Track1_09_Day1_Bromm_Stark
advertisement

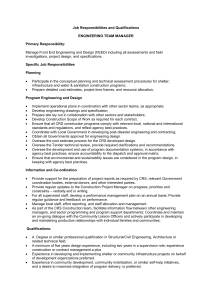
From Vision to Action: Empowering Local Partners to Deliver Sustainable Care Michele Broemmelsiek and Ruth Stark Track 1.0 Implementers Meeting Dar Es Salaam, Tanzania August 4th – 6th 2009 Key Messages Faith-Based Health Care is critical to Africa. There is significant value added in including FBO health networks in national health planning. Successful transition must consider at least the site management and technical aspects. South Africa transitioned successfully because the program was built on strong relationships and planned to transition from Day 1. FBOs and Health Services in Africa 30-70% of health infrastructure in Africa is owned by FBOs (WHO, 2006). Lesotho: 40% of health services Zambia: 30% of health services Kenya: 40% of health services Uganda: 43% of health services Where Do We Work? 34 6 19 3 242 Local Partner Treatment Facilities (Clinic)+ >151 satellite sites 28 16 95 19 22 Slide 4 FBO Role in Transition Overall, 242 sites, 27% public and 73% nonpublic (FBO and Private). The proportion between public and non-public sites differs by country from 100% FBO to 50% FBO. Consultative process to identify the local partners who can support sites Recognize treatment site ownership and ensure that transition strengthens their management and stewardship Vision for Transition Strengthen the capacity in treatment sites for a high quality care delivery system Promote local ownership and good stewardship of program for sustainability Leverage existing structures and develop referrals for effective program integration Ensure long term access to services for patients Ensure long term viral suppression for patients Guiding Principles to Transitioning Retain local human resource capacity (clinical, technical and managerial) Strengthen health systems Focus on best practices Link to existing national institutions and government structures Align transition process to timeline and specific benchmarks Expected Outcomes from Transition Sustained access to quality care with durable patient outcomes Continued support to and scale-up of local organization’s ART programs Local partners have the capacity to: Become a competitive prime for USG funding Manage all functions of Track 1.0 project Reach a sustainable level of operations COMPREHENSIVE HIV CARE Critical Capacities for Sustainable Transition Technical Capacities –Ambulatory HIV Care, Nursing Quality Improvement, Lab, MCH -M&E and coordination of SI, HMIS and DDIU TA Organizational Capacities –Grant Management -Community Linkages -Supply Chain and Pharmacy -Finance and Compliance (USG) Partners: National District Treatment Site Funding Capacities -Cost Management -Resource Mobilization -Communications Policy Capacities -Program Evaluation and Organizational Learning -Networking and Policy Input Key Program Components for Transition Program Management Finance and compliance Human Resources Site and community management Technical Assistance Support Strategic information Clinical mentoring and quality assurance Laboratory services strengthening Supply chain management Identification of Local Partners Identification of local partners that are part of the faith based health network: Sustainable institutions Stewards of quality health care Potential for sustainable level of operations Current or potential Prime USG partner National umbrella and/or a few sites Identification of local partners for local government sites Determined with MOH for specific sites Identification of Local Technical Orgs Sustainable institutions Potential for sustainable level of operations Sub grantees to, or MOU with, local partner for medical/technical assistance to sites Current or potential USG partner Proven technical expertise MOH, university medical schools, specialized technical institutes and other local technical organizations Models for Site Management Transition Model 1: Local partners (local umbrella org.) with sub-grantees providing TA Model 2: Local partners (local umbrella org.) in collaboration with national technical partner/s for clinical and SI (MOH/university/other) Model 3: Sites as direct primes to CDC A combination of these models Models for Transitioning SI Model 1: Local Partner Manages all Strategic Information responsibilities. Model 2: Local Partner manages monitoring and reporting (TA & training) to sites and subcontracts Futures Group for more rigorous data analysis, data demand and information use TA and feedback. Model 3: Local Partner subcontracts all monitoring and evaluation activities to Futures Group.. With all models, Futures Group will continue collaborations with national M&E and HMIS partners. Model for Technical Transition Specific to each country, but based on building partnerships with institutions that can take on different technical roles over the long term with or without long term support: Medical education institutions Ministries of Health National Labs Institutions Network of Sites/LPTFs Successful Transition Example Transition to Local Partners South Africa Transition in South Africa In South Africa, CRS worked through two Indigenous Umbrella Partners: Institute for Youth Development SA (IYDSA) with 5 ART sites in the Eastern Cape Province Southern African Catholic Bishops Conference (SACBC) AIDS Office with 20 ART sites in 7 of the 9 provinces The Transition In June 2009, 2009 IYDSA and SACBC transitioned to local leadership and now receive funds directly from CDC. St. Mary’s Hospital (previously working under the SACBC), now functions independently and receives funds directly from CDC. SACBC has a service agreement with CRS to support M&E, training, clinical coordination, and some aspects of financial management. Funding flow Pre-Transition HRSA/CDC CRS/HQ CMMB IHV CAF IMA CF CDC/SA CRS/SA IYD-SA SACBC ART site ART site St. Mary’s ART site ART site Post-Transition HRSA/CDC CRS/HQ CMMB IHV CAF IMA CF CDC/SA SACBC CRS/SA ART site IYD-SA ART site St. Mary’s ART site ART site Preparation for Transition Began preparation for transition on Day 1. Established relationships with local government. Identified local vendors for outsourcing pharmacy and laboratory services. Utilized local clinical experts for training, mentoring and evaluation. Facilitated direct relationships between local partners and donors. The Process of Transition Working as a Team Built on long established partnership relationship. Learned together and jointly planned and implemented the program. Assigned roles and responsibilities on basis of skills, NOT organizational identity. Local partners gained experience in managing USG-funded projects and applied directly for support Today local partners lead the team as the prime, with a service agreement with CRS for continued technical support. Transition Lessons Learned Respect local capacity Begin early Learn together Approach donors jointly Utilize local resources Work with the host government Build an effective team Work side by side Disengage gradually Challenges for Transition Flat-lined budget which means in fact reduced funding for transition, due to increasing numbers of patients on treatment. Technical transition requires a unique design per country, as there is not one model for medical or strategic information transition. Effective Health Systems Strengthening for sustainable transition will extend far beyond the transition period. Opportunities through Transition Strengthen local organizations to lead health advocacy at a national level and to access resources from multiple donors Improve health status in Africa by strengthening health systems to provide quality services (MDGs) Improve the linkages between the Government and Non-Governmental structures providing health services Slide 26 Thank You