The General Hospital - University of Leeds
advertisement

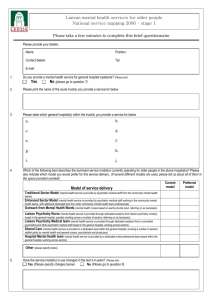
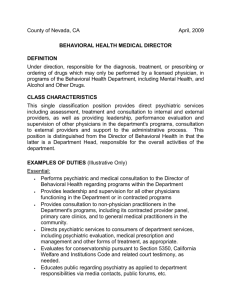
The Case of Need for OPMH Liaison Services John Holmes Senior Lecturer in Liaison Psychiatry of Old Age University of Leeds To establish a convincing case of need: • Evidence that mental health problems in older people are common in general hospitals • Evidence that outcomes are adversely affected in this group • Reasons why outcomes may be affected • Solutions that address these reasons Determining the prevalence • Comprehensive search – 576 papers identified – 256 contained original data – 97 met appraisal criteria How common is psychiatric illness in older people in general hospitals? Diagnosis Depression No. of Total Mean Prevalence studies sample sample size 27 5173 192 5–53% Mean prevalence 26% Delirium 19 4818 254 7–61% 17% Dementia 5 918 184 5–35% 13% Cognitive impairment 22 10298 468 7–88% 30% Schizophrenia 4 1147 287 1–8% 1% Alcoholism 3 583 194 1–5% 4% Total 61% Some gaps in epidemiology in GH • Self harm • Somatisation • Anxiety disorders Self harm attendances in A&E 110 of the 5038 attendances (2.2%) were by older people 900 800 700 600 500 400 300 200 100 0 <15 1519 2024 2529 3034 3539 4044 4549 Age (years) 5054 5559 6064 6569 7074 >74 University Hospitals of Leicester: • • • • • Glenfield Hospital Leicester Royal Infirmary Leicester General Hospital Total =1462 older people – 380 with depression – 249 with delirium – 190 with dementia 570 beds >1000 beds 680 beds 2250 Leeds Teaching Hospitals Trust Distribution of admissions 65 yrs 8000 7000 6000 5000 4000 3000 2000 1000 0 Geri Chest Gen Med Card Gastro Opth ENT Gen Surg Rheum Ortho Urol So… • There’s a lot of it about • What about outcomes? – systematic review – 27 studies – Outcomes affected across the board • LOS, mortality, institutionalisation, physical dependence, readmissions Survival after hip fracture… 1.0 .9 .8 .7 .6 .5 .4 Psyc h diagno sis .3 Depression (n-93) .2 Delirium(n= 108) .1 Dementia (n=294) 0.0 Well (n=208) 0 250 500 750 Time ( days) (Nightingale et al 2001, Lancet, vol. 357, no. 9264, 1264-126) As for length of stay… 1.0 .9 .8 .7 .6 .5 .4 Diagnosis .3 Depression (n=93) .2 Delirium(n= 108) .1 Dementia (n=294) 0.0 Well (n=208) 0 10 20 30 40 50 60 70 80 90 10 0 11 0 12 0 13 0 14 0 15 0 16 0 17 0 18 0 19 0 20 0 Time (days) (Holmes & House 2000, Psychol Med vol. 30, 921-929) To manage problems successfully we need: – Accurate detection by general hospital staff – Optimal management by general hospital staff • investigations • treatment • referral for specialist advice Why are things so bad 2? • We met with some general nurses: – To identify the attitudes, perceptions and training needs of general nurses relating to older people with mental health problems. – Data collection: • Focus groups with general nurses (CoE wards) – Analysis • Grounded theory approach to develop themes Theme 1 • Older people with mental health problems are identified through their behaviour. • “I suppose when I think of people mentally, with mental health problems on an elderly ward, I’m thinking about people that get violent.” • “It’s the dementias we see more of and they stand out more because they’re the one’s trying to get off the ward or mess with other people’s belongings or equipment on the ward.” • “I think we all have it don’t we? The wandering patients, which is the biggest problem really . . “ • “Outbursts of aggression” Theme 2 Physical care needs are prioritised over mental health needs •“you don’t die of confusion” •“you have to prioritise the life threatening conditions first.” •“that’s our problem on the ward, we prioritise the medical intervention, you know our focus, you know, hands on medical interventions.” •“if you’ve got 5 minutes, I don’t go and sit with a patient who I think might be getting more confused, to find out what the problem is, I think, ah, I’ve got 5 minutes, I am going to tidy up this bay because it’s a tip, because I don’t feel I have the skills to draw out from this patient.” Theme 3 Nurses perceive themselves and medical staff as lacking the skills needed to recognise and manage mental health difficulties • “ And the root of the problem is basically our education, we don’t know enough about mental conditions for us to screen and identify and therefore treat, and that’s our problem, resources aren’t available for us to be able to do that.” •“And we don’t, we don’t know enough about psychiatric illnesses to pick up exactly what it is.” •“What sections what, who? I’ve walked round with the bleep, half thinking, please God, don’t let me have to go anywhere, cos I don’t know what I’m doing.” •“I did four weeks in a day hospital and then that was it. I played Bingo and listened to The Sound of Music, and did exercises and we threw a ball at each other.” Theme 4 General nurses believe older people with mental health difficulties do not get a good service in general hospitals. “In terms of managing somebody’s mental illness, we are doing them a disservice, and if it was a medical problem, you know, it wouldn’t be tolerated, but because it’s a mental health problem it is.” “And the patients that are confused do get neglected, because you don’t give them the attention that you could give if you didn’t have your acutely unwell.” “Like taking sticks off people, and moving the table away so they can’t even get their water; cos they throw it.” Atkin et al. Int J Geriatr Psychiatry 2005; 20(11):1081-3. … and our survey of old age psychiatrists revealed deficits in: • Knowledge “How to engender some knowledge for the management of psychiatry disorders in non psychiatry areas” • Skills “Your questionnaire makes me aware of… …how much mental disorder/psychopathology/unhappiness and distress is being missed or probably dealt with inappropriately” • Attitudes “The general attitude is that anyone with a psychiatric label should be put in a corner and ignored - almost universal on surgical and orthopaedic wards” “Few referrals from surgery. I dread to think that they just over-sedate delirious patients with loads of haloperidol.” An acute trust chief executive: • Referral mechanisms SSD/Acute trusts/MHT do not address co-morbidity • Organisational boundaries get in the way of appropriate service delivery • Pressure on the acute system is not conducive to taking time and not rushing • Systems too rigid to provide care in the appropriate place for each person • Organisational cultures cause barriers more than a lack of resource Why are things so bad? • Different people interested in different outcomes: – Acute trusts – Mental health trusts – Primary care trusts – Users and carers Back to our nurses… Some solutions identified: • Training wanted, to identify and manage mental health difficulties. • Fast, direct access to a mental health professional for patient management advice. • Improve referral system to psychiatry – faster response, clear referral routes, nurses able to refer, improved follow up. • Specialist wards for older people with complex needs. So we need: – To ensure that general hospital staff are equipped to deal with the basics of mental health care • Training / education, ? supervision and – To deliver specialist mental health care where needs are more complex • Clinical service and – Input into service design • Stakeholder involvement For adults of working age: • Liaison psychiatry – Well established sub-speciality, Faculty of the RCPsych – Specific policy drivers • Health of the Nation • Self harm – Input into many different specialities • Ageist not to have the same for older people? What about old age psychiatry services? • Comprehensive – Generalist not specialist • CMHTs, day hospitals, clinics • Psychiatric wards – some general hospital based • Community focused – Because that’s where people are Potential models of general hospital care • • • • • • • Standard sector model Outreach from psychiatric wards Enhanced sector model Liaison nurse(s) Liaison psychiatrist(s) Shared care Hospital mental health team – (Clinical psychology) Our survey • Between Two Stools: Psychiatric services for older people in general hospitals – UK-wide – Old Age Psychiatrists Number of respondents Services for general hospital patients 2002 200 150 100 50 0 Traditional Enhanced sector model sector model Outreach from psychiatric w ards Liaison psychiatry nurse Liaison Shared care psychiatrist Hospital mental health team Other But… • General hospital referrals comprise 25% of the total referrals received by respondents • Many respondents gave higher priority to community referrals – perceived as higher risk • “The ones in hospital are safe and sound” • 5% able to respond in the same working day • 68% able to respond in 5 or more working days And… • 35% of respondents thought there were specialties who under-referred – in particular, orthopaedics, surgery, neurology • Why? – Inability of staff to recognise psychiatric illness – Lack of awareness of psychiatric interventions available – Need to discharge quickly, therefore don’t refer to slow to respond services – Inappropriate referral to geriatricians rather than psychiatric services Barriers to service delivery and development • Logistic – Travelling and parking – Workload • Financial – No mechanism for measuring and charging – Limited resources – Domiciliary visit fees • Organisational – Separate managerial arrangements of many trusts – Different priorities eg community – Lack of appreciation of the scale and impact of the problem • Lack of good evidence for the impact • Culture and attitudes What has changed? 2002 2006 130 120 Number of hospitalss 110 100 90 80 70 60 50 40 30 20 10 0 Traditionalsector Enhancedsector Outreach MH wards Liaison Psychiatric Liaison Psychiatric Nurse Medical Team Service model Shared Care Hospital Mental Health Team Other …and what do people want? current preferred 130 Number of hospitals 120 110 100 90 80 70 60 50 40 30 20 10 0 Traditionalsector Enhancedsector Outreach MH wards Liaison Psychiatric Nurse Liaison Hospital Mental Shared Care Psychiatric Health Team Medical Team Service model Other Non-elective LOS by PCT HRG T01 1999-2005 40 Stay in Days 35 30 25 20 15 10 5 0 West NorthWest South NorthEast East The Case of Need for OPMH Liaison Services j.d.holmes@leeds.ac.uk www.leeds.ac.uk/lpop Liaison Psychiatry for Older People: Directions and Developments, Leeds, 17 May 2007