Encouraging Healthy Eating Habits in Preschool Chidren Try to dine
advertisement

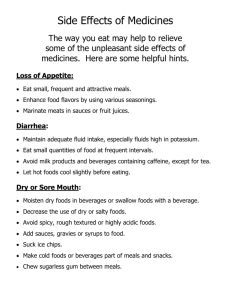
NUTRITION AND IMMUNIZATION OF CHILDREN AND ADULTS 5 A’s for Organizational Construct for Clinical Counseling • Ask about risky health behaviors (lifestyles) and consider factors such as age, gender, ethnicity, presence or absence of co-morbidities, literacy, etc. that would impact the choice of behavioral change goals/methods. • Advise Provide clear, specific, individualized behavior-change advice including personalized information about the risk/benefit of lifestyle change. Advice messages from the physician can be brief (30– 60 seconds), especially if provided in a team care context. 5 A’s for Organizational Construct for Clinical Counseling • Arrange Regularly scheduled follow-up in person or by phone/fax/email offers continual support and allows for adjustment of the treatment plan, as the patient’s condition, interest, and motivation level changes. After initial follow-up, contact is spaced based on intervention outcomes/patient need for reinforcement. Referral to more intensive/specialized treatment may be indicated as co-morbidities develop or environmental/support systems change. 5 A’sFor Organizational Construct for Clinical Counseling • Agree Treatment goals are mutually negotiated and selected based on the patient’s interest in and readiness to change problem behaviors, and after consideration of treatment options, probable outcomes, and patient preference. • Assist The physician, either directly, via office staff or by referral ensures that self-management skills are taught and problem-solving/coping skills development is encouraged to facilitate skills advancement, maintenance, and relapse prevention For patients not ready to commit to a specific behavioral change in the immediate future, assistance in the form of strategies that explore ambivalence can help to move patients along the change continuum. Stages of Change • Precontemplation No intention to change behavior in the foreseeable future • Contemplation Aware that a problem exists and are seriously thinking about overcoming it but have not yet made a commitment to take action • Preparation Intending to take action in the next month • Action Modifying behavior, experiences, or environment in order to overcome their problems • Maintenance Working to prevent relapse and consolidate the gains attained during action. This stage extends from six months to an indeterminate period past the initial action. Encouraging Healthy Eating Habits in Preschool Chidren • Try to dine as a family whenever possible. • Limit TV/computer time to less than 2 hours/day. • Encourage your child to be physically active (children need at least one hour of activity/day). • Offer family activities to promote exercise. Encouraging Healthy Eating Habits in Preschool Chidren • Do not use dessert as a reward ( ‘ finish your vegetables or you won’t have dessert’)-dessert is part of the meal and should be no more desired than the meal itself. • Serve healthy desserts when possible. • When a child says they have finished, allow them to take their plate to the sink and return to the table while parents finish. Appropriate activities or books will allow the child to enjoy this time. • Keep a cabinet full of healthy snacks for the child’s choosing at snack time. Encouraging Healthy Eating Habits in Preschool Chidren • Serve fruits and vegetables every day at meals and snacks. Keep canned fruit such as pineapple, peaches and mandarin oranges in their own juice on hand for quick snacks. • Provide milk (low-fat for children over 2 years) and water for meals or snacks. Limit juice to 100-160 g/ day. • Do not be afraid to say no to junk food, chips, soda, candy or sweets. • Serve small portions on small plates and small cups. Let the child regulate his or her own intake. Serving large portions and insisting on a ‘ clean plate’ can lead to overeating and the loss of self-regulation. • . Energy and Protein Requirements Energy(kcal/day) • • • • • • • Age 0-6 mon 7-12 mon 1-2 yrs 3-8 yrs 9-13 yrs 14-18 yrs Males 570 743 1046 1742 2279 3152 Females 520 676 992 1642 2071 2368 Protein(g/day) Males 9.1 11.0 13 19 34 52 Females 9.1 11.0 13 19 34 46 Recommendations for Weight and Length Gain in Healthy Children Weight • • • • • • Length Age (g/day) (cm/month) 3 months 25-35 2.6-3.5 3-6 months 6-12 months 1-3 years 4-6 years 7-10 years 15-21 10-13 4-10 5-8 5-12 1.6-2.5 1.2-1.7 0.7-1.1 0.5-0.8 0.4-0.6 Effectiveness of Medical Nutrition Therapy Endpoint • • Glycemic control A1C Plasma fasting glucose Lipids T.Cholesterol LDL cholesterol Triglycerides HDL cholesterol Blood pressure Expected outcome 1-2 unit(15-22%) decrease 50-100 mg/dL decrease 24-32 mg/dL(10-16%) When to evaluate 6 weeks to 3 mon. 6 weeks; if goals not achieved,intensify nutrition therapy and evaluate again in 6 weeks 19-25 mg/dL(12-16%) decrease 15-17mg/dL(8%) decrease With no exercise:7% decrease With exercise:No decrease 5mmHg decrease in systolic and 2mmHg decrease in diastolic Measure at every visit (in hypertensive patients) Guidelines for Avoiding Hypoglycemic Symptoms 1.Eat small meals, with snacks between meals and at bedtime. 2.Spread the intake of carbohydrate foods throughout the day. Carbohydrate foods include starches,fruits and fruit juices,milk and yogurt, and foods containing sugars. 3. Avoid foods that contain large amounts of carbohydrate. 4.Avoid foods and beverages containing caffeine. Guidelines for Avoiding Hypoglycemic Symptoms • 5. Limit or avoid alcoholic beverages. If an individual chooses to drink alcohol, it should be in moderation and food should always be eaten along with the alcoholic beverage • 6.Decrease fat intake. Decreasing fat intake also helps to weight loss.Excess weight interferes with the body’s ability to use insuline. Medical Nutrition Therapy for GERD • Limit intake of high fat, high calorie meals. • Eat smaller meals more frequently during the day. • Drink most fluids between meals rather than with meals. • Increase intake of high fiber foods, such as fruits and vegetables,and whole grains. Medical Nutrition Therapy for GERD • Sit up or take a walk after eating. Lying down after a meal can worsen symptoms. • Limit foods that worsen symptoms, such as alcohol, chocolate, coffee, or caffeinecontaining beverages, mint, citrus fruits, tomato products, spicy foods, or carbonated beverages. Medical Nutrition Therapy for Peptic Ulcer Disease • Limit intake of caffeine containing beverages and foods including coffee like tea, iced teas, colas, and chocolate. • Avoid alcohol, especially on empty stomach. • Eat three small meals per day. Medical Nutrition Therapy for Peptic Ulcer Disease • Don’t skip meals. • Avoid eating spicy foods, fried foods, and citrus fruits as these foods may worsen symotoms • Avoid other foods or drinks that cause discomfort. Tips to Decrease Gas and Bloating • Certain foods can produce excess gas during digestion. Various foods effect people in different ways. The following diet tips may improve symptoms. • Foods that may cause gas: • Beans, cabbage, cauliflower, brussel sprouts, broccoli, asparagus, peppers, cucumbers, onions, garlic, radishes, sauerkraut • Raw apples, avocado, melon • Eggs, fried and fatty foods, carbonated beverages • Swallowing air may also cause excess gas: • Eat slowly, avoid chewing gum, carbonated beverages,and smoking. Nutritional Recommendations for UTI • 1) Maintain adequate fluid intake of 8 cups of water, juice, milk, or other beverages. Tea and coffee can be considered part of fluide intake. • 2) Recommend two water glasses of cranberry juice every day; 10-12 hours apart for UTI-susceptible individuals. • 3) Increase intake of dairy products such as yogurt. • 4) Improve overall quality of food intake by increasing fruits, vegetables, whole grains, fish, poultry, olive or canola oil, and nuts. Dietary Counseling Issues by Age and Diseases • • • • • • • • • • • Infants Flouride,iron,calories for growth,development Children Flouride,iron,Ca,calories for growth,development Teenagers Iron,Ca,calories for pubertal devolopment Pregnancy Folate,iron,Ca.appropriate weigth gain Alcoholism Folate,thiamin,vit.B12,calories Anemia Iron,vit.B12,folate Ascites Sodium,protein,fluid Beriberi Thiamin Cancer Adequate calories and protein,vit.,minerals,fiber COPD Vit.D,Ca,weight loss,calories Diabetes Carbohydrates,sat.fat,cholesterol,calories,fiber Dietary Counseling Issues by Age and Disease • • • • • • • Hyperlipidemia Hypertension Kidney stone Liver disease Malabsorption Obesity Osteoporosis Sat.fat,monounsat.fat,choles.,folate,fiber Na,Ca,K,alcohol,total calories Ca,oxalate,uric acid,protein,Na,fluid Protein,Na,fluid Vitamins A,D,E,K,fat Total calories,saturated fat Vitamin D and calcium Dietary Counseling Issues by Age and Disease • • • • • Pellegra Renal failure Rickets Scurvy Vegetarian Niacin Protein,Na,K,phosphorus,fluid Vitamin D,calcium Vitamin C Protein,Vitamin B12,iron,calcium Key Diet History Questions for Brief Intervention • Questions for all patients • How many meals and snacks do you eat everyday? • How often do you eat out? What kind of restaurants? • What do you like to drink during the day, including alcohol? How many glasses? How often do you eat fruits and vegetables? • How often do you eat dairy products? Low fat or regular type? • Do you usually finish what is on your plate or leave food? • How often do you exercise, including walking? Key Diet History Questions for Brief Intervention • In addition to the questions above • Questions for patients with dislipidemia • How often do you eat fatty meats? (hot dogs, sausage, salami, pastrami) • How often do you eat fish? How is it prepared? • What do you spread on your bread? • What types of fats do you use in cooking? • What types of snacks and desserts do you eat ? Key Diet History Questions for Brief Intervention • Questions for patients with high blood pressure • Do you use a salt shaker at the table or in cooking? • Do you read food labels for sodium content? (<400 mg/serving permitted) • How often do you eat canned, smoked, frozen and prepared foods? Key Diet History Questions for Brief Intervention • Questions for patients with diabetes mellitus • What time do you take your diabetes medication (including insulin)? • What time do you eat your meals and snacks? • Do you ever skip meals during the day? • How many servings of starchy foods such as breads, careals, pastas, corn, peas, or beans do you eat during a typical day? Dietary Triggers for Migraine Headaches • Offending food or behavior Chemical trigger • Cheese Tyramine • Chocolate Phenylethyamine, theobromine • Citrus fruits Phenolic amines, octopamine • Hot dogs,cured meats Nitrites,nitric oxide • Dairy foods Allergenic proteins(casein) Dietary Triggers for Migraine Headaches • • • • • • • • Offending food or behavior Fatty and fried foods Food dyes,additives Artificial sweetener Wine,beer Caffeineated beverages Fasting,skipping meals Inadequate sleep Chemical trigger Linoleic and oleic fatty acids Tartrazine,sulfites Aspartame Histamine,tyramine,sulfites Caffeine withdrawal Hypoglycemia,stress hormone release Treatment Protocols by Body Mass Index • BMI • • • • • 25-30 27-30 RF 30-40 35-40 RF ≥ 40 Diet Exercise Behavior Pharm Surgery x x x x x x x x x x x x x x x x x x x x x Sources of Dietary Fat 1. More atherogenic: Saturated fatty acids a) Beef, Pork, Veal,Lamb, b) Hydrogenated vegetable oils c) Cocoabutter, coconut oil, palm oil Sources of Dietary Fat • 2.Less atherogenic: Unsaturated fatty acids • A) Polyunsaturated fatty acids • a) omega-6 fatty acids: corn,safflower, sunflower, soybean • b) omega-3 fatty acids: fish, flaxseed, soybean, marine vegetation • B) Monounsaturated fatty acids: olive-oil, canola oil, nuts, avocado Immunization In Childhood Birth Hep B I 1st month 2nd moth 4th month II 6th month 18-24 month 1st class III BCG I DaBTIPA-Hib I II III MMR Rapel I Polio Pneum ococcal 12 th month I I II III I Rapel I Immunization in Childhood • DaBT-IPA-Hib : Diphteria,tetanus,pertussis,inactivated polio,Haemophilus influenza type B • MMR :Measles, mumps, rubella Immunization in Aduts • Age 19-26 27-49 50-59 60-64 ≥65 Influenza __________________ every year(1) Tatanus,diphteria, Pertussis __________________ every 10 years(1) Varicella ___2 dose(1) HPV __3 dose (women)(1) Zoster __________________________________________1 dose(1) MMR ________ 1 or 2 dose(1)_______________1 dose(2) Pneumococcal__ 1 or 2 dose(2)___________________________________1 dose(1) Hepatitis A_____ 2 dose(2) Hepatitis B_____ 3 dose(2) Meningococcus_ 1 or more(2) Immunization in Aduts • 1. All individuals in this age group who are not immunized • 2. Individuals with risk factors ( medical, occupational)