Interdisciplinary Approaches to Addressing At
advertisement

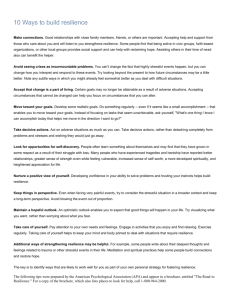
Interdisciplinary Approaches to Addressing At-Risk Behaviors in the Post-Acute Rehabilitation Setting Amy Gonshak, Ph.D. Introductions Amy Gonshak, Ph.D. Kentucky One Health Frazier Rehabilitation Institute NeuroRehab Program 4912 US Highway 42 Suite 104 Louisville, KY 40222 Phone: (502) 429-8640 Introductions - Frazier NeuroRehab Program description • Intensive outpatient (2 or 3 days a week, 8:45am-3:15pm, seven 45min individual & group treatment sessions) • ST, OT, PT, and psychology • Access to KY Voc Rehab and vision therapy onsite • Physician referral and follow-up (communication!) • Full-time case management (communication!) • 4 out of 5 days include staff team conferences (communication!) • Patient, family, and team conferences as needed (communication!) • 35-40 program patients on 6 staff teams plus 30 single discipline outpatients • Binders, Bands & Belts Introductions - Who’s in the audience? Survivors? Family members? Treatment Providers? Introductions - Patients (and Families) who have experienced Brain Injury Aquired Brain Injury (ABI) • Injury to the brain that occurred after birth and is not hereditary, congenital, or degenerative • Causes: Tumor, Stroke, Seizure, Toxic Exposure, Infections, Metabolic Disorders, Anoxia/Hypoxia, TBI • Includes injuries caused by external assault (TBIs) and by internal assault Traumatic Brain Injury (TBI) • Injury to the brain caused by an external physical force • Causes: Falls, Motor Vehicle Accidents, Assaults, Gun Shot Wounds, Sports Injuries, Work Injuries, Child Abuse, Domestic Violence, Military Actions Impairments can be either temporary or permanent and cause partial or total functional disability Our Patients • ABI may result in mild, moderate, or severe impairments in one or more areas including: • PHYSICAL: ambulation, balance, coordination, strength, endurance, sensation, vision, hearing, tasting, smelling • COGNITIVE: communication, attention, memory, reasoning, problem-solving, judgment, organization, processing speed • PSYCHOSOCIAL: emotional awareness and expression (arousal management), social skills, adjustment, self-identity Psychological Challenges • Emotional blunting, disengagement • Emotional dysregulation • Impaired interpersonal skills • Impaired sensory-perceptual functioning, sensitivity to light, sound, stimulation • Impaired motivation, initiation, and follow-through • Loss of major roles (family and work) Psychological Challenges (continued) • Sadness/depression, irritability/anger • Fear, anxiety, panic attacks • PTSD symptoms • Grief • Pain • Wounded sense of self: Uncertainty, loss of agency, loss of confidence and efficacy, shame, embarrassment, self-consciousness • Comprehension, acceptance, and integration of sudden unwanted loss and change What are the “At-Risk” Behaviors we might expect and want to prevent? Let’s Name Them… Without treatment, individuals with problematic or unmanageable behaviors are the most likely to become homeless, institutionalized in a mental facility, or imprisoned. -AACBIS At-Risk Behaviors that impact Treatment & Community Reintegration • Physical Safety Issues • Substance Use or Abuse • Medication and Treatment Non-compliance • Inappropriate interpersonal interactions (aggression, sexual) • Return to driving or work too soon CHARACTERISTICS of the *TEAM* • Knowledge of medical condition/neuroanatomy • Patience • Creativity • Mental flexibility • Holistically minded • Hopeful & Inspiring • Compassionate •“Trauma-Informed” • Tolerance and acceptance of ambiguity and frustration • Team player • Blend of patientcentered and directive • Realistic • Self-aware • Strong executive skills FOUNDATIONAL PRINCIPLES *COLLABORATION* *STRUCTURE* *ACCOUNTABILITY* *HOPE* “To live without hope is to cease to live.” – Fyodor Dostoevsky SO NOW WHAT? What Are Foundational Goals? WITH EVERY PATIENT and FAMILY… ************************************** *** • Build Resilience • Educate about Brain Injury and Recovery • Increase Self-Awareness & Self-Monitoring • Promote Wellness Behaviors • Provide Support and Validation ************************************** *** Helping to Build Resilience •Resilience is the process of adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress — “Bouncing Back” •Road to resilience is likely to involve considerable emotional distress. •Resilience can be learned and developed. Building Resilience Several factors are associated with resilience Ability to see your strengths Skills in communication and problem solving Capacity to manage strong feelings and impulses Capacity to make realistic plans and take steps to carry them out Family and social support GRATITUDE Specific Strategies for a “Healing Brain” • Brain Injury Education (Validate & Normalize) • Review medical records with patient and family • Review Neuropsychological Testing • Groups • Arousal Management • Breathing exercises (app-Breathe2Relax; drweil.com) • Mindfulness/Meditation • Progressive Muscle Relaxation • Expressive Therapy techniques • Motivational Interviewing Trauma-Informed Care & Motivational Interviewing Collaboration: Confrontation: • Partnership that honors the client’s expertise and perspectives. Therapist provides an atmosphere that is conducive rather than coercive to change. • Counseling overrides client’s impaired perspectives by imposing awareness and acceptance of “reality” that the client cannot see or will not admit. Evocation: • Resources and motivation for change are presumed to reside within the client. Intrinsic motivation for change is enhanced by drawing on client’s perceptions, goals and values. Autonomy: • Therapist affirms client’s right and capacity for self-direction and facilitates informed choice. Education (About How to Change): • Client is presumed to lack key knowledge, insight, and/or skills necessary for change. Therapists attempts to address these deficits by providing requisite enlightenment. Authority: • Therapist tells the client what he or she must do. Additional Strategies • Structure and Expectations • Note Taking (use of binder) • “Advisory Board” or “outside brain(s)” • Timing and Pacing of feedback • User-friendly language • Mantras (on note cards) • Diagrams, drawings • Complementary media (youtube videos, music, art, books, apps) TEAMWORK!!! Areas of Significant Overlap with team (ST, OT, PT) • Cognition: attention, memory, problem solving, decision making, organization, path finding, goal setting • Social communication • Medication management • Pain management • Frustration tolerance • Anxiety/ “internal distraction” • Pragmatic, constructive coping • Orientation x4, time management, safety • Belts, bands, binders & bathrooms PSYCHOLOGISTS’ UNIQUE VALUE TO PATIENTS, FAMILIES & TEAM More Psychology Specific • Provide less structured environment for emotional processing and support • Mood monitoring and management • Grief and loss • Depression, Anxiety, Frustration tolerance/anger • Pain management • Psychotropic med recommendations Psychology specific (cont.) • Health behaviors (nutrition, sleep, hydration, exercise) • Smoking cessation • Alcohol & drug use • Risk reduction/ avoidance • Meaning making/ sense of self • Coach self-advocacy, assertiveness • Family relationship dynamics – caregiver fatigue, role changes For Patients with Co-Morbid Diagnoses Substance Abuse, ADHD or other pre-existing learning disabilities, behavioral and mood disorders, personality disorders, conscious exaggerating of symptoms (malingering) • Make and enforce clear treatment rules (Axis II) • Modify Treatment Environment/Conditions that provoke behavior (aggression) • Monitor and Communicate about Patient’s disposition • Co-Treat • Adjunct Psychopharmacological Interventions • Protocols for Treating Patients at Risk for Self-Harm and Substance Abuse Role of Family Brain Injury of a family member challenges the core values and resources of the family system • Very similar emotional challenges as Patient • Balance Education with Support • Risks for Dysfunction • Pre-morbid history of family problems • Persistent and severe impairments of the BI patient • Extended denial period • Lack of basic supports • Strengths – Ability to listen, communicate, negotiate – Willingness to learn, grow, change – Ability to assist BI family member/ Availability – Spirituality – Present-focused – Self-care *Self Care* for Family & Treatment Provider • “Place the Oxygen Mask on Yourself First” – Role Model • *NURTURE yourself*: Sleep, Nutrition, Alone Time, Friendships, Intimacy, Exercise, Leisure Activity, Mental Vacations, REAL Vacations • Limit caseload of patients with severe comorbid Dx • Use Co-Treatment as needed for complex cases • Acknowledge Inability to “cure” every patient • “Pick Your Battles” • Focus on Process vs. Outcome • Self-Reflect, Utilize Supervision/Mentorship, Personal Therapy • Ask for what you need ABI Websites Model Systems Knowledge Transition Center http://www.msktc.org/tbi TBI Model Systems Data and Statistical Center https://www.tbindsc.org/ Brain Injury Association of America http://www.biausa.org/ Brain Injury Alliance of Kentucky http://www.biak.us/ ABI Websites Mayo Clinic – stroke http://www.mayoclinic.org/diseasesconditions/stroke/basics/definition/con-20042884 MedLine Plus (has Spanish printables) http://www.nlm.nih.gov/medlineplus/stroke.html National Stroke Association http://www.stroke.org/ American Stroke Association http://www.strokeassociation.org/ Thank You!