Collecting Processing and Testing Urine Specimens
advertisement

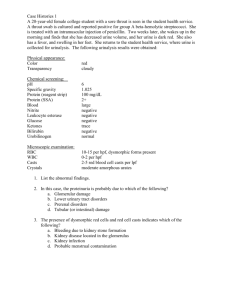
Contains few epithelial cells, occasional RBC’s, few crystals. 95% water 5% waste products Other dissolved chemicals Urea Uric acid Ammonia Calcium Creatinine Sodium Chloride Potassium Sulfates Phosphates Hydrogen ions Urochrome Urobilinogen A few RBCs A few WBCs Random urine specimen Most common Obtained any time during the day Clean-catch midstream Used for culturing urine External genitalia must be cleansed Discard small amount of urine prior to collecting specimen Can also obtain by catheterization First morning specimen Contains greater concentration of substances Timed urine specimen 24-hour specimen Discard first specimen Collect all urine for specified time Refrigerate Collected as a timed specimen Both are used for qualitative and quantitative analysis Urinary catheter – a plastic tube inserted to provide urinary drainage Catheterization – procedure by which the catheter is inserted Chemical, physical, and microscopic changes occur if urine is left at room temperature for more than 1 hour Preservation Refrigeration Prevents growth for 24 hours Return to room temperature before testing Chemical preservatives Specimens only Normal= aromatic due to the volatile fatty acids Ammonical – bacterial action Fruity- ketonuria The normal pale yellow color of urine is due to the presence of the pigment urochrome Urine color varies most commonly because of concentration, but many foods, medications, metabolic products, and infection may produce abnormal urine color. • Cloudy urine is most commonly due to phosphaturia • The large numbers of white blood cells cause the urine to become turbid. • Pyuria is readily distinguished from phosphaturia either by smelling the urine (infected urine has a characteristic pungent odor) • Rare causes of cloudy urine include chyluria (in which there is an abnormal communication between the lymphatic system and the urinary tract resulting in lymph fluid being mixed with urine), lipiduria, hyperoxaluria, and hyperuricosuria. Common Causes of Abnormal Urine Color Colorless Cloudy/milky Red Orange Very dilute urine Overhydration Phosphaturia Pyuria Chyluria Hematuria Hemoglobinuria/myoglobinuria Anthrocyanin in beets and blackberries Chronic lead and mercury poisoning Phenolphthalein (in bowel evacuants) Phenothiazines (e.g., Compazine) Rifampin Dehydration Phenazopyridine (Pyridium) Sulfasalazine (Azulfidine) Common Causes of Abnormal Urine Color Yellow Normal Phenacetin Riboflavin Green-blue Biliverdin Indicanuria (tryptophan indole metabolites) Amitriptyline (Elavil) Indigo carmine Methylene blue Phenois (e.g., IV cimetidine [Tagamet], IV promethazine [Phenergan]) Resorcinol Triamterene (Dyrenium) Brown Urobilinogen Porphyria Aloe, fava beans, and rhubarb Chloroquine and primaquine Furazolidone (Furoxone) Metronidazole (Flagyl) Nitrofurantoin (Furadantin) Brown-black Alcaptonuria (homogentisic acid) Hemorrhage Melanin Tyrosinosis (hydroxyphenylpyruvic acid) Cascara, senna (laxatives) Methocarbamol (Robaxin) Methyldopa (Aldomet) Sorbitol Ketone bodies Normally none in urine Presence Patient on a lowcarbohydrate diet Starvation Excessive vomiting Diabetes mellitus pH Normal 5.0 to 8.0 Alkaline UTI Metabolic / respiratory alkalosis Acidic Phenylketonuria Acidosis Reaction reflects ability of kidney to maintain normal hydrogen ion concentration in plasma & ECF Normal= 4.6-8 Tested by- 1.litmus paper 2. pH paper 3. dipsticks • • • • Urinary pH is measured with a dipstick test strip( methyl red and bromothymol blue), which yield clearly distinguishable colors over the pH range from 5 to 9. Urinary pH may vary from 4.5 to 8; The average pH varies between 5.5 and 6.5. A urinary pH between 4.5 and 5.5 is considered acidic, whereas a pH between 6.5 and 8 is considered alkaline. In patients with a presumed UTI, an alkaline urine with a pH greater than 7.5 suggests infection with a urea-splitting organism, most commonly Proteus. Urinary pH is usually acidic in patients with uric acid and cystine lithiasis. Alkalinization of the urine is an important feature of therapy in both of these conditions Ketosis-diabetes, starvation, fever Systemic acidosis UTI- E.coli Acidification therapy Alkaline urine Strict vegetarian Systemic alkalosis UTI- Proteus Alkalization therapy • • • • Leukocyte esterase activity indicates the presence of white blood cells in the urine. The presence of nitrites in the urine is strongly suggestive of bacteriuria The major cause of false-positive leukocyte esterase tests is specimen contamination Nitrites are not normally found in the urine, but many species of gram-negative bacteria can convert nitrates to nitrites Causes of sterile pyuria A recently (within last 2 weeks) treated urinary tract infection (UTI) or inadequately treated UTI. . UTI with 'fastidious' organism (an organism that grows only in specially fortified artificial culture media under specific culture conditions), eg Neisseria gonorrhoeae. Renal tract tuberculosis, chlamydial urethritis False negative culture due to contamination with antiseptic. False negative culture due to contamination with antiseptic. Contamination of the sample with vaginal leukocytes. Interstitial nephritis: sarcoidosis (lymphocytes not neutrophils) Urinary tract stones Renal papillary necrosis: diabetes, sickle cell disease, analgesic nephropathy. Urinary tract neoplasm, including renal cancer and bladder cancer. Polycystic kidneys. Interstitial cystitisProstatitis. Other reported associations include appendicitis, systemic lupus erythematosus and Kawasaki disease. The most common yeast cells found in urine are Candida albicans Yeasts are most commonly seen in the urine of patients with diabetes mellitus or as contaminants in women with vaginal candidiasis. Protocol for determining the need for urine sediment microscopy in an asymptomatic population Crystals in acidic urine Uric acid Calcium oxalate Cystine Leucine Crystals in alkaline urine Ammonium magnesium phosphates(triple phosphate crystals) Calcium carbonate Urinary crystals Acute Renal Failure Crystals – Pretty and important. Uric acid crystals: Seen in any setting of elevated uric acid and an acidic urine. Seen with tumor lysis syndrome. UpToDate Images. Calcium oxalate crystals: Monohydrate – dumbell shaped, may be needle-like. Dihydrate – envelope shaped. Form independent of urine pH. Seen acutely in ethylene glycol ingestion. Casts Urinary casts are cylindrical aggregations of particles that form in the distal nephron, dislodge, and pass into the urine. In urinalysis they indicate kidney disease. They form via precipitation of Tamm-Horsfall mucoprotein which is secreted by renal tubule cells. Casts • Tamm-Horsfall mucoprotein is the basic matrix of all renal casts; it originates from tubular epithelial cells and is always present in the urine • When the casts contain only mucoproteins, they are called hyaline casts and may not have any pathologic significance. • Red blood cell casts contain entrapped erythrocytes and are diagnostic of glomerular bleeding, most likely secondary to glomerulonephritis Casts • White blood cell casts are observed in acute glomerulonephritis, acute pyelonephritis, and acute tubulointerstitial nephritis • Granular and waxy casts result from further degeneration of cellular elements. Fatty casts are seen in nephrotic syndrome, lipiduria, and hypothyroidism. • Acellular casts Hyaline casts Granular casts Waxy casts Fatty casts Pigment casts Crystal casts Cellular casts Red cell casts White cell casts Epithelial cell cast The most common type of cast, hyaline casts are solidified Tamm-Horsfall mucoprotein secreted from the tubular epithelial cells Seen in fever, strenuous exercise, damage to the glomerular capillary waxy casts suggest severe, longstanding kidney disease such as renal failure(end stage renal disease). Granular casts Granular casts can result either from the breakdown of cellular casts or the inclusion of aggregates of plasma proteins (e.g., albumin) or immunoglobulin light chains indicative of chronic renal disease Introduction to casts… Hyaline Casts: Better seen with low light. Non-specific. Composed of TammHorsfall mucoprotein. waxy casts suggest severe, longstanding kidney disease such as renal failure(end stage renal disease). Granular Casts: Represent degenerating cellular casts or aggregated protein. Nonspecific. UpToDate Images. Waxy Casts: Smooth appearance. Blunt ends. May have a “crack”. Felt to be last stage of degenerating cast – representative of chronic disease. Formed by the breakdown of lipid-rich epithelial cells, these are hyaline casts with fat globule inclusions They can be present in various disorders, including nephrotic syndrome, diabetic or lupus nephropathy, Acute tubular necrosis Formed by the adhesion of metabolic breakdown products or drug pigments Pigments include those produced endogenously, such as hemoglobin in hemolytic anemia, myoglobin in rhabdomyolysis, and bilirubin in liver disease. Though crystallized urinary solutes, such as oxalates, urates, or sulfonamides, may become enmeshed within a hyaline cast during its formation. The clinical significance of this occurrence is not felt to be great. The presence of red blood cells within the cast is always pathologic, and is strongly indicative of glomerular damage. They are usually associated with nephritic syndromes. Indicative of inflammation or infection, pyelonephritis acute allergic interstitial nephritis, nephrotic syndrome, or post-streptococcal acute glomerulonephritis White Blood Cell Casts: Raises concern for interstitial nephritis. Can be seen in other inflammatory disorders. Also seen in pyelonephritis. UpToDate Images.