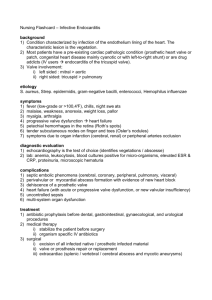
Stem Cell–Based, TEHV Implantation Into the Aortic
advertisement

ENDOVASCULAR DEVICE TO DECALCIFY AND REGENERATE HEART VALVES SO A PATIENT MAY KEEP THEIR OWN INSTEAD OF GETTING AN IMPLANT OUR APPROACH #1 - Debulk calcification with dental burr on tip of deflecting tip catheter. #2 – Ultrasonically clean entire area. #3 - Deliver microcurrent regeneration signal via flexible fiberoptic probe = recruits stem cells and differentiates them = regenerates valve and surrounding tissues. #4 – If the above fails implant autologous cell tissue engineered heart valve with key hole surgery or percutaneously OR cell sod OR glue a leaflet extension in place constructed of Goal = clean & regenerate the type of calcified valves on right to look and function like the clean healthy valve on the far left. STEM CELLS TO REPAIR HEART VALVES EMBRYONIC DEVELOPMENT OF HEART VALVES EMBRYONIC DEVELOPMENT OF HEART VALVES HOW TO MAKE A HEART VALVE: FROM EMBRYONIC DEVELOPMENT TO BIOENGINEERING OF LIVING VALVE SUBSTITUTES DONAL MACGROGAN1, GUILLERMO LUXÁN1, ANITA DRIESSEN-MOL2, CARLIJN BOUTEN2, FRANK BAAIJENS2 AND JOSÉ LUIS DE LA POMPA1 Early stages of heart development. (A) Central views of the developing mouse embryo. At E7.0, cardiac progenitors (red) have reached the head folds and, by E7.5, two cardiac lineages can be distinguished: the first heart field (FHF) (red) and the second heart field (SHF) (blue). At E8.0, the FHF progenitors merge to form the heart tube, which elongates at arterial and venous poles by the addition of progenitor cells from the second heart field (SHF). Between E8.0 and E9.0, the heart tube undergoes rightward looping. (B) Central view of the E9.5 heart, which consists of four anatomically distinct regions: atrium (At), atrioventricular canal (AVC), ventricle (V), and the outflow tract (OFT). (C) Longitudinal section depicting the prevalvular ECs. Two elongated cushions can be seen in the OFT, consisting of proximal (conal cushions, purple) and distal (truncal ridges, green) sections. The AVC has four cushions: right lateral (rlAVC), left lateral (llAVC), superior (sAVC), and inferior (iAVC). (Figure created from data adapted from Snarr et al. 2008.) US PATENT NO: 5,957,949 US Patent No: 5,957,949 – MAY 1997 Percutaneous placement valve stent Abstract An artificial valve stent for maintaining patent one way flow within a biological passage is disclosed. The artificial valve includes a tubular graft having radially compressible annular spring portions for biasing proximal and distal ends of the graft into conforming fixed engagement with the interior surface of a generally tubular passage. Also disclosed is a deployment catheter including an inner catheter having a nitinol core wire, a controllable tip balloon at its the distal end for dilation and occlusion of the passage, and a controllable graft balloon in the vicinity of and proximal to the tip balloon for fixedly seating the spring portions in conformance with the interior surface of the passage. A spool apparatus for adjusting or removing an improperly placed or functioning artificial valve, and a microembolic filter tube are usable with the deployment catheter. The artificial valve may be completely sealed to the living tissue by light activated biocompatible tissue adhesive between the outside of the tubular graft and the living tissue. A method of implanting the artificial valve is also disclosed. Inventors : Leonhardt Howard J. (Sunrise, US), Greenan Trevor (Sunrise, US) Published Assignee : WORLD MEDICAL MANUFACTURING CORP. (Sunrise, US) US PATENT NO: 5,957,949 Leonhardt et al US Patent No: 5,957,949 – MAY 1997 (prototype 1988) Percutaneous placement valve stent 17 claims highlights Light activated foam cuff with tissue adhesive packets. Light heats up and causes foam cuff to grow like a marshmellow in a microwave. Cell in-growth encouraging foam cuff. Removal and repositioning system. Nitinol adaptive conformace sealing stent. CIP multi-stage 8FR delivery – piece by piece. PATENTED MULTI-STAGE DESIGN TO REDUCE ENTRY PROFILE U.S. Patent 6572645 B2 – Priority Feb 1998 Inventor Howard J. Leonhardt Delivery system for development and endovascular assembly of a multi-stage stented graft ABSTRACT A multi-stage stent graft for implantation into a blood vessel is disclosed. Each stage or layer may comprise radially compressible spring stents with or without a fabric covering, or may comprise a foamed tube. The various stages or layers may also have an adhesive coated thereon. The multi-stage stented graft and the adhesive coatings provide a surface for the ingrowth of cells and promote healing. Also disclosed is a coaxial delivery system for the delivery and endovascular assembly of the multi-stage stented graft during one trip into the vasculature. STEP 1 = Decalcify with dental burr on tip of deflecting tip catheter BURRS FOR DEBULKING CALCIFICATION ON CATHETER TIP BULK DECALCIFY WITH BURR FLEXIBLE MICROSCOPE EXPLORES DEEPLY HIDDEN CELLS CELLVIZIO TECHNOLOGY MICROSCOPE ON A CATHETER TIP Step 2 = Ultrasonic cleaning. ULTRASONIC CLEANING DEVICE Step 3 = Deliver regenerative microcurrent to valve via flexible optical fiber. Causes SDF-1 release which recruits stem cells and separate signal differentiates those cells into valve tissue. How does microcurrent energy repair heart valve tissue? … #1 - Causes SDF-1 release from targeted tissue which homes stem cells to damaged tissue. Treats whole valve and surrounding tissues. #2 – Differentiates recruited cells into healthy tissue. #3 – Builds heart valves the way they are built in first place just like embryos. THE FUTURE IS NOW: WIRELESS MICRO CURRENT DIRECTED STEM CELL REGENERATION STRICTLY PRIVATE AND CONFIDENTIAL 26 MICROCURRENT REGENERATIVE SIGNAL DELIVERED TO DISEASED HEART VALVE VIA FLEXIBLE FIBER OPTICS FLEXIBLE FIBER PROBE FOR MICROCURRENT DELIVERY LOW PROFILE MICROCURRENT DELIVERY FOR REGENERATION THE REMODELING OF CARDIOVASCULAR BIOPROSTHESES UNDER INFLUENCE OF STEM CELL HOMING SIGNAL PATHWAYS. Biomaterials. 2010 Jan;31(1):20-8. doi: 10.1016/j.biomaterials.2009.09.016. Epub 2009 Sep 22. De Visscher G1, Lebacq A, Mesure L, Blockx H, Vranken I, Plusquin R, Meuris B, Herregods MC, Van Oosterwyck H, Flameng W. Abstract Optimizing current heart valve replacement strategies by creating living prostheses is a necessity to alleviate complications with current bioprosthetic devices such as calcification and degeneration. Regenerative medicine, mostly in vitro tissue engineering, is the forerunner of this optimization search, yet here we show the functionality of an in vivo alternative making use of 2 homing axes for stem cells. In rats we studied the signaling pathways of stem cells on implanted bioprosthetic tissue (photooxidized bovine pericardium (POP)), by gene and protein expression analysis. We found that SDF-1alpha/CXCR4 and FN/VLA4 homing axes play a role. When we implanted vascular grafts impregnated with SDF-1alpha and/or FN as carotid artery interpositions, primitive cells were attracted from the circulation. Next, bioprosthetic heart valves, constructed from POP impregnated with SDF-1alpha and/or FN, were implanted in pulmonary position. As shown by CD90, CD34 and CD117 immunofluorescent staining they became completely recellularized after 5 months, had a normal function and biomechanical properties and specifically the combination of SDF-1alpha and FN had an optimal valve-cell phenotype. Step 4 – Implant Autologous Cell Valve Mounted in Stent OR cell sod valve OR glue in place Autologous Cell create Valve Leaftets Minimally-Invasive Implantation of Living Tissue Engineered Heart Valves A Comprehensive Approach From Autologous Vascular Cells to Stem Cells Dörthe Schmidt, MD, PhD?,†,‡; Petra E. Dijkman, MSc§; Anita Driessen-Mol, PhD§; Rene Stenger, BSc‡; Christine Mariani, MSc?; Arja Puolakka, MSc?; Marja Rissanen, LicTech?; Thorsten Deichmann, DiplIng¶; Bernhard Odermatt, MD#; Benedikt Weber, MD?,†,‡; Maximilian Y. Emmert, MD?,†,‡; Gregor Zund, MD‡; Frank P.T. Baaijens, PhD§; Simon P. Hoerstrup, MD, PhD?,†,‡ [+] Author Information J Am Coll Cardiol. 2010;56(6):510-520. doi:10.1016/j.jacc.2010.04.024 DATA SUPPORTING STEM CELL REPAIR OF HEART VALVES IS BUILDING Injectable living marrow stromal cellbased autologous tissue engineered heart valves: first experiences with a one-step intervention in primates Benedikt Weber , Jacques Scherman , Maximilian Y. Emmert , Juerg Gruenenfelder , Renier Verbeek , Mona Bracher , Melanie Black , Jeroen Kortsmit , Thomas Franz , Roman Schoenauer , Laura Baumgartner , Chad Brokopp , Irina Agarkova , Petra Wolint , Gregor Zund , Volkmar Falk , Peter Zilla , Simon P. Hoerstrup DOI: http://dx.doi.org/10.1093/eurheartj/ehr059 2830-2840 First published online: 17 March 2011 DATA SUPPORTING STEM CELL REPAIR OF HEART VALVES IS BUILDING Valvular Heart Disease – CIRCULATION From Stem Cells to Viable Autologous Semilunar Heart Valve Fraser W.H. Sutherland, FRCS; Tjorvi E. Perry, MD; Ying Yu, PhD; Megan C. Sherwood, MD; Elena Rabkin, MD, PhD; Yutaka Masuda, MD, PhD; G. Alejandra Garcia, MD; Dawn L. McLellan, MD; George C. Engelmayr Jr, PhD; Michael S. Sacks, PhD; Frederick J. Schoen, MD, PhD; John E. Mayer Jr, MD Regenerative Medicine Approach to Heart Valve Replacement Stephen F. Badylak, DVM, MD, PhD ADIPOSE STEM CELL COLLECTION KIT Produced according to cGMP Each Laboratory Kit includes: • A vial of lyophilized “Adipolase” which consists of a clinical grade collagenase • consumables necessary to isolate regenerative stem cells THE SWISS EXPERIENCE Pre-Clinical Research | August 2012 Stem Cell–Based Transcatheter Aortic Valve Implantation First Experiences in a Pre-Clinical Model Maximilian Y. Emmert, MD?; Benedikt Weber, MD?; Petra Wolint?; Luc Behr, VDM, PhD¶; Sebastien Sammut, PhD?; Thomas Frauenfelder, MD§; Laura Frese, PhD?; Jacques Scherman, MD‡; Chad E. Brokopp, PhD?; Christian Templin, MD?; Jürg Grünenfelder, MD†; Gregor Zünd, MD?; Volkmar Falk, MD‡; Simon P. Hoerstrup, MD, PhD? Swiss Center for Regenerative Medicine, University and University Hospital Zurich, Zurich, Switzerland J Am Coll Cardiol Intv. 2012;5(8):874-883. doi:10.1016/j.jcin.2012.04.010 THE SWISS EXPERIENCE Objectives This study sought to investigate the combination of transcatheter aortic valve implantation and a novel concept of stem cell-based, tissue-engineered heart valves (TEHV) comprising minimally invasive techniques for both cell harvest and valve delivery. Methods Within a 1-step intervention, trileaflet TEHV, generated from biodegradable synthetic scaffolds, were integrated into selfexpanding nitinol stents, seeded with autologous bone marrow mononuclear cells, crimped and transapically delivered into adult sheep (n = 12). Planned follow-up was 4 h (Group A, n = 4), 48 h (Group B, n = 5) or 1 and 2 weeks (Group C, n = 3). TEHV functionality was assessed by fluoroscopy, echocardiography, and computed tomography. Post-mortem analysis was performed using histology, extracellular matrix analysis, and electron microscopy. THE SWISS EXPERIENCE Results Transapical implantation of TEHV was successful in all animals (n = 12). Follow-up was complete in all animals of Group A, three-fifths of Group B, and two-thirds of Group C (1 week, n = 1; 2 weeks, n = 1). Fluoroscopy and echocardiography displayed TEHV functionality demonstrating adequate leaflet mobility and coaptation. TEHV showed intact leaflet structures with well-defined cusps without signs of thrombus formation or structural damage. Histology and extracellular matrix displayed a high cellularity indicative for an early cellular remodeling and in-growth after 2 weeks. Conclusions We demonstrate the principal feasibility of a transcatheter, stem cell–based TEHV implantation into the aortic valve position within a 1-step intervention. Its long-term functionality proven, a stem cell–based TEHV approach may represent a next-generation heart valve concept. BASICS OF STEM CELL DERIVED HEART VALVE PROCEDURE THE SWISS EXPERIENCE THE SWISS EXPERIENCE Stem Cell–Based, TEHV Implantation Into the Aortic Valve Position via a Transcatheter, 1-Step Interventional Approach Bone marrow is aspirated from the sternum into a heparinized syringe (1) and bone marrow mononuclear cells (BMMC) are obtained by centrifuging the samples on a histopaque density gradient (2). The BMMC are seeded onto the stented heart valve scaffolds using fibrin as a cell carrier (3). Thereafter, the tissue-engineered heart valve (TEHV) is loaded into the delivery device by crimping the outer diameter down to 8 mm and transapically delivered (4). The mean duration of the entire procedure, starting from cell harvest until TEHV-implantation takes approximately 2 h. THE SWISS EXPERIENCE THE SWISS EXPERIENCE Explant Macroscopy of TEHV Explanted tissue-engineered heart valves (TEHV) displayed intact leaflet structures with well-defined cusps and sufficient coaptation, without signs of thrombus formation, thickening, shrinking, or structural damage from the lower view (A and inset) and the upper view (B). The TEHV harvested at 1 and 2 weeks after implantation appeared to be well integrated into the surrounding tissue by complete tissue covering of the stent-frame (C). THE SWISS EXPERIENCE THE SWISS EXPERIENCE Histological Analysis of TEHV Explants On histology, acute explants showed clear cellular infiltrates and fibrin formation in hematoxylin and eosin staining (A to D) (magnification 5× and 10×). Interestingly, this cellularity only slightly increased in the tissues of the 24-h explants (images not shown), whereas all later explant stages at 1 week and 2 weeks showed a clearly increased cellularity (E to L) (magnification 5× and 10×). TEHV = tissue-engineered heart valve(s). THE SWISS EXPERIENCE THE SWISS EXPERIENCE Performance of TEHV and Echocardiography Findings Tissue-engineered heart valve (TEHV) functionality and mobility was controlled via epicardial and transesophageal echocardiography. TEHV tolerated the loading pressure of the systemic circulation adequately and demonstrated a sufficient coaptation (A, B, and insets). TEHV functionality and absence of regurgitation was confirmed in the 2-dimensional color mode (C, D, and insets) and in the 3-dimensional mode demonstrating adequate leaflet mobility (E to G, and insets). See Online Videos 2A, 2B, and 2C. AUTOLOGOUS CELLS + SCAFFOLD PRODUCED HEART VALVE TISSUE ENGINEERED VALVE TISSUE ENGINEERED VALVE TISSUE ENGINEERED VALVE DELIVERY VIEW OF EXPLANTED TISSUED ENGINEERED VALVES CELL SODDING AND SUTURING CATHETER COMPARABLE CONCEPT OF HOW TO GLUE A NEW TISSUE ENGINEERED LEAFLET IN PLACE EXAMPLES OF MICROCURRENT HEALING Over 50 studies have been completed documenting the healing ability of microcurrent. The Leonhardt team has received two U.S. patents with many more pending. Major patent claims include specific program to cause any tissue to release stem cell homing signal and control of differentiation. 510KD MICROCURRENT STIMULATORS FOR HEALING STRICTLY PRIVATE AND CONFIDENTIAL 56 THE FUTURE IS NOW: WIRELESS MICRO CURRENT DIRECTED STEM CELL REGENERATION STRICTLY PRIVATE AND CONFIDENTIAL 57 WIRELESS MICROCURRENT HEALING PAPER ON WIRELESS MICRO CURRENT STIMULATION STRICTLY PRIVATE AND CONFIDENTIAL 59 Microcurrent Treatment 95% Reduction of Wound Scar Size @ 8 Weeks 47 Patient Clinical Study – Germany & Switzerland – Published International Wound Journal ISSN 1742-4801 2014 CARDIOBRIDGE CIRCULATORY ASSIST PUMP STRICTLY PRIVATE AND CONFIDENTIAL 61 Procyrion and Cardiobridge ACCESSORY CIRCULATORY ASSIST DEVICES TO RELIEVE HEART WORK LOAD AND IMPROVE PERFUSION IN LIMBS – RECOMMENDED FOR ALL HEART, VALVE AND LIMB REGENERATION PROCEDURES PROCYRION TEMPORARY AORTIC PLACED CIRCULATORY ASSIST STRICTLY PRIVATE AND CONFIDENTIAL 63 ADVANCED ARTERY REPAIR METHOD Athrectomy followed by adventia delivery of autologous endothelial progenitor cells (derived from fat tissue) – EndoCell – for artery repairing. Regrows healthy endothelium lining in vessel. ATHRECTOMY FOLLOWED BY ENDOTHELIUM ADVENTIA RE-LINING WITH INJECTED EPC’S STRICTLY PRIVATE AND CONFIDENTIAL 65