Education Committee Newsletter EKG TOPICS Spring 2014 Down
advertisement

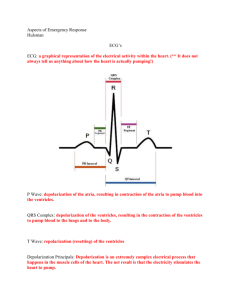
Education Committee Newsletter Down and Dirty EKGMichelle Earl Essentials of Cardiovascular Nursing at The Medical Center of the Rockies presented by Lisa Soltis, MSN & educator for MED-ED, explained an easy method for visualizing where 12 Lead EKG changes are occurring in the heart. 1st Consider how the heart lays in the chest: slightly anteriorly rotated & laying on its right side. 2nd Think of leads, AVL,AVF,I,II,III as views from a camera lens looking into the heart as they sit on the face of a clock. AVL: Looks in & down from the L shoulder @ 1:00 I: Looks in laterally @ 3:00 II: Looks inferiorly towards the heart @ 5:00 AVF: Looks up inferiorly from the feet @ 6:00 III :Looks from the Right to the inferior aspect @7:00 3rd The V leads are the views directly over the heart as the sit on the chest during the EKG. V1: Right Septal area V2:Left Septal area V2,V3,V4: Looks at the Anterior Left Ventricular area V5,V6: Looks at the Left lateral aspect. Hopefully ,visual learners will find this approach to 12 Lead EKG interpretation easier to “see”. Torsades: Becky Davis Torsades De Pointes (TdP) - is a form of Polymorphic VT which can occurred due to congenital long QT syndrome or be acquired. The definition of torsades is a EKG TOPICS ventricular rhythm which is faster than 100 beats per minute and has frequent variations of the QRS axis. Most TdP, has a progressive cyclical rotation or twist around the line hence the name Torsades De Point – “twisting around the points”. The usual presentation of TdP is a preceding prolonged QT interval in the last sinus beat which precedes the arrhythmia, shown with a ventricular rate between 160 – 250 beats per minute, with irregular RR intervals, and cycling of the QRS Axis through 180 degrees every 5 t0 20 beats. Usually the rhythm is short lived but can happen multiple times in a patient. The patients with this rhythm can potentially have the rhythm deteriorate to ventricular fibrillation and sudden cardiac death. Other risk factors that could cause TdP, hypokalemia, hypomagnesemia, and hypocalcemia. These can be seen in those patients taking antiarrhythmics, nutritionally malnourished individuals for example alcoholics and anorexic patients. Treatment for Torsades De Points depends on the presentation of the TdP. Frequently if it is drug induced patients develop prolonged QT, will be watched on an outpatient basis and changes in medication to decrease the prolonged QT. Frequently these patients will have Holter monitor or frequent intermittent EKGs to follow up. Any evidence of EKG instability, ventricular ectopy, widening QRS, TdP will require the patient to be admitted and telemetry observation for problems. Acute treatment of the patient who is awake and alert with TdP, is a brief trial of medical therapy. IV magnesium Sulfate is first line therapy for all TdP. Standard regimen is 2 grams 50% magnesium sulfate IV bolus over 2 minutes. If continues follow in 15 minutes with another bolus. Temporary transvenous overdrive pacing (atrial or ventricular) can be used for those patients who do not respond. Isoproterenol can be used according AHA guidelines for persistent TdP. For the thermodynamically unstable patient or unconscious patient, immediate defibrillation is required. Spring 2014 Finally, Brady Arrhythmias can also cause TdP and frequently these patients will have to be paced. Afib/Flutter-Amanda Puhal Flutter A-fib Afib and aflutter are atrial arrhythmias. Afib is a fast and irregular(unorganized) heart rate/rhythm. Aflutter differs from afib by being fast and regular. Common causes are alcohol use, CAD, hx of MI or bypass surgery, heart failure, valve disease, htn, medications, thyroid problems, pericarditis, or sick sinus syndrome. Afib can start or stop suddenly on its own. Sometimes cardioversion is required to get the heart back into a normal rhythm or medications. In chronic afib it is important the patient is on blood thinners to decrease the risk of stroke. STEMI/NSTEMI-Erin Pillette STEMI -Infarction with troponin elevation. -Developing complete occlusion of major coronary artery with full thickness damage to the myocardium. -Approx 70% of AMI population Diagnosis: EKG => ST Depression, transient ST elevation, T-wave inversion CK-MB => Rises after 4-6hrs and falls to normal after approx. 48-72hrs Troponin => Rises after 4-6hrs and remains elevated for up to 2wks Chest Xray => Assess for lung edema Echo => Assess for ventricular function and other complications Treatment: -Bed rest with continuous EKG monitoring -Oxygen therapy -Analgesia for pain control – i.e. morphine Education Committee Newsletter -Antiplatelet therapy such as Aspirin - ASA reduces mortality by 25% -Anticoagulation therapy such as heparin or fragmin -Beta Blockers– to reduce arrhythmias, heart rate, bp, myocardial oxygen demand, and relieve pain -Nitrates– to vasodilate and relieve pain -Statins– no matter if cholesterol levels are elevated or not -ACE Inhibitors or ARBs - ACE Inhibitors help prevent heart failure, reduce recurring infarctions, and reduce ventricular remodeling - ARBs can be used as alternatives to ACE Inhibitors -Reperfusion Therapy => within 120min Fibrinolytics ARE beneficial NSTEMI -Ischemia with troponin elevation. -Developing complete occlusion of minor coronary artery or partial occlusion of major coronary artery causing partial thickness damage to myocardium -Approx 30% of AMI population Diagnosis: EKG => ST Elevation, pathological Qwave, T-wave inversion CK-MB => Rises after 4-6hrs and falls to normal after approx. 48-72hrs Troponin => Rises at 4-6hrs and remains high for up to 2wks Chest Xray => Assess for lung edema Echo => Assess for ventricular function and for other complications Treatment: -Bed rest with continuous EKG monitoring -Oxygen therapy -Analgesia for pain control – i.e. morphine -Antiplatelet therarpy such as Aspirin -Anticoagulation therapy such as heparin -Beta Blockers – to reduce arrhythmias, heart rate, bp, myocardial oxygen demand, and relieve pain -Nitrates – to vasodilate and relieve pain -Statins – no matter if cholesterol levels are elevated or not -ACE Inhibitors or ARBs - ACE Inhibitors help prevent heart failure, reduce recurring infarctions, and reduce ventricular remodeling - ARBs can be used as alternatives to ACE Inhibitors -Angiography for further diagnosis Fibrinolytics ARE NOT beneficial EKG TOPICS RBBB/LBBB-Tre Andres In RBBB, the right bundle branch no longer conducts electricity normally, and the heart's electrical impulse enters the ventricles using only (or mainly) the left bundle branch - which means the left ventricle receives the electrical impulse first. Then, from the left ventricle, the electrical impulse finally makes its way to the right ventricle. As a result, the two ventricles no longer receive the electrical impulse simultaneously. First the left ventricle receives the electrical impulse, then the right. RBBB is a relatively common ECG finding, and while it occurs in a variety of medical conditions, it also is found in some people whose hearts are completely normal - in which case RBBB usually has no medical significance. While the presence of RBBB means that the right ventricle begins to contract slightly after the left ventricle, in normal hearts this delay in right ventricular contraction causes no measurable decrease in cardiac function. So in general isolated RBBB has no apparent medical significance, and usually can be written off as a "normal variant" and safely ignored. However, we should always educate patients to follow up with their PCP for a repeat EKG in 4-6 months. With a LBBB the left bundle branch no longer conducts electricity normally. So the electrical impulse enters the ventricles through the right bundle branch, and is carried first to the right ventricle (first panel). From there, it finally spreads to the left ventricle (second panel). Once again, the two ventricles no longer receive the electrical impulse simultaneously. First the right ventricle receives the electrical impulse, then the left. LBBB is Spring 2014 somewhat less common than RBBB, and its presence usually indicates underlying cardiac pathology. LBBB is commonly seen with dilated cardiomyopathy, hypertrophic cardiomyopathy, hypertension, aortic valve disease, CAD, and a variety of other cardiac conditions. While occasionally LBBB occurs in apparently healthy people, its appearance should trigger a thorough search (as opposed to a simple screening) for underlying cardiac problems, a new LBBB could be indicative of an MI. If the cardiac evaluation reveals no underlying heart problems, the medical significance of LBBB (especially in young people) is generally regarded as minimal. PEA-Jen Comer Pulseless electrical activity, PEA, is any organized rhythm without a pulse. This is not a shockable rhythm and requires immediate high quality CPR and intiation of ACLS guidelines for PEA. After gaining IV access, vasopressors, including Epinephrine and one dose of Vasopressin, are given simultaneously with CPR. If the PEA rate is slow, consideration may be given for dosing with atropine. Other medications may be given depending on the suspected cause of the PEA arrest. These patients have poor outcomes and their best chance of survival is to identify any reversible problems that may be causing the PEA. Consider frequent causes of PEA by recalling the H’s and T’s presented below. Analyzing the ECG may provide clues to the underlying cause of the PEA. Gathering information from friends/family could help recognize a drug overdose/poisoning. This patient population outcome depends solely on the ability of the team to provide effective CPR and identify and correct the cause of the PEA arrest. During resuscitation, the patient may go into VF or pulseless VT. This is a shockable rhythm and requires following the VF/VT pathway on the PEA algorithm. Education Committee Newsletter H’s T’s Hypovolemia Toxins Hypoxia Hydrogen (acidosis) Hyperhypokalemia Hypoglycemia ion Tamponade (cardiac) Tension pneumothorax Thrombosis (corona ry and pulmon ary) Trauma Hypothermia Narrow Complex/Rapid Rate could indicate hypovolemia, cardiac tamponade, tension pneumo-thorax, or lung thrombosis. Slow Rate would indicate hypoxia which could be related to a tension pneumo. Prolongation of QT interval would be indicative of drug overdoses or hypokalemia. WPW-Daryl Johnson Wolff-Parkinson-White syndrome is a heart condition in which there is an abnormal extra electrical pathway of the heart. The condition can lead to episodes of rapid heart rate (tachycardia). Wolff-Parkinson-White syndrome is one of the most common causes of fast heart rate disorders in infants and children. In people with Wolff-ParkinsonWhite syndrome, some of the heart's electrical signal goes down an extra (accessory) pathway. This may cause a very rapid heart rate called supraventricular tachycardia. Most people with Wolff-ParkinsonWhite syndrome do not have any other heart problems. However, this condition has been linked with other conditions, such as Ebstein's anomaly. There is also a form that runs in families. Symptoms How often the rapid heart rate occurs depends on the patient. Some people with Wolff-Parkinson-White syndrome may have just a few episodes of rapid heart rate. Others may have the rapid heart rate once or twice a week or more. Sometimes there are no symptoms, and the condition is found when a heart test is done for another EKG TOPICS reason. Spring 2014 Invitation to February’s CARDIAC CONSULT: A person with this syndrome may have: Chest pain or chest tightness Dizziness Light-headedness Fainting Palpitations (a sensation of feeling your heart beat) Shortness of breath Signs and tests Wolff-Parkinson-White syndrome may be diagnosed through continuous ambulatory ECG monitoring, such as with a Holter monitor. A test called an electrophysiologic study (EPS) is done using catheters that are threaded up to the heart from an IV placed in the leg. It may help identify the location of the extra electrical pathway. Treatment Medicine such as adenosine, antiarrhythmic drugs, and amiodarone may be used to control or prevent a rapid heartbeat. If the heart rate does not return to normal with medication, doctors may use a type of therapy called electrical cardioversion (shock). The long-term treatment for WolffParkinson-White syndrome is catheter ablation. This procedure involves inserting a tube (catheter) into an artery through a small cut near the groin up to the heart area. When the tip reaches the heart, the small area that is causing the fast heart rate is destroyed using a special type of energy called radiofrequency. Open heart surgery to burn or freeze the extra pathway may also provide a permanent cure for Wolff-ParkinsonWhite syndrome. However, surgery is usually done only if you need surgery for other reasons. Expectations (prognosis) Catheter ablation cures this disorder in most patients. The success rate for the procedure ranges between 85 and 95%. Success rates will vary depending on the location and number of extra pathways. SVT-Kellie Callahan What: When the Heart beats abnormally (at least 100 BPM, up to 300 BPM). A sudden start to the fast rhythm, and an abrupt stop, classify SVT. There are times in which patients dealing with SVT will have palpitation, syncope, bounding pulse, chest pain, nausea, and sweating. When patients become symptomatic, decreased mental status, decreased palpable pulse, immediate intervention is necessary. When: Faulty electrical connections made in the heart misfire. (Always at or above the Bundle of His) hence, the name SUPRA VENTRICULAR) Many different factors can cause SVT, including ephedrine; ETOH, caffeine or other stimulants. Other causes of SVT can include respiratory complications, such as pneumonia, and COPD. Where: Patients can go into SVT any time, and anywhere. It is appropriate as nurses, that we teach patients signs and symptoms of this hear irregularity, especially if the patient has been seen by a doctor for this in the past. Patients will often times be asked by their primary doctor to wear an “event monitor.” The patient will wear such device for a prescribed amount of time, when in which if the patient feels any palpitations, chest pain, nausea, vomiting, near syncope or rapid heart rate, the patient will push a button on the monitor, which alerts the patient’s MD electronically. At this point, they can read the patient’s EKG for that period of time, and determine if any irregularities exist. HOW TO TREAT! The most common and non-invasive attempted treatments of SVT include… Vagal Maneuvers (stimulating the Vagus nerve promotes slowed conduction of electrical impulses, which will slow the heart rate.) Vagal maneuvers include: -Bearing down -Blowing through a straw -Coughing Education Committee Newsletter Adenosine (this medication is a part of the ACLS algorithm for SVT) before you give adenosine you must….. Place patient on Zoll (cardiac pads) Have 2 Large bore AC IV’s established IV Saline hanging and infusing with NS flushes to be given immediately after drug admin Continuous EKG to determine if patient is in SVT (adenosine is given to slow the rate, so one can look at the underlying rhythm) Cycle blood pressure frequently Q3 minutes, have patient on nasal cannula 2L of O2 for comfort EXPLAIN TO PATIENT THEY WILL FEEL FUNNY FOR A SHORT AMOUNT OF TIME, BUT THOSE FEELINGS WILL PASS. Attending and Resident at bedside, wait for MD to give verbal start of medication administration. DOSE: 6mg Adenosine if that doesn’t work, repeat with 12mg of Adenosine. If patient remains in SVT, repeat once more with 12mg of Adenosine. If still in SVT and patient becomes further symptomatic, then move to Cardioversion. Cardioversion This is typically the last effort to break the patient’s arrhythmia of SVT. At this point, the patient has started to decompensate, ie: unsafe decrease in BP, decrease mental status, general condition of the patient. The MD will decide if cardioversion is necessary. At this point, you should have tried vagal maneuvers and Adenosine without any relief in symptoms. The patient will already be on the Zoll pads, BP cycling, continuous EKG, 2 large bore AC IV’s, 2L O2 via NC, and the primary RN will be educating patient regarding expectations. If time allows, the patient usually receives some pain medication, or sedative to ease the pain of the shock they are about to receive. EKG TOPICS Sinus Tachycardia-Ryan Morissette Sinus tachycardia is a commonly seen heart rhythm in the emergency department and can be caused by multiple factors. Usually this is a benign (asymptomatic) rhythm defined as a heart rate greater than 100 beats per minute (rarely greater than 160bpm), but can depend on age and physical status of patient. If the rate increases, less time is allowed for ventricular filling, and cardiac output and blood pressure can potentially be reduced. ST usually presents with increased blood pressure and cardiac output as a hyperdynamic rhythm but can decrease with decompensation. Most ST in ER patients is commonly caused by pain, fever, anxiety, dehydration, infection, drugs, withdrawal, hypoxia, anemia, exercise and many other factors. We usually see ST as a compensatory mechanism to increase cardiac output. This is caused by catecholamine release, such as epinephrine, norepinephrine, and dopamine, which act to increase impulses from the sinoatrial node to increase the ventricles rate and contractility. The rhythm itself will appear regular, rate greater than 100bpm, have normal P wave, PR interval, QRS complex, and T wave and configuration should be normal but may have a shortened QT. As the rate increases, the structures can become superimposed on each other and be difficult to identify and interpret. Generally, treatment is not needed but can include interventions for correcting reasons the patient is experiencing tachycardia. Interventions can include treatment for pain, anxiety, IV fluids for dehydration, antibiotics for infections, antipyretics, sedatives, correcting electrolyte imbalances, administering oxygen or a combination of therapies. The cause is usually multifactorial and takes investigation to figure out source with history and physical, diagnostics, and blood work and then to decide treatment options. The important thing to remember is that tachycardia (defined by patient age and status) is not normal for any average person and thus must be investigated. The longer the patient sustains this rhythm, the more their reserves are depleted and their chance Spring 2014 for a negative outcome can increase. It really depends at which point on the continuum they present to the ER and the speed at which they are diagnosed and treated. Quickly treating sinus tachycardia can help to prevent potentially life threatening consequences where the tachycardia is only a sign of a much deadlier pathology. Vfib-Nicholaus Mohr Ventricular Fibrillation (V-Fib) is a heart rhythm where the heart beats with rapid erratic electrical impulses. This causes your heart chambers to quiver uselessly instead of contracting in an organized fashion to pump blood to the body. This in turn cuts off blood supply to vital organs. Ventricular Fibrillation is frequently triggered by a heart attack. Symptoms include chest pain, rapid heartbeat, dizziness, nasuea, and shortrness of breath. Several factors put you at risk such as a previous episode of Ventricular Fibrillation, heart attack history, heart muscle damage or disease, and the use of illegal drugs such as methamphetamines and cocaine. Emergency treatments focus on restoring blood flow to the vital organs of the body, especially your brain. To accomplish this, early defibrillation and CPR are key. This will help get the heart back into a normal rhythm and help restore adequate cardiac output. Beta Blockers are often used for long term treatment of Ventricular Fibrillation. Other possible drugs such as Ace Inhibitors, Calcium Channel Blockers, and Amiodorone are also used. Implantable Cardioverter-Defibrillator (ICD) can be implanted to help your heart maintain a normal rhythm by sending electrical impulses through your heart to speed it up or slow it down. Sinus Bradycardia-Dan Evans Causes: SA node failure, athletic conditioning, SSS, MI, endocarditis, myocarditis, hypothyroidism, hyperkalemia, hypertension, medication overdose, beta blockers, antiarrhythmic Symptoms: dizziness, SOB, chest pain, hypotension, confusion, AMS Education Committee Newsletter - - A heart block is a disease in the electrical system of the heart. It can cause lightheadedness, syncope and palpitations. First degree AV block Spring 2014 Treatment: fluid challenge, medications, external pacing, correcting electrolyte imbalances Medications : Atropine, NS, epinephrine Heart Blocks-Catherine Bergstrom EKG TOPICS Regular rate and rhythm Lengthened PR interval ( >0.20 seconds) No treatment Third Degree AV block Regular , but atrial and ventricular rhythms are independent Atrial rate is usually faster The atria and ventricles beat independently Need to implant pacemaker Second degree AV block Type 1 (Mobitz I or Wenchebach) Irregular rhythm but with progressively longer PR interval PR interval get progressively longer until a QRS cycle drops off Cards consult l e m i a i n o u r Second Degree AV block Type 2 (Mobitz II) Atrial rate is regular (and faster than ventricular rate), ventricular rate is irregular More P waves than QRSs PR interval may be normal or prolonged QRS is normal or wide Cards consult r e n a l f a i l u r e o r