PowerPoint Presentation - Hematology System: Biochemistry
advertisement
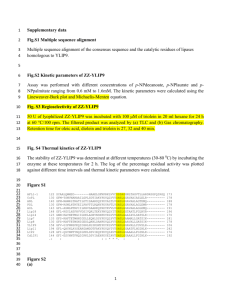
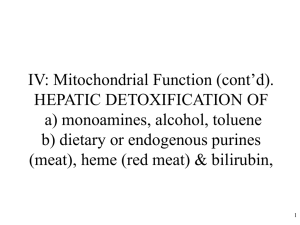
Some Biochemistry I. Metabolism of the Red Blood Cell A. Glycolysis B. Hexose Monophoshate Shunt II. Heme Synthesis and Degradation III. Anemia A. Hemolytic B. Megaloblastic C. Iron Deficiency Case 1:Peter T. History – Back Pain – Biliary Colic – Gallstones (bilirubin pigment) Presenting symptoms Malaise Palpable spleen Anemia Jaundice Peter T. Laboratory Results Red Blood Cells, x 1012/L 2.9 (5) Reticulocytes, % 15 (0.5-1.5) Hemoglobin, g/dl 8.0 (14-18) Serum Bilirubin, µmol/L 78 (2-44) • Serum bilirubin is unconjugated • Urobilinogen in urine Bilirubin Unconjugated Made in tissues Insoluble in plasma Bound to albumin Elevated in hepatic disease Elevated with hemolysis Conjugated Made in the liver Soluble Direct Elevated in biliary disease Peter T: Red Blood Cells • Spherocytes • Osmotic fragility Osmotic Fragility Harrison’s Figure 108-1 Red Blood Cell Shape Maintenance of electrolyte gradients – Fine architecture of the membrane – Supply of ATP K+ K+ ATP Na+ Na+ Peter T: Post splenectomy • Laboratory Values return to normal • Patient feels better Red Blood Cells, x 1012/L 5.4 (5) Reticulocytes, % 1 (0.5-1.5) Hemoglobin, g/dl 15.7 (14-18) Serum Bilirubin, µmol/L 8.5 (2-44) Case 2: R.P. History • Malaria • Primaquine prescribed • Black urine • Weakness • Abdominal and back pain Presenting Symptoms • Yellow sclerae • Weak • Anorexic • Vomiting R.P. Laboratory Results Red Blood Cells, x 1012/L 3.5 (5) Reticulocytes, % 12 (0.5-1.5) Hemoglobin, g/dl 9.2 (14-18) Serum Bilirubin, µmol/L 340 (2-44) • Serum bilirubin is unconjugated • Urobilinogen in urine R.P.: Red Blood Cells • Contain small dark inclusion bodies • Polymerized hemoglobin 2Hb-SH +oxidizing agent Hb Hb S S Glutathione • Tripeptide consisting of glutamic acid, cysteine (-SH group) and glycine. • Protects cells from oxidative damage • Requires NADPH for conversion from oxidized to reduced form. Glutathione and NADPH NADPH G S S G 2G SH + Hb S NADP 2G Hb S 2G SH +primaquine SH 2Hb SH + G S S G reduced primaquine + G S S G R.P.: Ten Days Later • Urine is normal color • R.P. feels better • Discharged from hospital Red Blood Cells, x 1012/L 5 (5) Reticulocytes, % 4 (0.5-1.5) Hemoglobin, g/dl 14.5 (14-18) Serum Bilirubin, µmol/L 23 (2-44) Case 3: George III History • Attacks of severe pain, excited overactivity, paralysis and delirium. • Began in 1765 (age 27) • Became frequent by 1788 Presenting symptoms • 1811, violently insane • blind pedigree Heme synthesis Harrison’s Fig. 346-1 Heme synthesis. Marks Marks Fig. 41.5 Gene Harrison’s Fig. 346-2 Porphyria Cutanea Tarda George III Precipitating Factors • Drugs • Increase in Heme Synthesis • Fasting or low carbohydrate intake Treatment • Heme • Glucose • Analgesics Case 4: Herbert B. History • Progressive anorexia • Liquid foods to avoid abdominal pain Presenting Symptoms • • • • • Loss of weight Weakness Shortness of breath Sore tongue Difficulty with swallowing • Epigastric pain • Numb, tingling hands • Palpitations Herbert B.: Laboratory Results Patient Normal 1.9 5 volume, liters per 24 h 0.3 2.5 pH 7.0 1.5 45 <4 Red blood cells, x 10 12/l Gastric secretion Urine methylmalonate, mg per 24 h Herbert B: Red Blood Cells B12 and folate Harrison’s Fig.107-2 Methionine Synthase “ folate trap” Methylmalonyl CoA mutase From ß-oxidation B12 L- Methylmalonyl CoA Succinyl CoA Methylmalonate in urine To TCA cycle and/or Heme biosynthesis B12 absorption Harrison’s Fig. 107-1 Herbert B.: Treatment IM injections of B12 monthly Herbert B.: Summary • • • • • • • • Loss of weight Weakness Shortness of breath Sore tongue Difficulty with swallowing Epigastric pain Numb, tingling hands Palpitations Case 5: Susan History • Heavy menstrual bleeding • Low fat diet-avoids red meat • “mature” multivitamin, mineral supplement Presenting Symptoms • Feels “great” • Ice chewing Susan: Laboratory Results Susan Normal 11.3 12.0 - 15.0 Hematocrit (%) 30 36 – 44 Ferritin (ng/ ml) 4.3 13 - 300 Hemoglobin (g/dl) Susan: Physical Exam • Physical exam unremarkable • Normal PAP and mammogram • Urine and stool negative for blood Iron Metabolism Harrison’s Fig. 105-1 Factors Affecting Iron Absorption • Positive – Heme vs. non heme – MFP factor or meat factor – pH- reduction of ferric to ferrous iron – Organic acids-ascorbic, malic and lactic • Negative – Phytates – Polyphenols – Fiber – Calcium Treatment • Iron supplements:325 mg (60 mg iron) PO with each meal tid • Nutrition education Some Biochemistry I. Metabolism of the Red Blood Cell A. Glycolysis B. Hexose Monophoshate Shunt II. Heme Synthesis and Degradation III. Anemia A. Hemolytic B. Megaloblastic C. Iron Deficiency Bilirubin Metabolism Marks Fig. 41.7 Normal Blood Smear Glycolysis Harrison’s Figure 108-3 Red Blood Cell Membrane Harrison’s Figure 108-2