FPM4_COHEN
advertisement
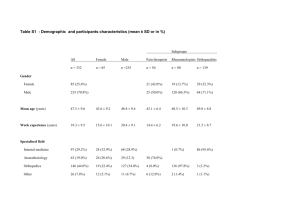
SEEKING THE DRAGON PEARL… MUSCULOSKELETAL PAIN? WRONG TARGET Milton Cohen FPMANZCA ASM, Hong Kong, May 2011 The “implementation gap” How do we use the information we have? We don’t use the evidence we have. Dr Steve Yentis, Ellis Gillespie Lecture, 14 May 2011 PSEUDODIAGNOSES • Low back pain • Musculoskeletal pain • Neuropathic pain • “Myofascial” pain • “Fibromyalgia” • Facet joint “arthritis” • Internal disc disruption • “Sciatica” • “Neuralgia” The dominant paradigm… • Biomedical focus • Anatomical determinism • Confused and confusing nomenclature …that has reached its use-by date • Biomedical focus >> “Biopsychosocial” • Anatomical determinism >> Functional appeciation • Confused nomenclature >> Rational understanding ENVIRONMENT PERSON BRAIN AND NERVOUS SYSTEM BODY ENVIRONMENT PERSON BRAIN AND NERVOUS SYSTEM BODY -social -psycho- Bio- THREE ARGUMENTS • From neurobiology • From therapeutics • From terminology CENTRAL SENSITISATION • “…once triggered remained autonomous for some time, or only required a very low level of nociceptor input to maintain it.” • “Pain…might not necessarily reflect the presence of a peripheral noxious stimulus.” • “Pain could…become the equivalent of an illusory perception…” Woolf C. Pain 2011;152:S2-S15 Yunus MB. Semin Arth Rheum 2007; 36:339-356 CLINICAL IMPLICATIONS OF CENTRAL SENSITISATION OF NOCICEPTION Diagnostic criteria Avoid chasing nociception in region of pain Nociception vs perception Words! What are we doing with drugs? Anterior cingulate cortical (ACC) activation • Thermal injury (Koyama et al 2003) • Rectal distention (Wilder-Smith et al 2004) • Hearing pain words (Osaka et al 2004) • Viewing facial expressions of pain (Botvinick et al 2005) • Social exclusion (Eisenberger et al 2003) A model regarding brain circuitry involved in the transition from acute to chronic pain. Apkarian et al. Pain 2011:152:S49-S64 HYPERVIGILANCE BRAIN AND NERVOUS SYSTEM HYPERALGESIA BODY HYPERVIGILANCE CONTEXTUAL EFFECT BRAIN AND NERVOUS SYSTEM HYPERALGESIA BODY MAINTAINING SENSITISATION THREE ARGUMENTS • From neurobiology • From therapeutics • From terminology ACUPUNCTURE • A review of reviews – Ernst et al. Pain 2011;152:755-764 • “It is becoming increasingly clear that the surrounding ritual, the beliefs of patient and practitioner and the nonspecific effects of treatment are likely responsible for any reported benefits.” – Hall, H. Commentary. Pain 2011;152:711-712 MYOFASCIAL PAIN (SYNDROME) Is it credible? • Variability of criteria used to diagnose myofascial trigger point pain syndrome - Evidence from a review of the literature. – • Tough EA et al, Clin J Pain 2007;23:278-286 Reliability of physical examination for diagnosis of myofascial trigger points: a systematic review of the literature. – Lucas N et al. Clin J Pain 2009; 25: 80-9. “Know that the best evidence for the treatment of myofascial pain is extremely limited.” IASP Curriculum • Systematic review of needling as a treatment for myofascial trigger point pain – • Cummings TM, White AR. Arch Phys Med Rehabil 2001;82:986-92 The effectiveness of non-invasive treatments for active myofascial trigger point pain: a systematic review of the literature. – Rickards LD. Int J Osteopath Med 2006; 9:120-136 “More studies are needed…” • Shoulder pain “There is some evidence from methodologically weak trials to indicate that some physiotherapy interventions are effective for some specific shoulder disorders.” (Green et al. Cochrane Database of Systematic Reviews 2003, Issue 2. Art. No.: CD004258) • Low back pain “In this systematic review, we present information relating to the effectiveness and safety of the following interventions: acupuncture, analgesics, antidepressants, back schools, behavioural therapy, electromyographic biofeedback, exercise, injections (epidural corticosteroid injections, facet joint injections, local injections), intensive multidisciplinary treatment programmes, lumbar supports, massage, muscle relaxants, non-steroidal anti-inflammatory drugs (NSAIDs), non-surgical interventional therapies (intradiscal electrothermal therapy, radiofrequency denervation), spinal manipulative therapy, surgery, traction, and transcutaneous electrical nerve stimulation (TENS).” (Chou R. Clinical Evidence [Clin Evid (Online)] 2010 Oct 08) “More studies [may not be] the answer…” • “…the positive studies are false positives…” • “No matter how many studies showed negative results, they would not persuade true believers to give up their beliefs.” – Hall, H. Commentary. Pain 2011;152:711-712. How do we use the information we have? We don’t use the evidence we have. CONCEPTUAL SHIFT Chronic “musculoskeletal” pain is attributable to altered central nociceptive and/or perceptual function rather than reflecting active peripheral pathology THREE ARGUMENTS • From neurobiology • From therapeutics • From terminology CLINICAL NOMENCLATURE • “Pain” unacceptable as a diagnosis • Biomedical matrix dominant – anatomical determinism – pseudo-mechanistic dichotomy • Where are the “-psycho-” and “-social” components A FALSE DICHOTOMY “NOCICEPTIVE” “NEUROPATHIC” REPLACING THE DICHOTOMY “NOCICEPTIVE” “NOCIPLASTIC” “NEUROPATHIC” A MATRIX FOR THE “BIO-” CONTRIBUTION [type] [site of pain] OR [hypothesis of pathogenesis] [site of clinical pain] KNEE PAIN [knee] [arthritis] [inflammatory] [knee impairment] knee “osteoarthritis” = symptomatic osteoarthrosis of the knee = biomechanical impairment of the knee on the [sufficient but not necessary] basis of osteoathrosis [biomechanical] [knee impairment] SPINAL ± REFERRED PAIN • (chronic) [low back] [pain] ?nociceptive ?neuropathic [nociplastic] [lumbar spine impairment] • leg pain in segmental distribution + signs of radiculopathy lumbar radiculopathy [radiculopathic] [leg impairment] • leg pain in non-segmental distribution with no signs of neurological deficit somatic referred pain in leg [nociplastic] [leg impairment] “CRPS” and “FIBROMYALGIA” • Complex regional “pain syndrome” of arm ? inflammatory ?neuropathic [nociplastic] [upper limb impairment] • “Fibromyalgia” or “myofascial pain” (“syndrome”) ? nociceptive neuropathic [diffuse] or [local] [nociplastic] [impairment] THREE ARGUMENTS • From neurobiology • From therapeutics • From terminology The “dragon pearl” for “musculoskeletal” pain ? “Target” is CNS and its person Transcending face validity of biomedical approach (“old paradigm”) New nomenclature required