Smith Mission Lifeline

Rural Nebraska
Julie Smith, RN BSN MHA
Director Mission: Lifeline Nebraska
©2013, American Heart Association 1
WELCOME
2014 NeRHA Conference
Mission: Lifeline
Nebraska STEMI INITIATIVE
4/16/2020 ©2013, American Heart Association 2
OBJECTIVES
1.
Mission: Lifeline
2.
STEMI System of care in Nebraska
3.
Grant funding opportunities for local EMS and Critical Access
Hospitals.
4.
Education
4/16/2020 3
AHA NE MISSION: LIFELINE Support
Julie Smith , RN BSN MHA
Director Mission: Lifeline Nebraska
American Heart Association, Midwest Affiliate
Mobile: (308) 695-6312
Julie.Smith@heart.org
Gary W. Myers, MS
Director Mission: Lifeline South Dakota
EMS Consultant for Midwest Affiliate
American Heart Association, Midwest Affiliate
Mobile: (605) 215-1551
Gary.Myers@heart.org
Kay Brown CSSBB
Director of Quality & Systems Improvement KC, Kansas and Nebraska
American Heart Association, Midwest Affiliate
Mobile: (913) 652-1916
Kay.Brown@heart.org
4/16/2020 ©2013, American Heart Association 4
AHA NE MISSION: LIFELINE Support
Brian Krannawitter
Government Relations Director
American Heart Association, Midwest Affiliate
Office: (952)278-7921
Brian.Krannawitter@heart.org
Kristin Waters
Communications Director
American Heart Association, Midwest Affiliate
Office: (402) 346-0771
Kristin.Waters@heart.org
4/16/2020
Ngia Mua
Project Specialist
American Heart Association, Midwest Affiliate
Office: 952-278-7934
Ngia.Mua@heart.org
©2013, American Heart Association 5
What is Mission: Lifeline?
Mission: Lifeline is the American Heart Association’s national initiative to advance the systems of care for patients with ST-segment elevation myocardial infarction (STEMI) and Out of Hospital Cardiac
Arrest. The overarching goal of the initiative is to reduce mortality and morbidity for STEMI and OOHCA patients to and improve their overall quality of care
4/16/2020 ©2013, American Heart Association 6
What is Mission: Lifeline?
• Mission: Lifeline will:
– Promote ideal STEMI systems of care
– Help STEMI patients get the life-saving care they need in time
–
Bring together healthcare resources into an efficient, synergistic system
–
Improve overall quality of care
• The initiative is unique in that it:
– Addresses the continuum of care for STEMI patients
–
Preserves a role for the local STEMI-referring hospital
–
Understands the issues specific to rural communities
–
Promotes different solutions/protocols for rural vs. urban/suburban areas
– Recognizes there is no “one-size-fits-all” solution
–
Knows the issues of implementing national recommendations on a community level
Improving the System of Care for STEMI Patients
7
•
•
•
How is STEMI Defined?
ST elevation at the J point in at least 2 contiguous leads of ≥
2 mm (0.2 mV) in men or ≥ 1.5 mm (0.15 mV) in women in leads V2 –V3, and/or of ≥ 1 mm (0.1 mV) in other contiguous chest leads or the limb leads.
New or presumably new LBBB at presentation occurs infrequently, may interfere with ST-elevation analysis, and should not be considered diagnostic of acute myocardial infarction (MI) in isolation. If doubt persists, immediate referral for invasive angiography may be necessary.
ECG demonstrates evidence of ST depression suspect of a
Posterior MI
8
What is a Mission: Lifeline
STEMI System?
At Least one
Receiving Center
At Least One EMS
Agency
At Least One referring
Center
…working together to decrease time to reperfusion and to reduce death and disability by improving patient outcomes.
9
Mission: Lifeline – A System of Care
Improving the System of Care for STEMI Patients
10
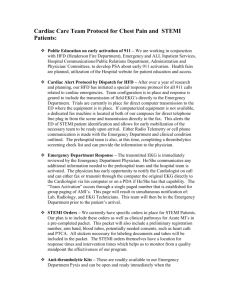
A System of Care – The Roles
The Patient and Family :
• Recognizing the signs and symptoms of a cardiac emergency
• Participate in community based cardiac education
• Need to use 911 and EMS
• PSA Announcements
STEMI Referring Hospital :
• Receive 12 lead ECG
• Provider notification and interpretation
• Local STEMI Treatment Team activation
• Implement early STEMI treatment
• Forwarding prehospital 12-lead ECG
• Timely arrangements for transfer to interventional care
• Feedback
Community EMS:
• Timely response, assessment, care and deployment of 12-lead ECG technology during a cardiac emergency
• Initiate pre-hospital care and prepare for transport to a receiving facility
• Acquisition and transmit of 12 lead ECG
STEMI Receiving Hospital
(PCI)
• Support referring facilities
• Receive 12 lead ECG from referring facility or EMS
• Provide consultation
• Interventional care
• Capturing STEMI data and reporting
• Feedback
Improving the System of Care for STEMI Patients
11
4/16/2020 ©2013, American Heart Association 12
GRANT
Mission: Lifeline
Nebraska The Grant
4/16/2020 ©2013, American Heart Association 13
Mission: Lifeline Nebraska Grant
5.3 million dollar initiative to enhance systems of care, save lives, and improve outcomes for heart attack patients in rural Nebraska, called Mission: Lifeline.
The lead funder for this investment in Nebraska is The Leona M. and Harry B.
Helmsley Charitable Trust, one of the nation’s largest foundations, providing a grant of $4.1 million to the American Heart Association for the initiative.
Other current funders include the Fund for Omaha through the Omaha
Community Foundation, the Ron and Carol Cope Charitable Fund, Aaron and
Rachel Wagner, Mid – Nebraska Community Foundation, Valmont Foundation,
Pinnacle Bank – Madison Branch and Hamilton County Foundation.
14
Mission: Lifeline NE Project Roll-out
1. Three year grant: February 2014 – February 2017
2. Statewide Mission: Lifeline Task Force a. Leadership b. Advisory Committees c. Interventional Cardiology Steering Committee
3. Equipment allocation
4. Protocol Development – Guidelines
5. Provider Education
6. Public Education Campaign
7. Data Collection
8. State STEMI Conference
15
Mission: Lifeline Nebraska - Timeline
MAY 2014 – JULY 2014
Mission: Lifeline Director
Hired
–
JULIE SMITH
Contact with all PCI capable facilities -
COMPLETED
Met with DHHS / EMS
Program director and specialists COMPLETED
Task Force Group
CREATED
Task Force leadership selected COMPLETED
Kick Off – Task Force
Meeting – HELD 7.9.2014
4/16/2020
AUG 2014 – DEC 2014 JAN 2015 - MAY 2015
Applications for EMS
Services to be finalized and sent to services -
COMPLETED
EMS Advisory Committee
Meeting and will review and determine eligibility – IN
PROGRESS
Award of first round funding for equipment
MOU and contract work for
PCI capable hospitals begins. Funding to start fall of 2014
Advisory Committees will begin meeting.IN
PROGRESS
I
Interventional Cardiology
Steering Committee
–
IN
PROGRESS
Reporting 1 st quarter data for Action Registry participating hospitals.
Second round funding for
EMS equipment will begin
Development of
Guidelines – NE approved
System of Care IN
PROGRESS
Advisory Committees will continue to meet as needed to review data
Mission: Lifeline
Statewide Conference
2015 AND BEYOND
Data collection continues
Continued EMS equipment funding
Hospital and EMS recognition
Quality Improvement efforts statewide based on registry data
2 nd Annual Mission:
Lifeline Statewide
Conference
©2013, American Heart Association 16
Rural NE PCI Capable Hospitals
PCI – 24/7
1. Faith Regional Health Services – Norfolk
2. Saint Francis Medical Center - Grand Island
3.
Good Samaritan Hospital – Kearney
4.
Kearney Regional Medical Center – Kearney
5. Great Plains Regional Medical Center – North Platte
6. Mary Lanning Healthcare – Hastings
PCI – Non 24/7
1. Fremont Area Medical Center – Fremont
2. Regional West Medical Center - Scottsbluff
4/16/2020 ©2013, American Heart Association 17
Nebraska PCI Hospitals
4/16/2020 ©2013, American Heart Association 18
NE CAHS
4/16/2020 ©2013, American Heart Association 19
PCI Referring Hospitals
NE Referring Hospitals 65 CAH hospitals
12-L receiving equipment funding available starting 2015
Referring Hospital Education
Plan Development will begin Fall of 2014 with delivery to begin in
Spring of 2015
4/16/2020
Improving the System of Care for STEMI Patients
20
Mission: Lifeline Nebraska Frequently Asked
Questions for Hospitals
1. Who is eligible to participate in the NE Mission: Lifeline statewide Taskforce?
2. Will all Hospitals be eligible to receive grant funding?
3. Are all hospitals required to participate in pre-hospital 12-lead transmission and receiving systems?
4. Will hospitals be required to purchase a particular brand of 12-lead ECG receiving equipment?
5. Will hospitals be eligible for reimbursement for equipment or software already purchased?
6. Will there be education for referring hospitals?
7. Will hospitals be required to participate in any data collection tool?
8. What is the timeline for the grant process?
Ineligible Counties
Cass County
Sarpy County
Lancaster County
Washington County
Douglas County
Saunders County
Seward County
21
Mission: Lifeline Nebraska Frequently Asked
Questions for EMS Agencies
1. Will all EMS agencies be eligible to receive grant funding?
2. Will EMS agencies be required to purchase a particular brand of equipment?
3. Will EMS agencies be eligible for reimbursement for equipment already purchased?
4. Will EMS agencies only be able to apply for 12-lead monitors?
5. How much funding (amount) can EMS agencies apply for?
6. What is the timeline for the grant process?
Ineligible Counties
Cass County
Sarpy County
Lancaster County
Washington County
Douglas County
Saunders County
Seward County
22
Taskforce & Committees
Mission: Lifeline
Nebraska Task Force
4/16/2020 ©2013, American Heart Association 23
M:L NE Meetings and Conferences
Biannual NE M:L Taskforce in person meetings
• Monthly Teleconferences
• Subcommittee meetings
Annual NE STEMI Summit Conference:
• Highlight NE successes and Lessons learned
• Hear from clinical experts about new science
• Network with peers to advance collaboration
• STEMI Survivor Celebration
• Recognize System excellence and award achievements
Improving the System of Care for STEMI Patients
24
Mission: Lifeline Nebraska
Committee Structure
Nebraska Mission: Lifeline Taskforce
• Composition: All interested volunteers: Nurses/Nursing leaders, EMS Providers, Leadership
& Medical Directors, Rural and Urban health care providers from Emergency medicine and
Cardiology. State Health Department partners. Other medical professionals and leadership interested in improving emergency cardiovascular care in Nebraska.
Nebraska Mission: Lifeline Chairs
• Composition: ED physician, 2 Cardiologists, Maximum 3 members
Interventional Cardiology Steering Committee
• Composition: Cardiologist representation from each PCI Hospital
Nebraska Mission: Lifeline Quality Committee
•
Composition: Quarterly teleconference with Hospital Participants involved in Cardiovascular
Care Quality improvement and/or the ACTION-GWTG Registry tool 10-20 members
25
Mission: Lifeline Nebraska
Committee Structure
Nebraska Mission: Lifeline STEMI Hospital Advisory Committee
• Composition: at least 1 nursing and 1 physician representative from each included PCI
Hospital, at least 1 representative from each regional non-PCI Hospital, and at least 2 EMS representatives (40 member maximum)
Nebraska Mission: Lifeline EMS Advisory Committee
•
Composition:
– DHHS EMS regional specialists
– EMS agency representatives from throughout the state
– EMS agency medical directors
– Other EMS representatives (max 18 members)
Nebraska Mission: Lifeline STEMI Conference Planning Committee
26
Leadership
Mission: Lifeline
Nebraska Task Force
Leadership
4/16/2020 27
Chairs 2014-2015
Dr. Matt Johnson
Matthew Johnson, MD, is an Alma, NE native. Dr. Johnson is an interventional cardiologist withe
Bryan Heart Cardiology group at Bryan Health. He providers outreach clinical services to several communities across NE. We are fortunate to have Matt as one of the task force leads. His knowledge of rural Nebraska will be a great resource.
Dr. Doug Kosmicki
Douglas. Kosmicki M.D. is a St. Paul, NE native. Dr. Kosmicki is an interventional cardiologist form the CHI Nebraska Heart Hospital and provides service to both Grand Island and Hasting PCI cath labs. He also serves rural communities providing outreach clinics. Doug will help provide insight from the central / rural areas of the state.
Dr. David Cornutt
Is the Medical Director for Emergency Services at Regional West Medical Center in Scottsbluff
Nebraska. He and his wife live on a ranch 80 miles from Scottsbluff. He worked in an urban
Emergency department for over 25 years and has in-depth knowledge of STEMI systems of care and is currently the Medical Director for the majority of EMS Services in the Panhandle. David’s rural and ED expertise are an essential part of representation needed.
Improving the System of Care for STEMI Patients
28
LEAD – Cardiology
Interventional Cardiology Steering Committee -
Dr. Steve Martin
Steve Martin, MD is a Nebraska Native. Dr. Martin is an interventional Cardiologist and the medical director for the Cardiovascular Service line for CHI/NHH in Lincoln. He is able to represent the overall CHI system concerning Cardiology here in Nebraska. As the lead for the
Interventional Cardiology Steering Committee he will work with statewide interventionists across the state on the statewide guidelines.
29
INTERVENTIONAL
CARDIOLOGIST STEERING
COMMITTEE
Dr. Arshad Ali
Interventional Cardiologist
Great Plains Health Center – North Platte
Dr. John Cimino
Interventional Cardiologist
Bellevue Medical Center – Bellevue
Dr. Azariah Kirubakaran
Interventional Cardiologist
Faith Regional Health Services
– Norfolk
Dr. Rick Markiewicz
Interventional Cardiologist
Kearney Regional Medical Center - Kearney
Dr. Dan McGowan
Interventional Cardiologist
Central Nebraska Cardiology - Kearney
Dr. Charles Olson
Interventional Cardiologist
Methodist Hospital – Omaha
Dr. Drew Purdy
Interventional Cardiologist
Rapid City Regional Hospital
Rapid City South Dakota
Dr. Steve Diamantis
Interventional Cardiologist
Fremont Area Medical Center - Fremont
30
LEAD – Hospital Advisory
Hospital Advisory Committee -
Dr. Ed Mlinek
Dr. Ed Mlinek, is the Medical Director for Bryan Medical Centers Emergency Services. In addition, through Bryan Health, he has participated in outreach efforts in rural areas and is familiar with the differing care models in these areas. He has also hosted EMTALA conferences for the Heartland Health Alliance and has been a CIMRO reviewer which has furthered is understanding of the care provided in the more rural facilities .
The Hospital Advisory Committee has good representation of PCI Capable facilities and CAH across the state.
31
Group Decision Making
Mission: Lifeline
Nebraska Task Force
4/16/2020 ©2013, American Heart Association 32
Consensus Based Decision Making
• Consensus Decision-Making – Participants make decisions by agreement rather than by majority vote.
• Inclusiveness – To the extent possible, all necessary interests are represented or, at a minimum, approve of the decision.
• Accountability – Participants usually represent stakeholder groups or interests. They are accountable both to their constituents and to the process.
• Facilitation – An impartial facilitator accountable to all participants manages the process, ensures the ground rules are followed, and helps to maintain a productive climate for communication and problem solving.
Improving the System of Care for STEMI Patients
33
Consensus Based Decision Making
• Flexibility – Participants design a process and address the issues in a manner they determine most suitable to the situation.
• Shared Control/Ground Rules – Participants share with the facilitator responsibility for setting and maintaining the ground rules for a process and for creating outcomes.
• Commitment to Implementation – All stakeholders commit to carrying out their agreement.
Improving the System of Care for STEMI Patients
34
Consensus Based Decision Making
Elements of a Consensus-Based Decision
• All parties agree with the proposed decision and are willing to carry it out
• No one will block or obstruct the decision or its implementation
• Everyone will support the decision and implement it.
Levels of Consensus
• I can say an unqualified “yes!”
• I can accept the decision.
• I can live with the decision.
• I do not fully agree with the decision, however, I will not block it and will support it.
Improving the System of Care for STEMI Patients
35
Mission: Lifeline South Dakota
Statewide STEMI Guideline
Introduction letter signed by members of Interventional
Cardiology Steering Committee representing all 7 PCI centers in the state sends a very powerful message on the need for standardized statewide guidelines.
Improving the System of Care for STEMI Patients
Data, Public Awareness
& Guidelines
Mission: Lifeline
Nebraska Task Force
4/16/2020
Improving the System of Care for STEMI Patients
37
Data
How Does the Nebraska Mission: Lifeline Project Support Data
Colletion?
• The PCI Capable Hospitals in the included rural areas will receive funding support to participate in ACTION Registry-GWTG for three years
• 24/7 PCI capable hospitals will also receive FTE support for data abstraction
*** Hospitals must agree to enter patients into ACTION Registry to receive any of these dollars
• All Hospitals will also be eligible for funding support for 12-L receiving software
• Non-funded, Metro PCIs are strongly encouraged to participate in ACTION
Registry to be part of the state system data.
Improving the System of Care for STEMI Patients
Mission: Lifeline® and
ACTION Registry ® - Get With The Guidelines™
Relationship
ACC
AHA
• Quality Improvement Specialists
• Mission: Lifeline Implementation
• Provide M:L Reports using AR-G data
M:L
Reports
• Keeper of AR-G Data
• Operational Support for data upload
• Executes Data Release Consent
Forms
• Analyze the AR-G data using logic specific to ACTION reports
• Posts AR-G and M:L Reports
DCRI
• Analyze the AR-G data using logic specific to M:L
4/16/2020 2012 AHA Mission: Lifeline 39
Mission: Lifeline Reports are generated through the NCDR Registry called
ACTION Registry-GWTG. This registry collects the data for the entire STEMI system and is the method for reporting outcomes, successes and understanding gaps.
Quarterly, hospitals will receive a Mission: Lifeline report in the Action Registry Dashboard
4/16/2020
4
1
Improving the System of Care for STEMI Patients
South Dakota Data Examples
4/16/2020
Median time FMC to
Primary PCI Overall % within
90 min
Median time FMC to Primary PCI
Overall % within 90 min
2013 Q1
2013 Q2
2013 Q3
2013 Q4
ML STEMI participating hospitals State Aggregate SD
55.0%
56.0%
61.0%
65.0%
ML STEMI participating hospitals
National Aggregate
59.0%
59.0%
59.0%
60.0%
©2013, American Heart Association 42
South Dakota Data Examples
4/16/2020
REC CTR Mission Lifeline
Composite Score
REC CTR Mission Lifeline
Composite Score
2013 Q1
2013 Q2
2013 Q3
2013 Q4
ML STEMI participating hospitals State Aggregate SD
96.9%
97.9%
98.3%
98.5%
ML STEMI participating hospitals National Aggregate
95.1%
95.3%
96.1%
96.3%
©2013, American Heart Association 43
South Dakota Data Examples
4/16/2020
2013 Q1
2013 Q2
2013 Q3
2013 Q4
SYSTEM Direct Pres
% of patients
Treated for reperfusion
SYSTEM Direct Pres
% of patients
Treated for reperfusion
SYSTEM Transfer In
% of patients
Treated for reperfusion
SYSTEM Transfer In
% of patients
Treated for reperfusion
ML STEMI participating hospitals State
Aggregate SD
95.0%
98.0%
ML STEMI participating hospitals National
Aggregate
90.0%
90.0%
ML STEMI participating hospitals State
Aggregate SD
92.0%
92.0%
ML STEMI participating hospitals National
Aggregate
91.0%
91.0%
96.0%
96.0%
90.0%
90.0%
94.0%
94.0%
91.0%
91.0%
©2013, American Heart Association 44
South Dakota Data Examples
4/16/2020
RC Median time FMC to
Primary PCI (min) Overall
RC Median time FMC to
Primary PCI (min) Overall
2013 Q1
2013 Q2
2013 Q3
2013 Q4
ML STEMI participating hospitals State Aggregate SD
86 min
85 min
80.5 min
77 min
ML STEMI participating hospitals National Aggregate
85 min
85 min
85 min
84 min
©2013, American Heart Association 45
Mission: Lifeline Reports will also capture referring hospital metrics for system improvement
STEMI referring Center Achievement Measures:
1. Percentage of STEMI patients with a door-to-first ECG time <10 minutes
2. Percentage of reperfusion – eligible patients receiving any reperfusion (PCI or fibrinolysis) therapy
3. Percentage of reperfusion – eligible patients with door-to-needle time within 30 minutes
4. Percentage of reperfusion – eligible patients transferred to PCI center with door-into door-out time within 45 minutes
* Facility goal to make STEMI referring Center ED FMC
– to device (balloon) within 120 minutes (including transport time)
5. Percentage of STEMI patients receiving aspirin within 24 hours
4/16/2020 ©2010, American Heart Association 46
Hospital and System Improvement
Strategies
• Know your numbers, data sources and benchmarks
• Understand the performance measures and understand who is key to success (FMC is a collaborative measure!)
• Develop plan for Q1 to achieve award Q2 – small tests of change
• Look at your “misses”, Evaluate process change based on trends
• Provide messaging to champions for hospital key partners and use your data!
• Communicate
©2010, American Heart Association 47
Mission: Lifeline Statewide STEMI
Guideline
Guidelines Constructed following the 2013 ACC/AHA Guidelines
I IIa IIb III
All communities should create and maintain a regional system of
STEMI care that includes assessment and continuous quality improvement of EMS and hospital-based activities. Performance can be facilitated by participating in programs such as Mission:
Lifeline and the D2B Alliance.
I IIa IIb III
Performance of a 12-lead ECG by EMS personnel at the site of
FMC is recommended in patients with symptoms consistent with
STEMI.
Mission: Lifeline Statewide STEMI
Guideline
Guidelines Constructed following the 2013 ACC/AHA Guidelines
I IIa IIb III
Reperfusion therapy should be administered to all eligible patients with STEMI with symptom onset within the prior 12 hours.
I IIa IIb III
Primary PCI is the recommended method of reperfusion when it can be performed in a timely fashion by experienced operators.
I IIa IIb III
EMS transport directly to a PCI-capable hospital for primary PCI is the recommended triage strategy for patients with STEMI with an ideal FMC-to-device time system goal of 90 minutes or less.*
*The proposed time windows are system goals. For any individual patient, every effort should be made to provide reperfusion therapy as rapidly as possible.
Mission: Lifeline Statewide STEMI
Guideline
Guidelines Constructed following the 2013 ACC/AHA Guidelines
I IIa IIb III
Immediate transfer to a PCI-capable hospital for primary PCI is the recommended triage strategy for patients with STEMI who initially arrive at or are transported to a non –PCI-capable hospital, with an
FMC-to-device time system goal of 120 minutes or less.*
I IIa IIb III
In the absence of contraindications, fibrinolytic therapy should be administered to patients with STEMI at non –PCI-capable hospitals when the anticipated FMC-to-device time at a PCI-capable hospital exceeds 120 minutes because of unavoidable delays.
*The proposed time windows are system goals. For any individual patient, every effort should be made to provide reperfusion therapy as rapidly as possible.
Mission: Lifeline Statewide STEMI
Guideline
Guidelines Constructed following the 2013 ACC/AHA Guidelines
I IIa IIb III
When fibrinolytic therapy is indicated or chosen as the primary reperfusion strategy, it should be administered within 30 minutes of hospital arrival.
*
I IIa IIb III
Reperfusion therapy is reasonable for patients with STEMI and symptom onset within the prior 12 to 24 hours who have clinical and/or ECG evidence of ongoing ischemia. Primary PCI is the preferred strategy in this population.
*The proposed time windows are system goals. For any individual patient, every effort should be made to provide reperfusion therapy as rapidly as possible.
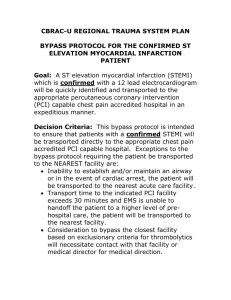
Mission: Lifeline South Dakota
Statewide STEMI Guideline
South Dakota
Page 1 –
Initial Treatment Guidelines
Definition of STEMI Patient
Blue section: Arrive by EMS
Starts the flowchart process
Follow the “yes” & “no”
Proceed to Page 2 or Page 3
Key items and goal in RED
Improving the System of Care for STEMI Patients
Mission: Lifeline South Dakota
Statewide STEMI Guideline
South Dakota
Page 2 –
Primary PCI Patients
FMC – PCI less than 120 min.
Key items and goal in RED
Improving the System of Care for STEMI Patients
Mission: Lifeline South Dakota
Statewide STEMI Guideline
South Dakota
Page 3 –
Fibrinolysis Patients
Greater than 120 min. to PCI
Door to Needle less than 30 min.
Contraindication to fibrinolysis
Key items and goal in RED
Improving the System of Care for STEMI Patients
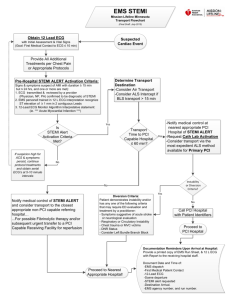
Mission:
Lifeline
Nebraska
STEMI EMS
Transport
Guideline
Draft
Improving the System of Care for STEMI Patients
55
Mission:
Lifeline
Nebraska
STEMI EMS
Transport
Guideline
Draft
Improving the System of Care for STEMI Patients
56
Mission:
Lifeline
Nebraska
STEMI EMS
Transport
Guideline
Draft
Improving the System of Care for STEMI Patients
57
Mission:
Lifeline
Nebraska
STEMI EMS
Transport
Guideline
Improving the System of Care for STEMI Patients
58
59
DIDO Goal
45 minutes or less
!
• Observed in-hospital mortality was significantly higher among patients with DIDO times >30 minutes than among those with
DIDO times <30 minutes
STEMI Statistics
• Acute Coronary Syndrome (ACS) will strike 935,000 people a year in the
United States, an estimated 250,000 of those will be STEMIs
• In 2011, 3,267 Nebraska Residents died from heart disease, according to the Nebraska Department of Health and Human Services.
• Heart disease is the #2 leading cause of death in Nebraska.
Heart Disease and Stroke Statistic 2011 Update: A Report From the American Heart Association
Statistics Committee and Stroke Statistics Subcommittee. Circulation 2011;123:e18-e209.
61
Opportunities for Improvement
Are patients not aware of S&S and calling 911, thus causing a delay in treatment/out of hospital death prior to treatment? This supports the need for enhanced public awareness/education.
Access to care? Do we currently have systems in place in which patients are not able to get to the appropriate facility in a timely fashion, thus supporting the need to improve systems of care so that patients are transported to a facility with a plan in place to treat based on guidelines.
4/16/2020 62
Public Awareness
4/16/2020
South Dakota
http:// www.youtube.com/watch?v=QMo07hyqugI http://www.youtube.com/watch?v=Zm5PJUMHPcQ
63
Public Awareness
North Dakota
4/16/2020 64
Public Awareness
Minnesota
4/16/2020 65
PCI Referring Hospitals
What does pre-hospital STEMI activation look like at your facility? Do you routinely call for the next leg of transfer pre-arrival?
• What are the greatest barriers in obtaining a door in- door-out of 45 min or less?
• What are the greatest barriers to obtaining a door to lytic administration time of < 30 minutes
• What are the greatest barriers to obtaining a door to ECG time of < 10 minutes?
• How do we break down political barriers and develop a unified voice for
NE?
Improving the System of Care for STEMI Patients
66
PCI Receiving Hospitals
• What mechanism is your facility currently utilizing for STEMI Data
Collection, Quality Improvement, Outreach and Feedback?
• What is the level of support for ACTION GWTG – ARG Participation at your facility?
• What are the greatest barriers within your network to achieving a:
– 90 FMC to Primary PCI reperfusion in your area? (non-transfers)
– 120 FMC to Primary PCI reperfusion in your area? (transfers)
Improving the System of Care for STEMI Patients
67
Going Forward
Bi-Annual Face to Face Taskforce Meeting
Annual NE STEMI Conference
Local, Regional, and State STEMI system of care development, optimizing the destination plans and protocols and feedback recommendation development.
Referring Hospital Education Curriculum Development and Delivery –
Learn Rapid STEMI ID and STEMI Provider Manual Distribution
Public Awareness Campaign Assessment, Development, and Delivery
Improving the System of Care for STEMI Patients
68
Going Forward
EMS Education Curriculum
Data Analysis and Quality Improvement
Model sharing
Public Media and Awareness campaign
Sustainability Plan Development
Improving the System of Care for STEMI Patients
69
Questions?
4/16/2020
Thank You!
2012 AHA Mission: Lifeline
70