shigella -ve rods -ve +ve O+/F+ NLF NLF Colorless Proteus -ve rods -ve +ve O+/F+ NLF NLF/ H2S Colorles s Summary of morphology, cultural characteristics, and biochemical reactions of Enterobacteriaceae TSI Indole MR VP Citrate Urease Motility E. coli A/A/- +ve +ve -ve -ve -ve Motile Citrobacter A/A/- +ve +ve -ve +ve -ve Motile Klebsiella A/A/- -ve -ve +ve +ve +ve Non motile Enterobacter A/A/- -ve -ve +ve +ve +ve Motile Salmonella A/Alk/ + -ve +ve -ve +ve -ve Motile Shigella A/Alk/- -ve +ve -ve -ve -ve Non motile Proteus A/Alk/ + +ve -ve +ve +ve Motile Swarwing -ve Practical Work • Indole Test • MR test • VP test • Citrate Utilization test • Urease test Gram negative bacteria O/F Test Oxidative (O+/F-) Pseudomonas Fermentative (O+/F+) Enterobacteriacae Vibrioionaceae Gram negative bacteria Oxidase Test Oxidase positive Pseudomonas Vibrioionaceae Oxidase negative Enterobacteriacae Pseudomonas • Gram-negative bacilli belonging to Pseudomonadaceae • Motile by means of a single polar flagellum. • Non spore forming • Capsulated "Polysaccharide capsule" • Aerobic • Breakdown glucose by oxidation i.e. Oxidative (O+/F-) • Oxidase and catalase positive • Non fastidious • The most important pathogenic organism is Ps. aeruginosa • Optimum temperature is 37 C, and it is able to grow at 42 C • It is resistant to dyes, weak antiseptics, and many antibiotics • Common inhabitants of soil, water, GIT • Ps. aeruginosa is opportunistic pathogen and associated with a variety of infections including: – Urinary tract infections – Wound and burn with blue green pus – Respiratory system infections (Pneumonia) – Eye infection and may lead to blindness – Ear infection (external ear or otitis media) – Meningitis – A variety of systemic infections • Ps. aeruginosa produce two types of soluble pigments: – Pyoverdin or fluorscein: It is yellow-green pigment and fluorescent – Pyocyanin: It is a blue-green pigment and non-fluorescent Identification of Ps. aeruginosa • Laboratory diagnosis – Specimen: • Urine, pus, sputum, CSF, blood, skin swap according to the type of infection – Microscopical Examination • Gram Stain: Gram-negative rods • Motility Test: – Hanging Drop Techniques – Semisolid agar medium Motile Cultural Characteristics • On Nutrient agar: – Colonies are surrounded by bluish green coloration • On selective media "Cetermide" – Pigments are more obvious • On Blood agar – -hemolytic colonies • On MacConkey agar – Pale yellow colonies i.e. non lactose fermenters • Ps. aeruginosa able to grow at 42 C for 3 days Cultural Characteristics Ps. aeruginosa on cetrimide agar Gram Stain of Pseudomonas Ps. aeruginosa on Nutrient agar Biochemical Reactions • Oxidase positive • Breakdown glucose oxdatively • Nitrate Reductase positive (further reduction to N2) • Gelatinase positive • Utilize Citrate Oxidase Test: Principal Alternative substrate for Cytochrome Oxidize the reagent from colorless to purple color Oxidase Reagent Indophenol Cytochrome Oxidase Tetramethyl-PPheneylenediamine Colorless Pseudomonas Vibrio Purple color Play role in aerobic respiration Method: hold a piece of the oxidase test paper with forceps and touch onto an area of heavy growth Use platinum loop (not used nichrome) or wood stick Results Color change to purple within: 10 seconds = positive 10 - 60 seconds = delayed positive >60 seconds = negative Positive Negative Oxidation/Fermentation (O/F) Test • Principle : – To determine the ability of bacteria to breakdown glucose oxidative or fermentative – O/F medium (Hugh and Leifson Medium) is formulated to detect weak acids produced from saccharolytic M.O. – O/F medium contains • Sugar (glucose 1%) • Low percentage of Agar and Peptone • pH indicator (Bromothymol blue) – Alkaline Blue – Neutral Green – Acidic Yellow • O/F medium differs from carbohydrate fermentation medium to be more sensitive to detect the small amount of weak acids produced by M.O. • O/F medium is more sensitive due to: – Higher % of glucose to increase amount of acid produced – Lower % of peptone to reduce formation of alkaline amines which neutralize weak acids formed – Lower % of agar making the medium semisolid to facilitate diffusion of acid throughout the medium • Procedure • Each organism is inoculated into two tubes of glucose O/F medium • Inoculation is carried out as a stab to within 1 cm of the bottom of the tube • One of which is covered with mineral oil to exclude oxygen Incubate at 37°C for 24 hours. O/F Test: Results There are three types of reactions possible Reaction 1 Non-Saccharolytic O-/F Alcaligenes faecalis Open & covered remain green Reaction 2 Oxidative O+/FPseudomonas Open turns yellow Reaction 3 Fermentative O+/F+ Enterobacteriaceae Both turn yellow Gelatin Liquefaction Test: Principle Certain bacteria are capable of producing a proteolytic exoenzyme called gelatinase Gelatinase hydrolyze the protein (solid) to amino acids (liquid) At temperature below 25°C, gelatin will remain a gel, but if the temperature rises about 25°C, the gelatin will be liquid. Gelatin hydrolysis has been correlated with pathogenicity of some microorganisms Pathogenic bacteria may breakdown tissue & spread to adjacent tissues Pseudomonas Gelatinase Incubation at 37/overnight Nutrient gelatin Protein/Polypeptides Solid Gelatinase hydrolyze the protein to aminoacids Nutrient gelatin Amino acids Liquid at > 25 C Gelatinase Test: Procedure Stab M.O. If tube remains solid No change -ve E. coli Incubate at 37 C overnight If tube liquefied at > 25 C +ve Nutrient gelatin Ps. aeruginosa Gelatin Liquifaction Test • Method – Stab a nutrient gelatin tube with Positive test inoculums of the tested organism – Inoculated nutrient gelatin tube is incubated at 37°C for 24 h • Result – If a tube of gelatin liquefy indicates positive test (Ps. aeruginosa) – If a tube of gelatin remains solid indicates negative test (E. coli) Negative test Nitrate Reductase Test • Principle – To determine the ability of an organism to reduce nitrate to nitrites or free nitrogen gas • Method – Inoculate a nitrate broth with tested M.O. – incubate for 24 hrs at 37°C. – Add 1 ml of sulphanilic acid and 1 ml of -naphtylamine to nitrate broth tube • Result – The production of a red color occurs in the presence of nitrite indicates the ability of the organism to reduce nitrate to nitrite. – To broths showing a negative reaction add a few particles of zinc. – The appearance of a red color indicates that nitrate is still present and hence has not been reduced by the organism. – If the solution does not change color the organism has reduced the nitrate through nitrite to nitrogen gas. Nitrate Reductase Test: Principal Nitrate reductase Nitrate (NO3) Sulfanilic acid Nitrite (NO2) Nitrogen gas N2 α-naphthylamine Red diazonium salt Nitrate Reductase Test: Procedure Red color Positive Nitrate broth M.O. 1m Sulfanilic acid Red color Negative 1m -naphthylamine Incubate at 37oC for 24 hrs Zn No red color No red color Positive Nitrate Reductase Test: Results Red color after addition of sulfanilic acid & -naphtylamine Reduction of Nitrate to nitrite Red color after addition of zinc dust -ve reduction Nitrate unreduced No red color after addition of zinc dust Nitrate reduced into nitrite and further reduction to Nitrogen Practical Work ☺Gram stain ☺Growth on Cetrimide agar ☺Oxidase test ☺O/F test ☺Nitrate reductase test ☺Gelatinase test ☺Citrate Utilization Test ☺(See under Enterobacteriacea) Vibrionaceae • General characteristics – – – – – – – – Gram negative, curved, comma shaped bacilli Motile by single polar flagella Non spore forming Non capsulated Most vibrios have relatively simple growth factor requirements and grow well in alkaline pH Facultative anaerobes Fermentative i.e. O+/F+ Oxidase and catalase positive – Aquatic environment • Natural inhabitants Gram stain of Vibrio cholerae Species of Vibrio Vibrios V. parahaemolyticus Vibrio cholerae Cause Cholera O1 V. cholorae Classical type V. cholorae Allied vibrios Saprophytic Non-O1 V. cholorae Non-classical type V. El-tor Species of Vibrio • V. cholerae – V. cholerae divided serologically into 6 groups based on somatic O-antigens – V. cholerae O1 and O139 are the most important agents that cause cholera – V. El-Tor is O1 serotype that cause disease similar to cholera but milder • V. parahaemolyticus – V. parahaemolyticus is the cause of acute gastroenteritis following ingestion of contaminated seafood such as raw fish • Both V. cholerae & V. parahaemolyticus produce diarrhea, but in ways those are entirely different. – V. parahaemolyticus is an invasive organism affecting the colon – V. cholerae is noninvasive, affecting the small intestine through secretion of an enterotoxin. • Allied Vibrios are a large group of organisms; some of them are saprophytic while others cause disease in animals Vibrio cholerae • V. cholerae is the causative agent of cholera • Cholera is toxin mediated, a severe diarrheal disease caused by V. cholerae O1 & 139 serotype and others • Cholera is endemic in southern Asia (India, Pakistan, and Bangladesh), Latin America. • Transmission is by contaminated water or food through oral-fecal routes. • Incubation period of the disease is 1-4 days. Pathogenesis • V. cholerae multiply in the small intestine and cause the same disease as ETEC, but more severe • V. cholerae attach to the intestinal mucosa without invading the blood • V. cholerae secretes an enterotoxin (cholargen)that binds to a specific receptor on the intestinal mucosal cell • The toxin stimulates the activity of cAMP, resulting in active secretion of chloride and secondary loss of Na and H2O Principle Identification of V. cholerae Growth on TCBS TCBS medium is selective because High conc. of thiosulfate & citrate & strong alkalinity of this medium (pH9) Also, contains bile salts kills most intestinal commensals TCBS medium is differential because It contains sucrose It contains bromothymol blue Alkaline pH: blue Neutral pH: green Acidic pH: yellow Some species ferment sucrose & others not ferment Sucrose fermenting Vibrio spp (V. cholerae) appears as yellow colonies Sucrose non fermenting Vibrio spp (V. parahemolyticus) appears as blue to green colonies Sucrose fermentation on TCBS is the gold standard in its identification Identification of Vibrio Differentiation between SF & NSF by Growth on TCBS • Method: – TCBS agar is inoculated with tested organism recovered from alkaline peptone water using streak plate technique – Incubate the plate in incubator at 37 C/24 hrs • Results: – SF organism appears as yellow colonies (V. cholerae) – NSF organism appears as blue to green colonies (V. parahaemolyticus) Flame & Cool 2 1 3 5 4 Flame & Cool Flame & Cool Diagnosis of V. cholerae • Gram stain – Any sucrose fermenting colonies were subjected to Gram stain and oxidase test – Gram negative short rods, comma shaped, motile • Biochemical reactions: – Oxidase positive – O+/F+ – Cholera red reaction • M.O. is inoculated on nitrate peptone water and incubated at 37C overnight • V. cholorae produces indole and reduce nitrate into nitrite • Upon addition of sulfuric acid develops a red color of nitrosoindole • Serology: – Diagnosis can be confirmed as well as serotyping done by agglutination with specific antisera (O1, O139 antisera) Difference between O1 V. choleae V. cholerae Vibrio El-Tor Hemolysis Non hemolytic Hemolytic VogesProsakauer Negative Positive Polymyxin B resistance Sensitive Resistant Applied Microbiology Food Microbiology Water Milk Bacteriological Examination of water Most important water contaminants: Escherecia coli Enterococcus faecalis Clostridium welchii Bacteriological Examination of water Media used in bacteriological examination of water: for Escherecia coli use MacConkey. for Enterococcus faecalis use Glucose azide broth. for Clostridium welchii use reinforced anaerobic medium. Bacteriological Examination of water Methods used in bacteriological examination of water: Membrane Filtration Method. Determination of Most Probable Number (MPN) by dilution method. Membrane Filtration Method Using Millipore Filter Apparatus MacConkey’s agar Determination of MPN of Coliforms by Dilution Method 50 ml water sample 10 ml water sample 1 ml water sample Water Sample 50 ml DSMB 5 x 10 ml DSMB 5 x 5 ml SSMB Determination of MPN of Coliforms by Dilution Method • Results • Positive tubes are showing production of acid or gas. • Acid production is indicated by change color of tube from purple to yellow. • Gas production is detected in the Durham’s tube in the 1st bottle. Determination of MPN of Coliforms by Dilution Method Results: Gas Purple Yellow • Determine no. of coliforms per 100 ml water sample (MPN) using the standard probability table. Determination of MPN of Coliforms by Dilution Method Results: 1 3 MPN = 14 2 i.e: No. of coliform bacilli per 100 ml water sample is 14 cells.