clinical care gap
advertisement

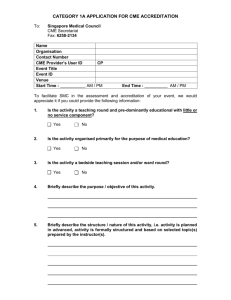
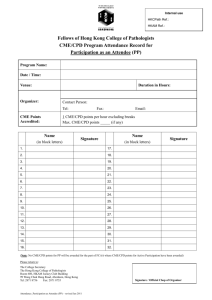
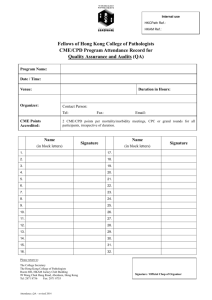
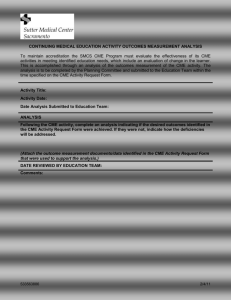
Changing Health Care Provider Performance: the role of effective CME & CPD National Coalition for HP Education in Genetics, September 2011 Dave Davis, MD Senior Director, Continuing Education and Improvement Association of American Medical Colleges An outline: many questions, little time… 1. What are CME and CPD? Why are they ‘invisible’? 2. The ‘Does CME Work?’ question: the in- vitro perspective 3. Does CME work in the real world? - a look at the in-vivo, clinical care gap and its relationship to the world of genetics education 4. So What? Recommendations to a thoughtful genetics audience: guidelines for the use of CME & CPD Question #1 Some definitions: • What do we mean by CME & CPD? • ….by the terms diffusion, implementation? • ….how have we changed in our thinking? • Later….what is knowledge translation/implementation science? What do we mean by ‘CPD and CME’? • educational materials • formal CME: lectures, small groups, courses • outreach visits • opinion leaders • patient-mediated strategies • audit/feedback • reminders (paper, computerized, interactive, etc) • comprehensive, QI- or practice-based interventions • web-based tools, PDAs (borrowed from EPOC, Cochrane Collaboraitve) How have we changed…? Pedagogy (1940’s-50’s) Andragogy (1960-80s) Informed Self-assessment Competency-based education (2000-) What do we mean by…? Diffusion: distribution of information and the practitioners’ natural unaided adoption of policies and practices Dissemination: communication of information to clinicians to improve their skills Implementation: putting a guideline in place, involves effective communication, overcomes barriers by administrative and educational techniques (after Lomas)... Question # 2 “Does CME (CPD) Work?” The In Vitro Question (The Sackett question) Database of Physician Education & Change: www.rdrb.utoronto.ca The Research and Development Resource Base - educational, clinical & health services literature • supported by the American medical Association, the North American CME organizations, Royal College of Physicians and Surgeons of Canada, the University of Toronto and the Association of American colleges Now ~25,000 studies • 12 metropolitan areas, roughly 30 conditions studied, >6,000 patient records examined • Substandard care noted in 45% of clinical areas (of this, 46% underuse; 11% overuse) • Little variation by region or by type of condition (chronic, acute), socioeconomic status • Notable gaps in care in depression, alcohol abuse, diabetes care (about 45%), pneumonia (39%); • Better care (>50% compliance with recommendations) noted in hypertension, cardiac care, but just •NOTE: the inviible care gap (undiagnosed, undetected – e.g., smoking cessation, obesity counseling, care gap is HUGE) www.rdrb.utoronto.ca www.rdrb.utoronto.ca 1) About educational interventions Changing Physician Performance - a systematic review of the effect of CME strategies JAMA 1995;274:700-705 + The effect of formal CME conferences, symposia, rounds, meetings, lectures Effective Not so Effective • *Interactive Lecturing Didactic Teaching • *Sequenced Sessions One-time only • Accurate needs sessions assessment • Successful education has three elements – predisposing, enabling, reinforcing Other findings… Needs Assessment appear to be important – the more the better (subjective needs, objective, gaps and barrier analysis) No evidence yet about long-term effects (well, some) Group size: no demonstrated effect Effective CME may follow Green’s PROCEED model - predisposing, enabling and reinforcing strategies Knowledge necessary but not sufficient for change Quantitative methodology necessary but not sufficient to understand change NEW Multiple methods’ effect uncertain; print materials (simple messages) may not be so bad after all; consider the message; and consider the setting 2) and about the learner-clinician • age • motivation • (dis)incentives • experience • time • environment • training • • • • Emphasis on knowledge Inability to detect needs, evaluate performance ?self-directed learning ?critical appraisal The Pathman Model • awareness: of a guideline, practice innovation, change • agreement: with the innovation or guideline • adoption: ‘trying out’ the new practice, irregularly • adherence: abiding by the new practice on all appropriate occasions Pathman, 1996 The selfassessment question Davis & co., JAMA 2006;296:1096-1102 Of 20 comparisons….. 13 demonstrated little, no or an inverse relationship between self and external assessment: • Examples: learning needs, EBM skills, simulated knee injections • Note: inverse relationships between confidence noted by Leopold (knee injections), Fox (OSCE misperception) and Parker (knowledge-based FP exam) 7 demonstrated a positive relationship: • Examples: cultural-linguistic competencies, global performance with dementia patients, comfort with psycho-social issues in family medicine Just in case we miss the point: of 20 comparisons of selfassessments with external assessments 3) About aligning the learner and educator: the Pathman-PROCEED model stages Methods/ Stages Predisposing Enabling Reinforcing Awareness Agreement Adoption Adherence 3) About the cumulative effect of CCME/CPD Question # 3: Does CME/CPD work in the real world? In the world of effectiveness? Why or why not? The In Vivo Questions The Clinical Care Gap • Overuse • Underuse • Misuse Chassin, 1998 The clinical care gap Ideal, evidence-based practice clinical care gap clinical care gap Current practice What causes the gap? The evidence-to-practice puzzle No time… No, Thursday’s out. How about never-is never good for you? “Information management is like having your mouth to a firehose” David Naylor, President, University of Toronto What causes the gap? the educational delivery System and knowledge translation/ implementation science An emerging field; one concept, two terms “Knowledge translation is the effective and timely incorporation of evidence-based information into the practices of health professionals in such a way as to effect optimal health care outcomes and maximize the potential of the health system” – Adapted from the Canadian Institutes for Health Research definition, 2001 Implementation Science is the scientific study of methods to promote the systematic uptake of research findings and other evidence based practice into routine practice thus to improve the quality and effectiveness of health care and services. ..adapted from the NIH, USA Question #4: How do CME and CPD play a role in genetics & genetics education ? The guideline process: evidence-toaction ‘Consideration of clinician learning style, needs The goal: effective implementation Effective CME/PD How an we use CME/CPD in evidence/message/guideline development in genetics? Recommendation #1: Guideline Development/adaptation Consider CME/CPD in any evidence development process: from learner and educational perspectives (for example, guard against knowledge overload, consider already-held knowledge) a. secure buy-in; involve the end-user in guideline development/adaptation b. employ adult learning principles in guideline statements (format, spacing, language) c. consider recommending effective educational strategies in the guideline itself ….educational issues to consider within the guideline, evidence itself • compatibility • complexity • cost • relative advantage • accessibility • format • patency of evidence, process of development • opportunity; trial-ability One attempt to fix the Message: The Guidelines Advisory Committee, Ontario (now the Center for Evidence-based practice) • Joint body of the Ontario Medical Association and the Ministry of Health and Long term Care, Ontario • Chooses a topic area; reviews all guidelines in that area; scores them by the Cluzeau/AGREE instrument • Mounted them on a website – – – – – Quick, 30 second synopsis Clear language Appropriate format Parallel patient synopsis The apple-score How an we use CME/CPD in genetics education ? Recommendation # 2: Include CME/CPD in any guideline implementation strategy a) Consider the learner - mode of current learning - stage of awareness-adherence at which clinicianlearners exist b) Consider effective educational strategies The CPG implementation toolkit Formal CME Lectures, workshops, small groups Informal education Audit/Feedback Reminders Policy, CQI administrative techniques Print Patient Strategies Multiple Strategies M&M conferences Quality-based rounds Journal Club Team training Handover/off rounds How can we use CME/CPD in genetics education? Recommendation # 3: Consider CME/CPD in a staged fashion, depending on stage of adoption of information, by individuals, groups; use appropriate educational strategies Example #1: a new guideline describes the use of a new disease screening test….. Methods/Stages Predisposing Enabling Reinforcing Awareness Print material, Lectures, Conferences Academic detailing, Media Agreement Adoption Adherence Interactive sequential sessions Small groups, opinion leaders Pt. education, workshops, opinion leaders Reminders, audit/feedback Reminders, audit/feedback Example #2: many primary care providers fail to use a simple genogram when taking patient history Methods/Stages Awareness Agreement Print material, Reinforcing Adherence Patient education and advocacy Predisposing Enabling Adoption Small groups, opinion leaders Pt. education, workshops, flow charts Reminders, audit/feedback Reminders, audit/feedback Example #3: a national campaign: a project of the Association of American Medical Colleges • Launch, June 2011 www.aamc.org/bestpractices • Tools, resources, and support for AAMC members • Collaborative learning sessions • National Faculty Development Initiative • Roughly 250 med schools & teaching hospitals participating Participating medical schools and teaching hospitals have committed to: • Teach quality and patient safety to the next generation of doctors • Ensure safer surgery through use of surgical checklists • Reduce infections from central lines using proven protocols • Reduce hospital readmissions for high-risk patients • Research, evaluate, and share new and improved practices. This list of commitments will grow over time. The Pathman-PROCEED model applied to AAMC’s BPBC campaign Methods/Stages Awareness Predisposing Emails, Conferences, Media Enabling Reinforcing Agreement Adoption Adherence Group work at meetings, conference calls Learning collaboratives, workshops, Web-tools, webinars Reminders, audit/feedback, Awards Reminders, audit/feedback And a few final last words • Large and growing body of evidence about the effect of CME/CPD now imbedded in models of change- no longer an invisible (and ineffective) intervention • Huge clinical care gap, no less so in genetics • Considerable support for consideration of CME/CPD practices and principles – based on best evidence. Dave’s contact info: ddavis@aamc.org www.aamc.org/initiatives/CME/ae4Q www.rdrb.utoronto.ca