1-866-764-6260 - SafetyLeaders.org
advertisement

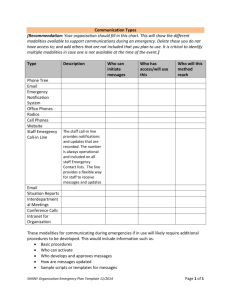
Welcome to the NQF Safe Practices for Better Healthcare 2009 Update Webinar: Clear Communication Practices for Safer Healthcare (Safe Practices 12-16) Hosted by NQF and TMIT Attendee dial-in instructions: Toll-free Call-in number (US/Canada): 1-866-764-6260 (direct number, no code needed) To join the online webinar, go to: www.safetyleaders.org Online Access Password: Webinar1 (case-sensitive) Welcome and Safe Practices Overview Hayley Burgess, PharmD Director, Performance Improvement Measures, Standards, and Practices TMIT Toll-free Call-in number: 1-866-764-6260 Safe Practices Webinar November 19, 2009 2 Panelists Hayley Burgess David W. Bates Kimberly Visconti Peter Angood Hayley Burgess: David W. Bates: Kimberly Visconti: Welcome and Safe Practices Overview Achieving Success with CPOE Using RED to Implement NQF SP 15: Discharge Peter Angood: Practical Implementation Approaches to Patient Care Information, Order Read-Back and Abbreviations, and Labeling of Diagnostic Studies Arlene Salamendra Arlene Salamendra: Roles for the Patient Advocate (Are You Listening?) 5 Culture Consent & Disclosure Consent and Disclosure Workforce Information Management and Continuity of Care Medication Management Healthcare-Associated Infections Condition- and Site-Specific Practices Toll-free Call-in number: 1-866-764-6260 Culture Structures and Systems Culture Meas., FB., and Interv. Team Training and Team Interv. ID and Mitigation Risk and Hazards CHAPTER 2: Creating and Sustaining a Culture of Patient Safety (Separated into Practices] Leadership Structures and Systems Culture Measurement, Feedback, and Interventions Teamwork Training and Team Interventions Identification and Mitigation of Risks and Hazards Consent & Disclosure Consent and Informed Consent Life-Sustaining Treatment Care of Caregiver Disclosure Workforce 2009 NQF Report Nursing Workforce Direct Caregivers CHAPTER 3: Informed Consent and Disclosure • Informed Consent • Life-Sustaining Treatment • Disclosure • Care of the Caregiver CHAPTER 4: Workforce • Nursing Workforce • Direct Caregivers • ICU Care ICU Care Legend: No Material Changes Information Management and Continuity of Care Patient Care Info. Material Changes Read-Back & Abbrev. Labeling Studies Discharge System CPOE CHAPTER 5: Information Management and Continuity of Care Patient Care Information Order Read-Back and Abbreviations Labeling Studies Discharge Systems Safe Adoption of Integrated Clinical Systems including CPOE New Medication Management CHAPTER 6: Medication Management Medication Reconciliation Pharmacist Leadership Role Including: High-Alert Med. and Unit-Dose Standardized Medication Labeling and Packaging Med. Recon. Pharmacist Systems Leadership: High-Alert, Std. Labeling/Pkg., and Unit-Dose Healthcare-Associated Infections Influenza Prevention Hand Hygiene Sx-Site Inf. Prevention VAP Prevention Central V. Cath. BSI Prevention MDRO Prevention UTI Prevention Condition-, Site-, and Risk-Specific Practices Wrong-site Sx Prevention Contrast Media Use Organ Donation Press. Ulcer Prevention Glycemic Control DVT/VTE Prevention Falls Prevention Anticoag. Therapy Pediatric Imaging CHAPTER 7: Hospital-Associated Infections • Hand Hygiene • Influenza Prevention • Central Venous Catheter-Related Blood Stream Infection Prevention • Surgical-Site Infection Prevention • Care of the Ventilated Patient and VAP • MDRO Prevention • UTI Prevention CHAPTER 8: • Wrong-Site, Wrong-Procedure, Wrong-Person Surgery Prevention • Pressure Ulcer Prevention • DVT/VTE Prevention • Anticoagulation Therapy • Contrast Media-Induced Renal Failure Prevention • Organ Donation • Glycemic Control • Falls Prevention • Pediatric Imaging 7 Achieving Success with Computerized Physician Order Entry (CPOE) David W. Bates, MD, MSc Medical Director of Clinical and Quality Analysis, Partners Healthcare Chief, Division of General Internal Medicine Brigham and Women’s Hospital Toll-free Call-in number: 1-866-764-6260 Safe Practices Webinar November 19, 2009 8 Goals • NQF Safe Practice • CPOE benefits - Drugs - Labs - Other • Meaningful use overview • CPOE risks - University of Pennsylvania (Koppel) - University of Pittsburgh (Han) • Implementing well • CPOE and the big picture • - Bar-coding Conclusions 9 Safe Practice 16: CPOE 2009 Implement a computerized prescriber order entry (CPOE) system built upon the requisite foundation of re-engineered evidence-based care, an assurance of healthcare organization staff and independent practitioner readiness, and an integrated information technology infrastructure. Toll-free Call-in number: 1-866-764-6260 10 CPOE as part of the EHR • Is centrally important because most things that occur in a hospital happen as the result of a physician’s order - Need to get physician to use the computer - Key opportunity to change behavior • Many opportunities to improve performance Toll-free Call-in number: 1-866-764-6260 11 Inpatient Prevention • 55% reduction in serious medication error rate with CPOE Bates, JAMA, 1998 • 83% reduction in overall medication error rate Bates, JAMIA, 2000 • Cost of each preventable ADE ~ $6,000 Toll-free Call-in number: 1-866-764-6260 12 Systematic Review of Impact of CPOE on Medication Safety • 5 trials of CPOE - 2 marked decrease in serious medication error rate - 1 improvement in corollary orders - 1 improvement in 5 prescribing behaviors - 1 improvement in nephrotoxic drug dose and frequency • Numerous additional studies since Kaushal, Shojania, Bates, Arch Int Med 2003 Toll-free Call-in number: 1-866-764-6260 13 Other Recent Reviews of CPOE and Medication Safety • CPOE and medication errors—66% reduction in prescribing errors on average Shamliyan et al., Health Services Res 2008 • CPOE and ADEs—ten studies, five showed decrease in ADE rates, 4 showed nonsignificant trends, 1 showed no effect Wolfstadt et al., J Gen Intern Med 2008 Toll-free Call-in number: 1-866-764-6260 14 Selected Laboratory Interventions • Charge display RCT - No statistically significant effect - BUT $1.7 million lower lab charges in intervention group • Redundant labs - 67% reminders followed - Annual charge savings $31,000, vs. estimate of $376,000 - Only 44% tests performed had computer order - Substantial improvement possible if loop closed with laboratory “back end” Toll-free Call-in number: 1-866-764-6260 15 Order Entry and Critical Paths • Critical paths specify what should happen for a specific day - Essentially sequences of order sets - In place for 25 diagnoses • Have decreased length of stay, costs, improved satisfaction • Require physicians to select diagnosis at admission - Allows prompting about path - Increases likelihood path will be selected Toll-free Call-in number: 1-866-764-6260 16 Summary of Benefits • Benefits are much greater than drug safety benefits alone - Those represent small part of financial benefits • Achieving value depends on building in good decision support - Also on ability to modify, iteratively improve Toll-free Call-in number: 1-866-764-6260 17 How to Prioritize? • ROI of inpatient CPOE evaluated • Cumulative net savings were $16.7 million over 10 years, and net operating $9.5 million • Leading contributors - Renal dosing guidance - Tools to help nurses - Specific drug guidance - Adverse drug event prevention Kaushal, JAMIA 2006 Toll-free Call-in number: 1-866-764-6260 18 Meaningful Use is Being Defined and Will Follow an “Ascension Path” 2009 2011 2013 2015 HIT-Enabled Health Reform HITECH Policies 2011 Meaningful Use Criteria (Capture/share data) 2013 Meaningful Use Criteria (Advanced care processes with decision support) *Report of sub-committee of Health IT Policy Committee 2015 Meaningful Use Criteria (Improved Outcomes) 19 Meaningful Use Matrix and Decision Support: Hospitals 2011 • 10% all orders through CPOE • Drug-drug, drug-allergy, drug-formulary checks • Up-to-date problem list • Generate lists of patients by condition • Implement one clinical decision rule related to a high-priority condition Toll-free Call-in number: 1-866-764-6260 20 Meaningful Use Matrix and Decision Support: Hospitals 2013 • • • • Use CPOE for all order types Use evidence-based order sets Conduct closed-loop medication management Use clinical decision support at the point of care • Retrieve and act on fill data Toll-free Call-in number: 1-866-764-6260 21 University of Pennsylvania: Unintended Consequences • Koppel et al. evaluated on a commercial CPOE application at U Penn and asked users about their impressions about the system - Found many situations in which “a leading CPOE system facilitated medication error risks” - Often took many screens to do things - Needed views not available • Others including Ash have also reported on this Toll-free Call-in number: 1-866-764-6260 Koppel, JAMA, 2005 22 Issues with the Koppel Study • Didn’t actually count errors or adverse events • Said that other studies focused only on advantages—not accurate • CPOE application studied was an old one • Nonetheless, paper stimulated valuable debate and identified key points - Need change systems after implementation - Software alone is insufficient Bates, J Biomed Inform, 2005 Toll-free Call-in number: 1-866-764-6260 23 University of Pittsburgh: Pediatrics Study • Studied children transported in for special care • Mortality rate increased from 2.8% to 6.3% (OR=3.3) after introduction of a commercial CPOE application • Study design was before-after - Other changes were made at same time as CPOE was implemented - Overall mortality wasn’t reported Toll-free Call-in number: 1-866-764-6260 Han, Pediatrics 2005 24 Introduction of CPOE • CPOE was introduced very rapidly—over 6 • • • • • days! After implementation, order entry wasn’t allowed until the patient had actually entered hospital and been logged into system After CPOE implementation, all drugs including vasoactive agents were moved to central pharmacy Pharmacy couldn’t process medication orders until after they were activated Many order sets weren’t available initially Result was substantial delays in care delivery Comments on Han Study • Study was very weak methodologically • Nonetheless, increase in mortality rate was very large and of obvious concern - Introducing substantial delays in this group could easily have caused • Organization broke many of the rules for implementation • Essential for other organizations to handle sociotechnical aspects better Phibbs et al., Pediatrics 2005 Toll-free Call-in number: 1-866-764-6260 26 The Path To Success in Implementing CPOE • Much is the inverse of common pitfalls - But not all • Anyone will have issues that leadership need to deal with • Keep in mind that it will be worth it - Have to pay attention to details to achieve value— doesn’t simply come with successful implementation • Is a much bigger change than anything most organizations have previously attempted on the IT front Toll-free Call-in number: 1-866-764-6260 27 Critical Success Factors in Implementation • • • • • Strong leadership and long-term commitment Creating a culture of innovation Excellent project management Attention to clinical processes A focus on quality Toll-free Call-in number: 1-866-764-6260 28 Getting Benefits— What Does It Take? • Have to have successful implementation • But also need to decide on a core of decision support - Implies having organizational structure enabling group to reach consensus • Will have to make many changes - Need architecture enabling agility - Sufficient resources to keep up - Rule is to have a long queue - Want to start low, go slow—but need to end up with enough Toll-free Call-in number: 1-866-764-6260 29 How to Assess Where You Are Regarding Decision Support • Use the AHRQ/NQF/Leapfrog assessment tool • Gives you a score regarding decision support • Without doing that hard to assess level of implementation of decision support Toll-free Call-in number: 1-866-764-6260 30 The Assessment Methodology Simulations of EHR Use with CPOE The assessment pairs medication orders that would cause a serious adverse drug event with a fictitious patient. A physician enters the order… Patient AB Female 52 years old Weighs 60 kg Allergy to morphine Normal creatinine and observes and records the type of CDS-generated advice that is given (if any). Coumadin (Warfarin) 5 mg po three times a day. Toll-free Call-in number: 1-866-764-6260 31 The Assessment Tool AHRQ/NQF/Leapfrog Assessment Tool Hospital logs on (Password access) Obtain patient criteria Complete sample test (Adult or pediatric) Program patient criteria (HM if AMB) Review patient descriptions Hospital selfreports results on website Review scoring Score generated against weighted scheme Download and print 30 – 40 test orders Enter orders into CPOE application and record results Review orders and categories Aggregate score to Leapfrog Report generated Order category scores viewed by hospital 32 Broader Context • Multiple technologies can improve medication safety - Address different stages of the process • Bar-coding • Smart pumps • Computerized monitoring for ADEs Toll-free Call-in number: 1-866-764-6260 33 Evidence Regarding Bar-coding • Increasingly widely used - About a quarter of hospitals • Very wide use in VA • Published evidence base still modest but growing • Will be included in meaningful use for 2013 • Likely to be put forward as a safe practice soon Toll-free Call-in number: 1-866-764-6260 34 Dispensing Errors and Potential ADEs: Before and After Bar-code Technology Implementation 1.00% Before Period (115164 doses observed) After Period (253984 doses observed) 0.88% 0.80% 0.61% 31% reduction* 0.60% 63% reduction* 0.40% 0.19% 0.20% 0.07% 0.00% Dispensing Error Rate * p<0.0001 (Chi-squared test) Potential ADE Rate Projections for errors prevented per year at study hospital: • >13,500 medication dispensing errors • >6,000 potential ADEs Poon et al., Annals Internal Medicine, 2006 Conclusions • CPOE appears highly beneficial in the aggregate - But can create new problems as well as prevent them • Need to monitor, engineer out • Realizing benefits requires: - Strong implementation - Later implementation of good decision support • Important not just to have but to implement well - Serial refinements in decision support • Easiest things are not highest-yield - Today’s discussion/results very important Toll-free Call-in number: 1-866-764-6260 36 Using the Re-Engineered Discharge (RED) to Implement NQF Safe Practice 15: Discharge Systems Kimberly Visconti, RN Discharge Advocate, Project RED Boston Medical Center Toll-free Call-in number: 1-866-764-6260 Safe Practices Webinar November 19, 2009 37 Background to Current Problem • Hospital discharge is non-standardized and frequently marked with poor quality • Little time spent on discharge teaching • Patients are not prepared at discharge • Poor communication between inpatient and outpatient care • Communication barriers lead to adverse events Toll-free Call-in number: 1-866-764-6260 38 39 Communication Deficits at Hospital Discharge Are Common • Discharge summary not readily available: - Only available for 12%-34% of first post-discharge appointments • Discharge summary lacking key components: - Hospital course (14.5%) - Discharge medications (21%) - Completed test results (38%) - Pending test results (65%) - Follow-up plans (14%) - Main diagnosis (17.5%) Toll-free Call-in number: 1-866-764-6260 40 Rehospitalizations and Medicare • 20% of Medicare beneficiaries who had been discharged from a hospital were readmitted within 30 days • The cost of unplanned rehospitalizations in 2004 was $17.4 billion Toll-free Call-in number: 1-866-764-6260 41 Major Changes in Hospital Payments • "Hospitals with high rates of readmission will be paid less if patients are readmitted to the hospital within the same 30-day period saving $26 billion over 10 years" Obama Administration Budget Document • MedPAC recommends reducing payments to hospitals with high readmission rates MEDPAC Testimony before Congress March ‘09 Toll-free Call-in number: 1-866-764-6260 42 NQF SP 15 Objective: “Ensure effective transfer of clinical information to the patient and ambulatory clinical providers at the time of discharge." Toll-free Call-in number: 1-866-764-6260 43 RED meets the NQF SP 15 objective using 11 mutually reinforcing components: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Patient education Follow-up appointments Outstanding tests Post-discharge services Medication reconciliation Reconcile DC plan with national guidelines What to do if problem arises Assess patient understanding Written discharge plan for patient Timely transmission of DC summary to PCP Post-discharge telephone reinforcement 44 RED Component #1 Educate patient about his/her diagnosis throughout the hospital stay • The RED intervention starts within 24 hours of the patient’s admission to the hospital and continues daily until discharge SP 15: “preparation for discharge occurring with documentation, throughout the hospitalization” 45 RED Component #2 Make appointments for clinician follow-up and post-discharge testing • Schedule PCP appt within 2 weeks after discharge • Review the provider, location, transportation, and plan to get to appointment • Consult with patient regarding best day and time for appointments • Discuss reason for and importance of all follow-up appointments and testing SP 15: “explicit delineation of roles and responsibilities in the discharge process” 46 RED Component #3 Discuss tests/studies completed and who will follow up on results • Information listed in After Hospital Care Plan (AHCP), which is transmitted to PCP • Patient knows to discuss this with PCP at follow-up appointment and where to find it on his/her AHCP SP 15: “coordination and planning for follow-up appointments that the patient can keep and follow-up of tests and studies for which confirmed results are not available at time of discharge” 47 RED Component #4 Organize post-discharge services • Communicate with case manager and social worker about post-discharge services that they schedule • Provide patient with contact information for these services (phone number, name of company, etc.) Toll-free Call-in number: 1-866-764-6260 48 RED Component #5 Confirm the Medication Plan • Reconcile the patient’s home medication list as close to admission as possible • Review each medication; make sure that the patient knows why s/he takes it • Discuss new medications each day with medical team and with patient SP 15: “completion of discharge plan and discharge summaries before discharge” 49 RED Component #6 Reconcile discharge plan with national guidelines and critical pathways • Communicate with medical team each day about the discharge plan • Recommend actions that should be taken for each patient under a given diagnosis Toll-free Call-in number: 1-866-764-6260 50 RED Component #7 Review appropriate steps for what to do if a problem arises • What constitutes an emergency • What to do if a non-emergent problem arises • Where to find contact information for the discharge advocate and PCP on the After Hospital Care Plan SP 15: “The time from discharge to the first appointment with the accepting physician represents a period of high risk. All patients discharged from hospitals should be told what to do if a question or problem arises, including whom to contact and how to contact them. Guidance should also be provided about resources for patients’ questions once they are discharged.” 51 RED Component #8 Expedite transmission of the discharge summary to the PCP • Fax the discharge summary and After Hospital Care Plan to PCP within 24 hours after discharge SP 15: “reliable information from the primary care physician (PCP) or caregiver on admission, to the hospital caregivers, and back to the PCP, after discharge, using standardized communication methods” “A discharge summary must be provided to the ambulatory clinical provider who accepts the patient’s care after hospital discharge.” 52 RED Component #9 Assess degree of understanding by asking patient to explain the details of the plan • Deliver information to reach those with low health literacy level • Include caregivers when appropriate • Utilize professional interpreters as needed SP 15: "Before discharge, present a clear explanation that the patient understands that addresses post-discharge medications, how to take them and how and where prescription can be filled. This information must also be communicated to the accepting physician.” "Use the 'teach-back process' to ensure pt understands transition-of-care planning." 53 RED Component #10 Give the patient a written discharge plan at time of discharge • After Hospital Care Plan includes: 1) Principal discharge diagnosis 2) Discharge medication instructions 3) Follow-up appointments with contact information 4) Pending test results 5) Tests that require follow-up SP 15: “coordination and planning for follow-up appointments that the patient can keep and follow-up of tests and studies for which confirmed results are not available at time of discharge” 54 David Smith 55 56 David Broitman 57 Pharmacist to call you 58 RED Component #11 Provide telephone reinforcement of the discharge plan after discharge • • • • • Call patient within 72 hours after discharge Assess patient status Review medication plan Review follow-up appointments Take appropriate actions to resolve problems SP 15: “Prospectively identify and provide a mechanism to contact patients with incomplete or complex discharge plans after discharge to assess the success of the discharge plan, address questions or issues that have arisen surrounding it, and reinforce its key components, in order to avoid postdischarge adverse events and unnecessary rehospitalizations" 59 Can Health IT assist with providing a comprehensive discharge? Toll-free Call-in number: 1-866-764-6260 60 New Horizons Using Health IT Embodied Conversational Agents • Enhance patient education before discharge • Emulate face-to-face communication • Develop therapeutic alliance • Determines competency • ECA is currently being tested at BUMC Toll-free Call-in number: 1-866-764-6260 Characters: Louise (L) and Elizabeth (R) Automated Discharge Workflow SP 15: “the development of IT systems to collect discharge information and create discharge plans from existing hospital databases could enable components of the plan to be easily collected” 62 Patient interacting with ECA Thank you! • For general information about Project RED, please refer to our website: http://www.bu.edu/fammed/projectred/ • For information about implementing RED or obtaining RED software, please contact: info@engineeredcare.com Toll-free Call-in number: 1-866-764-6260 64 Practical Implementation Approaches to Patient Care Information, Order Read-Back and Abbreviations, and Labeling of Diagnostic Studies Peter B. Angood, MD, FRCS(C), FACS, FCCM Senior Advisor, Patient Safety, National Quality Forum Toll-free Call-in number: 1-866-764-6260 Safe Practices Webinar November 19, 2009 65 Safe Practice 12: Patient Care Information Safe Practice 13: Order Read-Back and Abbreviations Safe Practice 14: Labeling of Diagnostic Studies Toll-free Call-in number: 1-866-764-6260 66 SP 12: Patient Care Information Ensure that care information is transmitted and appropriately documented in a timely manner and in a clearly understandable form to patients and to all of the patient’s healthcare providers/professionals, within and between care settings, who need that information to provide continued care. Toll-free Call-in number: 1-866-764-6260 67 SP 12: • The fragmentation of care across many providers, and an inability to access key care information for patients, results in very dangerous, yet preventable, scenarios. • One study reported that only 51% of potentially "life- threatening" critical test results received appropriate attention ... audit of patient charts revealed that 15% contained no documentation that clinicians were ever aware of the critical test result or that any corrective action was taken. • Patient care information, for the purposes of 2009, is defined as “critical information regarding medical history, diagnostic test results, medications, treatment, and procedures.” 68 SP 12: • This practice instructs organizations how to ensure that care information is appropriately documented in a timely manner and clearly communicated to patients and all of the patient's health care professionals who need that information to provide continuity of care. • This practice now includes establishing a process to communicate critical test results that are completed after the patient has been discharged from the organization. Toll-free Call-in number: 1-866-764-6260 69 SP 13: Order Read-Back and Abbreviations Incorporate within your organization a safe, effective communication strategy, structures, and systems to include the following: • For verbal or telephone orders or for telephonic reporting of critical test results, verify the complete order or test result by having the person who is receiving the information record and “read-back” the complete order or test result. • Standardize a list of “Do Not Use” abbreviations, acronyms, symbols, and dose designations that cannot be used throughout the organization. 70 SP 13: • Combined into one 2009 Safe Practice, the activities defined were merged from 2 separate 2006 Practices … combination addresses ineffective communication, which is most frequently cited category of root causes for sentinel events. • Implementing safeguards to relay accurate patient information, such as a verbal or telephone order, includes having the person receiving the information record and read back the complete order or test result. Toll-free Call-in number: 1-866-764-6260 71 SP 13: • Organizations are instructed to standardize a list of "do not use" abbreviations and dose designations that should not be used. • Though now a combined practice, it does not have substantive changes to the 2006 practice elements. Toll-free Call-in number: 1-866-764-6260 72 SP 14: Labeling of Diagnostic Studies Implement standardized policies, processes, and systems to ensure accurate labeling of radiographs, laboratory specimens, or other diagnostic studies, so that the right study is labeled for the right patient at the right time. Toll-free Call-in number: 1-866-764-6260 73 SP 14: • The potential exists for radiographs, laboratory samples, and pathology specimens to be mislabeled, or incompletely labeled, and consequently misinterpreted across all care settings. • This practice defines implementation of standardized processes to ensure accurate labeling of diagnostic studies. • No substantive changes from 2006 practice. Toll-free Call-in number: 1-866-764-6260 74 Roles for the Patient Advocate (Are You Listening?) Arlene Salamendra Patient Advocate Leader Former Board Member and Staff Coordinator, Families Advocating Injury Reduction (FAIR) Safe Practices Webinar November 19, 2009 Toll-free Call-in number: 1-866-764-6260 75 76 77 78 Upcoming Safe Practices Webinar December 17 – Optimizing a Workforce for Optimal Safe Care (Safe Practices 9-11) 79