Antibiotic resistance
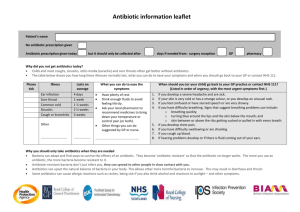
advertisement

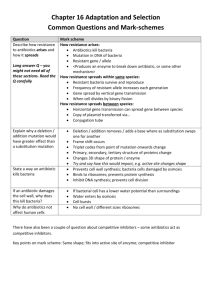
The evolution of antibiotic resistance Rob Knell / Lars Chittka MRSA in the UK Deaths per year Source: Health Protection Agency MRSA - Methicillin resistant Staphylococcus aureus -S. aureus is a common bacterium that can be found on the skin of many healthy people -it typically causes only minor infections (in “pimples” but can also cause serious diseases (e.g. pneumonia)) -First report of resistance to penicillin in 1947 -MRSA is also resistant to ampicillin and other penicillins, erythromycin, tetracycline -can only be treated with Vancomycin -Vancomycin-resistant strains have already been found and bred Examples of resistant bacteria •Mycobacterium tuberculosis: causes TB • Originally controlled with Streptomycin • Now often resistant to a variety of antibiotics • The frequency of multi-drug resistant TB in the late 1990s was 1.2% in the UK • Multi-drug resistant TB requires the patient to be given a two-year course of therapy • This costs >£60,000, whereas non-resistant TB costs about £6,000 to treat What are antibiotics? • Have been used by fungi to kill bacteria for many millions of years • First discovered in 1929 by A. Fleming • Brought into widespread use in the 1940s • Antibiotics are chemicals that kill bacteria • Their introduction was arguably the biggest medical breakthrough since sanitation Penicillin A discovery by accident • A fungal spore that the wind might have blown into his lab while Fleming was on vacation in 1928, forever changed the course of medicine... • A. Fleming named the substance Penicillin, after the mould Penicillium notatum – but was unable to isolate the substance • In the late 1930s and early 1940s, E. Chain & H. Florey managed to produce larger amounts of penecillin, and ran successful trials on mice • Nobel prize in 1945 • http://nobelprize.org/medicine/educatio nal/penicillin/readmore.html Antibiotic use and misuse •During the 1940s and 1950s antibiotics were extremely effective •They were (and still are) widely prescribed, often for medical conditions that did not require them •Antibiotics started to be used in agriculture: dosing cattle with antibiotics increases yield, and battery farming relies on antibiotics to control infection •By the 1970s the World was awash with antibiotics. Antibiotic use and misuse "There was complacency in the 1980s. The perception was that we had licked the bacterial infection problem. Drug companies weren't working on new agents. They were concentrating on other areas, such as viral infections. In the meantime, resistance increased to a number of commonly used antibiotics, possibly related to overuse of antibiotics. In the 1990s, we've come to a point for certain infections that we don't have agents available." Michael Blum, M.D., medical officer in the Food and Drug Administration's division of anti-infective drug products. Quoted in Lewis, R. (1995)The Rise of Antibiotic-Resistant Infections. Available online at http://www.fda.gov/fdac/features/795_antibio.html Resistance •As early as 1946, scientists (including A. Fleming) were warning of the possible dangers of antibiotic-resistant bacteria •A few bacteria in populations that have never been exposed to artificial antibiotics probably carry alleles that give resistance to antibiotics •Resistance alleles can also arise by mutation •Resistant bacteria can use a number of mechanisms to overcome antibiotics Mechanisms of resistance Imipenem resistant Pseudomonas aeruginosae Streptococcus pneumoniae resistance to penicillins Tetracycline MRSA penicillin binding protein PBP2A Penicillins, Cephalosporins Hawkey, P. M BMJ 1998;317:657-660 Evolution of resistance •Antibiotic use represents a strong selection pressure •If a population of bacteria with a few resistant individuals is exposed to a lethal antibiotic, the susceptible bacteria will die, but the resistant bacteria will survive •In an environment with a lot of antibiotic use, resistance alleles spread rapidly •The problem is compounded by horizontal gene transfer and by cross-resistance Horizontal transfer •Simple selection isn’t the only means for resistance alleles to spread •Bacteria can acquire resistance genes by transformation, when they pick up DNA from the environment •They can also get resistance genes by conjugation: bacterial sex, when they exchange plasmids •Plasmids can have multiple resistance genes, conferring multiresistance Cross-resistance •Resistance to one antibiotic can confer resistance to others •Resistance to cephalosporins gives resistance to methicillin, even in bacteria that have never been exposed to methicillin Managing resistance •There are two different approaches to managing antibiotic resistance: 1.Managing existing resistant pathogens 2.Avoiding future evolution of more resistance •The first can be done by, in the case of MRSA, improving hygiene in hospitals, screening hospital visitors and isolating patients •The second can be done by changing selection on bacteria Selection and resistance •Reduce inappropriate prescription of antibiotics • Increase public awareness that many diseases cannot be cured with antibiotics •Reduce use of agricultural antibiotics •Increase the number of patients who finish their courses of antibiotics •Restrict the use of new antibiotics •Where possible, use other treatments: • Vaccines • Phage treatment? Mechanisms of resistance • 1. Antibiotic modification: some bacteria have enzymes that cleave or modify antibiotics: e.g. b lactamase inactivates penicillin • 2. Denied access: membrane becomes impermeable for antibiotic: e.g. imipenem • 3. Pumping out the antibiotic faster than it gets in: e.g. tetracyclines • 4. Altered target site: antibiotic cannot bind to its intended target because the target itself has been modified • 5. production of alternative target (typically enzyme): e.g. Alternative penicillin binding protein (PBP2a) in MRSA