Respiratory System - mrsmurraysmedicalcareersclass
advertisement

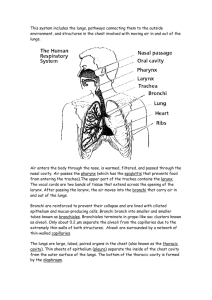
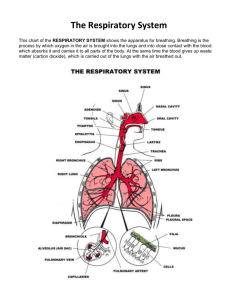
The Respiratory System Fun Facts • The highest recorded "sneeze speed" is 165 km per hour. • The surface area of the lungs is roughly the same size as a tennis court. • The capillaries in the lungs would extend 1,600 kilometers if placed end to end. • We lose half a liter of water a day through breathing. This is the water vapor we see when we breathe onto glass. Functions 2 Basic Functions: • 1. Air distribution • 2. Gas exchange • Supplies body w/ O2 • removes CO2 • O2/CO2 levels maintained homeostatically Additional functions • • • • 3. Filters, warms and humidifies air 4. Sound production 5. Olfaction 6. Homeostasis of gases, ph of blood Structures • • • • • • • Nose Pharynx Larynx Trachea Bronchi “Upside-down tree” –Bronchioles Lungs - Alveoli Upper Resp Tract Lower Resp Tract 1. Resp Mucosa • Membrane that lines most of the air distributing tubes of resp tract • Covered w/ mucous that cleanses, warms and humidifies inspired air. More than 125 ml of resp mucous produced daily • Covered w/ cilia that move debris out of resp tract, away from lungs NOSE • Made of bone and cartilage • External nares: nostrils: hair filters dust, blood vessels under surface warm air, mucous humidifies it • Div by nasal septum (vomer and ethmoid bones) • R&L nasal cavities: lined w/ nasal mucosa (ciliated epithelium) NOSE • Olfactory receptors: nerve endings responsible for olfaction (smell). They detect vaporized chemicals that have been inhaled **Sense organ • Functions: warm and humidify inhaled air; • Lacrimal sacs: tear ducts that drain into nasal cavities PARANASAL SINUSES • #4: frontal, maxillary, ethmoidal and sphenoidal • Frontal and maxillary are largest • Functions: lightens the weight of the skull, assists w/ sound and mucous production for resp tract • Lined w/ ciliated epithelial tissue • Mucous produced drains into nasal cavity • Sinusitis PHARYNX • • • • Muscular tube w/ resp & digestive function @ 5 inches long Divided into 3 sections: 1. Nasopharynx: directly behind nasal cavity for passage of air only; connects to middle ear by eustachian tubes • 2. Oropharynx: behind mouth • 3. Layrngopharynx: lowest segment; opens ant. into larynx & post into esophagus • Function: food and air passageway T0NSILS • Masses of lymph tissue embedded in mucous membrane • of pharynx LARYNX • Voice box • Located between the pharynx and the trachea • 2-inch-long, tube-shaped organ in the neck. • 9 pieces of cartilage bound by muscle and ligaments. Largest is thyroid cartilage (adams apple), lowest is cricoid cartilage • Functions: • 1. Air passageway between pharynx and trachea • 2. Sound production: vocal cords, two bands of muscle, form a "V" inside the larynx. These tighten up and move closer together. Air from the lungs is forced between them & makes them vibrate, produces the sound of our voice. The tongue, lips, teeth form this sound into words. • Glottis: space between cords LARYNX • Epiglottis: flap of cartilage that protects the trachea from food entry • The esophagus is just behind the trachea and larynx. The openings of the esophagus and the larynx are close together. When we swallow, this flap moves down over the larynx to keep food out of trachea TRACHEA • 12 cm (5 in)Tube-like portion of resp tract that connects the larynx with the bronchial tree 16-20 “C” shaped rings of cartilage that are stacked w/ little soft tiss in between • Open section of the C allows faces esophagus & allows for expansion of esophagus when food is swallowed • Strong tiss to prevent collapse during inspiration Upper Resp Disorders • • • • • • • Rhinitis Pharyngitis Laryngitis Deviated septum Epistaxsis Sinusitis Tonsilitis • Common cold: caused by over 200 viruses. Spread by direct contact and in air droplets. Often leads to secondary infection • Influenza: flu involving upper and lower resp tracts. Cause: virus and often leads to secondary infection that can be life threatening to young children and elderly TRACHEA • Lined w/ mucosa that is ciliated epithelial tissue • Cilia help sweep debris toward pharynx • Function: air passage to lungs • Complete obstruction: 5th cause of accidental death in US. Tx: Heimlich Maneuver • Branches into R & L primary bronchi that enter lungs BRONCHIAL TREE • Trachea branches into R&L primary bronchi which divide into smaller secondary bronchi in each lung • Bronchi divide into bronchioles which subdivide into alveolar ducts then alveolar sacs then alveoli in the lungs LUNGS • • • • • • • Large paired organs of thoracic cavity Function: gas exchange R lung has 3 lobes (sup, mid, inferior); L has 2 (sup, inferior) Apex: superior portion, under clavicle Base: inferior section, rests on diaphragm Hilus: indentation on medial surface of each lung where primary bronchus, pulmonary artery and veins enter each lung ALVEOLI • Functional unit of the lung • Millions in each lung surrounded by capillary network • Walls made of simple squamous epithelial tissue; elastic connective tissue between clusters necessary for exhalation • Each is lined with thin layer of tissue fl necessary for diffusion of gases • Surfactant: lipoprotein that lines the alveolus; decreases surface tension and prevents collapse of alveoli during respiration • Function of bronchus to alveoli: air distribution and gas exchange • Movement of gases between alveolus and capillaries occurs by diffusion PLEURAL MEMBRANES • AKA: respiratory membrane • Thin barrier between blood in capillaries and air in alveoli • Allows for diffusion of gasses due to the thinness of this membrane PLEURA • Covers outer surface of lungs and inner surface of rib cage • Function: reduce friction between lungs and chest wall • Parietal pleura: lines walls of thoracic cavity • Visceral pleura: covers lungs • Interpleural space: between these, contains serous fluid to reduce friction Lower Resp Tract Disorders • Pleurisy: inflammation of parietal pleura • Atelactasis: collapse of the lung; different causes • Pneumothorax: air in pleural space; caused by rib fx or can be spontaneous • Hemothorax: blood in pleural space • Tx: chest tube to allow lung to re-expand Respiratory Distress • RDS: Respiratory Distress Syndrome: inability of alveoli to inflate • Infant RDS: lack of surfactant in premature infants. AKA: Hyaline membrane disease • Adult RDS: due to irritant (chemical, smoke, vomit) that causes edema of alveoli Respiration • Exchange of O2 & CO2 between a living organism and the environment • External: movement of air in and out of lungs to allow for exchange of gases between lungs and capillaries • Internal: Exchange of gases between capillaries and cells of the body • Cellular: use of O2 by cells for metabolism Mechanics of Breathing • Pulmonary ventilation: involuntary muscular work and a change of air pressure in thoracic cavity. Occurs in 2 stages: • Inspiration: moves air into lungs; active • Expiration: moves air out; passive • Resp muscles: diaphragm and intercostals Inspiration • Thoracic cavity enlarges allowing air to enter • Motor impulse from medulla to resp muscles • Diaphragm contracts and flattens; ^ thoracic cavity size • External intercostals contract & pull ribs up and out; ^ thoracic cavity size from front to back/side to side • ^ size = decreased pressure in thoracic cavity the result air entry into lungs. Expiration • Impulse stops, muscles relax • Thoracic cavity returns to smaller size which ^ pressure, lungs recoil and decrease in size forcing air out (passive) • Forceful expiration: expiratory muscles the internal intercostals/abdominal muscles contract to further decrease size of thoracic cavity • ^ air press in thoracic cavity result air flows out of lungs O2-CO2 Exchange 1. O2 concentration ^ in alveoli, low in capillaries. 2. CO2 is reverse low in alveoli ^ in capillaries Gases move by diffusion: move from high to low press gradient which is passive transport mechanism Gas exchange in Lungs • AKA external respiration • O2 moves out of alveolar air into blood and combines w/ Hgb in lung capillaries to form oxyhemoglobin. • This bond is unstable so when bld passes thru tiss capillaries w/ low O2 concentrates it breaks and releases O2 to diffuse from RBC into tissue cell • CO2 diffuses in opp direction (into RBC) • Some binds w/ Hgb to form carbaminohemoglobin • Most CO2 is carried in plasma in the form of bicarbonate ion. It combines w/ H2O to form carbonic acid (H2CO3) which will disassociate to form H and HCO3 (bicarb) • In lungs, CO2 will dissociate from bicarb and carbamino to diffuse out of bld into alveolar air Gas Exchange in Tissues • AKA internal respiration • Tissue capillaries: site for breakdown of oxyhemoglobin • O2 then moves out of cap and into cells of the tissue • O2 necessary for metabolic activity/cell respiration • O2-CO2 move by diffusion: O2 moves from cap bld to cells in tiss; CO2 does reverse • CO2 leaves tiss cells and enters capillaries where bicarb/carbaminohemoglobin forms to transport it to the lungs Volumes of Air Exchanged • Normal inspiration takes in @ 500ml of air • Tidal volume: amt of normal inspiration/expiration • Vital Capacity: largest amt that can be inspired/expired in 1 breath (@ 4800 ml in young adult) • Expiratory Reserve: amt of air forcibly exhaled after tidal volume (@ 10001200ml) • Inspiratory Reserve: amt of air forcibly inhaled • VC = TV + IRV + ERV • Residual volume: air that remains in the lungs after forcible expiration (@ 1200ml) • VC = TV + IRV + ERV • Total Lung Capacity = VC + resid vol (5700-6200ml) Regulation of Respiration • Nervous and chemical regulation allow the body to adapt to changing demands for O2 Nervous Sys Regulation • Resp control centers in medulla and pons: send impulses to the muscles of respiration based on input from receptors throughout the body • O2, CO2, ph of bld, amt of stretch in lung tissue send messages to medulla to adapt respiratory rate • 2 most important control centers are insp/exp centers of medulla • Inspiratory center in medulla automatically generates impulse to produce resp rate @ 12-18 breaths per minute • Impulse from medulla to nerves to resp muscles to stimulate contraction result = inhalation • Lungs inflate causing stretch which generates impulse to medulla to depress inspiratory center & stimulate expiratory ctr which will decrease # impulses to resp muscles result = exhalation • Chemoreceptors: specialized cells in carotid/aortic bodies that respond to varying gas and ph levels to modify respiratory rate • Pulmonary stretch receptors: in airway/alveoli: stimulated when tidal vol is reached and inhibit inspiratory center – prevents overinflation • Cerebral cortex: limited/voluntary control of breathing Chemical Regulation • Chemoreceptors located in carotids and aorta detect changes in ph, O2 and CO2 levels of blood • Decreased ph due to ^^ CO2 causes acidosis • Medulla will respond by ^^ resp rate to exhale more CO2 and ^^ O2 levels to decrease acidity of blood Breathing Terms • • • • • Eupnea: normal breathing Hyperventilation: rapid/deep Hypoventilation: slow/shallow Dyspnea: difficult Orthopnea: dyspnea relieved in upright position • Apnea: no respirations • Cheyne-Stokes: cycles of hyperventilation/dyspnea + apnea • Hypoxia: Insufficient O2 to tissue • Respiratory arrest: failure to resume breathing after period of apnea More Respiratory Disorders • Bronchitis: URI • s/s: non-prod then prod cough • Tx: antibiotics (often this is a secondary inf) • Pneumonia: acute lung infec/inflamm, airway blocked w/ exudate (thick fl). Strept is common cause • s/s: fever, malaise, h/a, cough, chest pain • Aspiration pneumonia, bronchial, lobar • Tx: antibiotics, mechanical ventilation if resp distress is severe • TB: chronic contageous (airborne) lung inf. Caused by mycobacterium tuberculosis • s/s: fatigue, pleurisy, wt loss, fever, dyspnea • Tx: long term antibiotics • Pleural Effusion: excess fluid in pleural space; often caused by infection, heart failure or CA TB Pleural effusion Obstructive Disorders • COPD: progressive, often irreversible obstruction of airflow • Includes: chronic bronchitis (chronic inflammation usually c/b smoking), emphysema (chronic bronchitis causing rupture of alveoli), asthma (spasm of smooth muscle tissue in smaller bronchial air passages) • Tx: primarily symptomatic Lung CA • Malignancy of pulmonary tissue that can metastasize • s/s: none until well advanced; smokers cough, wt loss, hoarseness • Tx: lobectomy, pneumonectomy, chemo, radiation • One of the most common type of CA Chemical Imbalance • Resp acidosis: CO2 accumulation due to decreased resp rate (excess H ions cause decreased ph) ^ H = Acidosis when Ph starts drifting below 7.47 • Resp alkalosis: Low CO2 blood levels due to ^ resp rate eg. hyperventilation decreased H= Alkalosis when Ph starts ^^ above 7.47