PretermLabor1
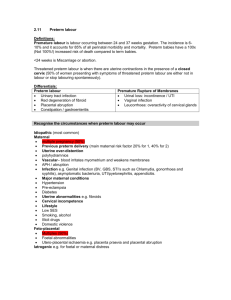
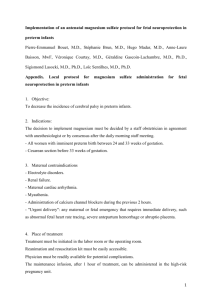
advertisement

PRETERM LABOR Solt Ido MD Preterm Labor and Delivery (<37 Weeks) Preterm Labor 800,000 (1 in 5) pregnant women exhibit signs and symptoms of preterm labor 70% of women identified as “high risk” deliver at term Preterm Delivery >452,000 (11%) of all pregnancies result in preterm birth Single largest cause of perinatal mortality and morbidity $4 to $6 billion annual acute care costs Sources: ACOG Technical Bulletin,1995, No. 206; National Vital Statistics Report 2000;48(3). St John EB et al. Am J Obstet Gynecol. 2000;182:170-175. Preterm Births United States, 1985-1998 20 Percent 15 10 5 9.8 10.0 10.2 10.2 10.6 10.6 10.8 10.7 11.0 11.0 11.0 11.0 11.4 11.6 0 1985 1986 1987 1988 1989 1990 1991 All Races 1992 1993 1994 1995 1996 1997 1998 White Note: Preterm is less than 37 weeks gestation. Source: National Center for Health Statistics, final natality data. Prepared by March of Dimes Perinatal Data Center, 2000. Black Patient Characteristics Predisposing Factors Low socioeconomic status Previous preterm birth Nonwhite race Previous abortion Maternal age <18 or >40 years Substance abuse Low prepregnancy weight No prenatal care Multiple gestation PROM Smoking Cause unknown for most cases Source: ACOG Technical Bulletin. 1995; No. 206. Etiologies of Preterm Labor Uterine Causes Cervical incompetence Uterine anomalies Uterine stretch Infectious Causes Association with chorioamnionitis Source: ACOG Technical Bulletin. 1995; No. 206. Clinical Characteristics of PTL Regular or irregular contractions Nonspecific symptoms Backache Pelvic pressure Increased vaginal discharge Bleeding Cervical exam not always informative Source: Cunningham FG et al, eds. Williams Obstetrics. 20th ed. Stamford, Conn: Appleton & Lange; 1997. Current Approach Clinical history Clinical scoring systems Risk classification High Risk Previous PTD Multiple gestation pregnancy Diabetes Hypertension disorders Patient presentation Nulliparity—Risks not established Source: Cunningham FG et al, eds. Williams Obstetrics. 20th ed. Stamford, Conn: Appleton & Lange; 1997. Survival According to Gestational Age 100 90 25 Survival, % 80 70 20 60 50 15 40 10 30 20 5 10 0 Distribution of Births, % 30 0 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 Gestational Age (weeks) Survived Frequency of Birth Source: St John EB et al. Am J Obstet Gynecol. 2000;182:170-175. Ten Leading Causes of Infant Mortality United States, 1997 Rate per 100,000 live births 159.2 Birth Defects 101.1 Preterm/LBW 77.1 SIDS 33.5 RDS 32.1 Maternal Preg. Comp. 24.7 Placenta, Cord Comp. 20.0 Infections 19.7 Accidents 11.6 Hypoxia/Birth Asphyxia 10.8 Pneumonia/Influenza 0 20 40 60 80 Source: National Center for Health Statistics, final mortality data. Prepared by March of Dimes Perinatal Data Center, 2000. 100 120 140 160 180 Commonly Used Interventions Culture/treatment for infection Bed rest on left side Hydration Tocolytic agents Lifestyle changes: Stress reduction Improve nutrition Pelvic rest No tobacco/alcohol Relaxation techniques Work modification Cerclage Home uterine monitoring Maternal transport Source: Cunningham FG et al, eds. Williams Obstetrics. 20th ed. Stamford, Conn: Appleton & Lange; 1997. Potential Benefits of Risk Assessment Markers More accurately identify women at risk Avoid unnecessary treatment Develop effective ongoing surveillance programs Avoid unnecessary expense Risk Assessment Markers Biophysical markers Measurement of cervical length Biochemical markers Fetal fibronectin (fFN) Salivary estriol (E3) Corticotropin-releasing hormone (CRH) Interleukin-6 (IL-6) Etiology Most cases are idiopathic Low socioeconomic status Nonwhite Young or advanced maternal age Low prepregnancy weight Previous preterm delivery (16-37%) Smoking, cocaine Multiple second-trimester losses Etiology Preterm rupture of membranes Has its own set of etiologies Results in preterm labor in >80% of cases Racial / Ethnic groups White patients more likely to present with preterm labor Non-white more likely to present with preterm rupture of the membranes Etiology Uterine Abnormalities Unicornate or bicornate uterus Submucosal myomata Cervical incompetence Painless cervical dilation May lead to preterm labor or PPROM DES exposure Infection? Suspected Organisms BV (Gardnerella) Chlamydia Ureaplasma Trichomonas Weak associations, no benefit of antibiotics in preventing PTL or PTD Assessing Risk Several methods advocated Cervical length studies Digital exams 2 cm dilation at 28 weeks showed increased risk in one study 1 cm dilation in early third trimester associated with increased risk Large study found 7% at 28 weeks and 32% at 32 weeks with dilation and no increased PTL or PTD Assessing Risk No screening test or “score” successful in predicting PTL with any significant positive predictive value FFN has a “useful” negative predictive value, but is NOT recommended by ACOG as a screening tool Vaginal pH, uterine monitoring; jury is out Prevention Uterine monitoring Randomized trials with conflicting data Patients benefit from the nurse visit not necessarily the uterine monitor More useful in patients with multiple gestation May be useful in patients with a history of PTL/PTD or at high risk Prevention Oral Tocolytics No benefit shown in randomized, placebo controlled trials Bed rest Most common treatment Studies show no benefit Prevention 17-P Therapy 17 alpha hydroxyprogesterone caproate Shows 37% reduction in PTL / PTD in patients with previous PTL / PTD in two large, randomized, placebocontrolled trials Start weekly injections at 16 weeks and continue until 36 weeks Not for tocolysis or adjunct therapy Risk of PTD by Cervical Length Probability of Preterm Delivery Preterm Delivery <35 Weeks 0.5 0.4 0.3 0.2 0.1 0.0 0 20 40 Cervical Length (mm) Source: Iams JD et al. N Engl J Med. 1996;334:567-572. 60 80 Risk of PTD by Cervical Length Probability of Preterm Delivery Preterm Delivery <35 Weeks 0.5 0.4 0.3 0.2 0.1 0.0 0 20 40 Cervical Length (mm) Source: Iams JD et al. N Engl J Med. 1996;334:567-572. 60 80 Fetal Fibronectin A glycoprotein secreted by fetal membranes that is found in the choriodecidual junction Responsible for cellular adhesiveness Level in cervicovaginal secretions is highly associated with preterm labor (potential or existing) and preterm delivery Source: Lockwood CJ et al. N Engl J Med. 1991;325:669-674. Fetal Fibronectin Amnion Chorion Fetal Fibronectin Decidua Fetal Fibronectin (ng/mL) Fetal Fibronectin vs Gestational Age 4500 Clinically Relevant Time Frame (22-35 weeks) 4000 3500 3000 2500 2000 1500 1000 500 0 0 5 10 15 20 25 30 Gestational Age (weeks) Source: Adapted from Garite TJ et al. Contemp Obstet Gynecol. 1996;41:77-93. 35 40 50 ng/mL Cutoff Level Conclusions NPV 99.7% before 28w NPV 96.3% before 35w PPV 31.7% at 24w Tocolysis Goals Transport to tertiary care center Administer corticosteroids Prolong pregnancy More effective when started prior to 3 cm dilation No data suggest that tocolysis improves any index of long-term prenatal or perinatal morbidity or mortality beyond steroid adminstration ? Placement of cervical cerclage Tocolysis Indications Less than 35 weeks gestation (morbidity and mortality is within 1% of term infants after 34 weeks gestation) No evidence of infection Viable No life-threatening maternal complications Tocolysis Contraindications Acute fetal distress Chorioamnionitis Severe Preeclampsia Fetal demise Maturity Maternal hemodynamic instability Tocolysis Magnesium Sulfate Most commonly used in tertiary centers Low incidence of maternal side effects Decreases smooth muscle contractility by interfering with calcium transportation (theory) No better than other tocolytics but easier to control (drip) and fewer side effects Magnesium Sulfate Dosing Try to maintain levels of 5.5-7 mg/dl Usual dose is 6g loading dose followed by 3g/hour infusion Magnesium levels can be monitored to check for theraputic range or if soft signs of toxicity are present May increase dosage if no signs of toxicity Magnesium Sulfate Contraindications Myasthenia Gravis Myasthenia Gravis MYASTHENIA GRAVIS!!!! Renal failure Severe hypocalcemia Magnesium Sulfate Side effects Maternal “flushing” or warmth Headache Nausea Dry mouth Dizziness Blurred vision Magnesium Sulfate Toxicity Loss of deep tendon reflexes (serum concentration around 8mg/dl) Mental status change / loss of consciousness Respiratory depression Pulmonary Edema Profound Hypotension Cardiac Arrhythmias Magnesium Sulfate Toxicity (continued) Treat according to symptoms NOT levels Calcium Gluconate Comes in 10 ml vials Each vial contains 4.5 mEq of Calcium Gluconate Recommended dose is 4.5-7 mEq in adults Can be given IM or in a 10% dilution IV In respiratory depression or arrest, think of the ABC’s first, then give Calcium Terbutaline Β-agonist Promotes smooth muscle relaxation May be given IV or Sub-cutaneously Rapid onset of action No better than magnesium for PTL; higher incidence of maternal side effects Terbutaline Contraindications Maternal cardiac rhythm disturbance Cardiac disease Poorly controlled diabetes Thyrotoxicosis Severe hypertension Terbutaline Side Effects / Toxicity Maternal tachycardia Fetal tachycardia Hyperglycemia, hypokalemia Hypotension Cardiac insufficiency Arrhythmias Myocardial ischemia Maternal death Terbutaline Other Uses Asthma P.O. tocolysis (not effective) Subcutaneous pump (may be effective) Uterine relaxation / fetal recussitation Indomethacin Powerful Anti-inflammatory Inhibits prostaglandin synthesis Readily crosses the placenta Often used in conjunction with other tocolytic therapy (e.g., magnesium) Shown effective in prolonging pregnancy 48-72 hours Indomethacin Contraindications Asthma Coronary artery disease GI bleed Oligohydramnios Renal failure Fetal cardiac lesion Gestational age >32 weeks Indomethacin Side effects / toxicity Rare maternal effects GI bleeding (rare) Mask fever (rare) Fetal effects May constrict ductus; most profound in patients >32 weeks May cause oligohydramnios May increase risk of IVH Other Agents Nifedipine Calcium Channel blocker Smooth muscle relaxer Torodol Anti-inflammatory More GI side effects than Indomethacin Ritodrine Only FDA approved drug for PTL Very rarely used; Β-agonist Corticosteroids For now, the ONLY evidence-based rational for tocolysis Proper course of steroids within a 48-hour period reduced the risk of neonatal IVH by greater than 50% and RDS by 28% Benefit seen prior to 34 weeks Also reduces risk for NEC, ROP, and neonatal death Corticosteroids Dosing Two IM doses of 12.5 mg Betamethasone, 24 hours apart Full benefit is reached 24 hours AFTER the second dose Also may give 6 mg Dexamethasone IM x 4 doses, 12 hours apart Increased risk of cystic para-ventricular leukomalacia and cerebral palsy with Dex Corticosteroids Controversies Multiple course administration No evidence of harm to mother or fetus No evidence of benefit over one course “Accelerated” dosing No evidence early course completion is better than single dose May be a candidate for a new course if possible Antibiotics Used ONLY to prevent Group B β-streptococcus infection in the neonate Fetus should receive two doses if possible Dosing for PCN 5 million units loading dose 2.5 million units every 4 hours May use ampicillin Use clindamycin with PCN allergy Antibiotics Massive trials show antibiotics do not increase time to delivery in PTL Culture-based use of antibiotics in pre-term labor is controversial Use PCN if at all possible; most group B strep is sensitive Summary for PTL Does the patient have PTL? Cervical exam Document advanced dilation or change Toco monitor Is the patient a candidate for tocolysis? <34 weeks Viable No contraindications Summary for PTL What method should be used? Use magnesium if not contraindicated Best tolerated Easiest dosing to control Indomethacin generally considered second line, then Terbutaline What else should be given? Steroids (ALWAYS) Antibiotics Summary for PTL What other considerations? Ultrasound for fetal weight Neonatology consultation What if the first line drug is not working? Consider gestational age Consider adding additional agent or re-bolus of current medication Note interactions CAREFULLY תודה רבה