Preventive Medicine
advertisement

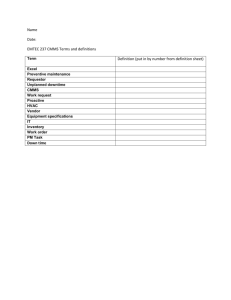
American Board of Preventive Medicine Careers in Preventive Medicine in the 21st Century Cheryl S. Barbanel, MD, MBA, MPH, FACOEM Boston University School of Medicine Public Health Achievements and Current Public Health Issues Ten Great Public Health Achievements United States 1900 - 1999 MMWR 4/2/99/48(12);241-243. Vaccination Motor-vehicle safety Safer workplaces Control of infectious diseases Decline in deaths from coronary heart disease and stroke Safer and healthier food Healthier mothers and babies Family planning Fluoridation of drinking water Recognition of tobacco use as a health hazard Leading Causes of Death Death Rate for Infectious Diseases Emerging Disease Issues Antibiotic resistance Foodborne and Waterborne Diseases Vectorborne and Zoonotic Diseases Disease transmission by blood Chronic diseases caused by infectious agents Vaccine development and use Travelers, immigrants, and refugees and disease transmission Environmental Conditions Favoring the Spread of Infectious Disease Globalization of the food supply Development projects that alter the habitat of disease carrying insects and animals Increased human contact with the wilderness habitat that may harbor unknown infectious agents Increased use of antimicrobial agents and pesticides hastening resistance Demographic Conditions Favoring the Spread of Infectious Disease Population growth and movement due to man made and natural disasters Global travel Human behaviors such as intravenous drug use and risky sexual behaviors The Role of Physicians in Public Health in Biological and Chemical Terrorism CDC calls for integrated training designed to ensure core competency in public health preparedness and the highest level of scientific expertise on local, state and federal levels The proportion of students of public health who were physicians declined from 35% in 1944 to 11% in 1978 What is Preventive Medicine? Preventive medicine physicians work with large population groups as well as with individual patients to promote health and understand the risks of disease, injury, disability and death. Prevention Primary Prevention - preventing the occurrence of disease and injury, for example by immunizations. Secondary Prevention - early detection and intervention, by reversing, halting or retarding the progression of a condition. Tertiary Prevention - minimizing the the effects of disease and disability by surveillance and maintenance to prevent complications. Preventive Medicine Competencies Biostatistics Epidemiology Environmental and occupational medicine Planning, administration, evaluation of health services Social and behavioral aspects of health and disease Practice of prevention in clinical medicine Careers in Preventive Medicine Preventive Medicine Physicians Have Key Roles In: Global environmental risk assessment Health care systems Prevention and control of infectious diseases Careers in Preventive Medicine Preventive Medicine Physicians May Specialize In One of Three Areas: Aerospace Medicine Occupational Medicine Public Health/General Preventive Medicine Where Do Preventive Medicine Physicians Work? Public health agencies Community agencies Outpatient and primary care settings Industry Managed care organizations Academia What Do Preventive Medicine Physicians Do? Initiate programs in the infectious disease prevention and control Manage programs in public and community health and research Provide patient care (nearly 70%) Identify health and safety hazards in the workplace to prevent illness and injury Work to improve preventive health services in the underserved and high risk populations The Public Health Physicians Direct multidisciplinary teams to provide health services on the city county or state level Plan community intervention programs (e.g. vaccination programs) Serves on task forces that solves community problems Provides clinical services in traditional public health areas - tuberculosis, sexually transmitted diseases, or primary care settings International Health Preventive Medicine Physician Assess Disease Risks for the Global Environment Diseases that have no respect for national boundaries: AIDS/HIV and tuberculosis Diseases more common in developing countries: malaria, cholera Diseases associated with under-nutrition Preventive Medicine Physicians in Medical Administration Serve as director of health departments and corporate medical departments Work as managers of HMO’s or group practices, community-based clinics or university-based health centers The Preventive Medicine Physician in Academic Medicine Research and teach in medical schools, public health schools, and other institutions Teach clinical prevention, epidemiology, and health services administration Research prevention of HIV and TB transmission, cancer, and the role of life style modification in prevention of disease Preventive Medicine Physician in Clinical Practice Identifying risk factors and methods of intervention for chronic, occupational, infectious disease and/or sexually transmitted diseases Develop practice guidelines, quality assurance and utilization review programs Practice medicine in primary care, sports medicine, exercise physiology, behavioral epidemiology, addiction medicine, geriatrics or maternal and child health American College of Preventive Medicine (ACPM) National medical specialty society for physicians committed to disease prevention and health promotion Represent more than 2,000 physicians boarded in preventive medicine and other specialties (e.g., family practice, internal medicine, pediatrics, emergency medicine, psychiatry, etc.) Leadership in the science, policy, and practice of preventive medicine Preventive Medicine Trends and The Public Health Workforce Public Health Workforce Physician Trends Small number of certified specialists in Public Health / Preventive Medicine Decline in proportion of self-designated preventive medicine specialists among U.S. physicians Decline in total number of preventive medicine residents with greatest decline in number of public health residents American Board of Preventive Medicine Living Diplomats by Certifications 2000 Aerospace Medicine Occupational Medicine Public Health and / or General Preventive Medicine TOTAL Unduplicated* living diplomats *Counts those with multiple PM certifications only once 922 2563 2839 6324 5966 Preventive Medicine Residency Training 1993 - 1999* Year Programs 1993 1994 1995 1996 1997 1998 1999 82 85 89 89 89 90 88 Residents 441 448 434 381 438 420 426 * Source: AMA GME Database, copyright 1993-1998, Chicago IL Distribution of Residents in Preventive Medicine Programs General Preventive 35% Public Health 16% Aerospace 15% Occupational 34% Needed Incentives to Address Public Health Workforce Trends Include preventive medicine explicitly in specialty mix to meet national workforce needs Support for infrastructure departments of preventive medicine in medical schools – – Health departments Schools of public health / graduate MPH programs Preserve loan forgiveness for preventive medicine trainees – Add tuition reduction for academic year Funding Sources for Preventive Medicine Training Programs Federal • HRSA • VA • NIOSH • CDC • HCFA • NASA • NIH • DoD • NASA State/Other • Health agencies • Public health schools • University medical centers • Foundations • National health organizations • Private industry COGME Resource Paper Preventive Medicine Workforce Recommendations: Increase the number of physicians with public health competencies Increase funding of preventive medicine residents, programs, faculty and faculty development Increase funding through Title VII, Medicare GME, and National Health Services Corps scholarships http://www.cogme.gov/resourcemain.htm Occupational and Environmental Medicine A Medical Career for the 21st Century Occupational Medicine The specialty devoted to the prevention and management of occupational injury, illness, disability, and the promotion of health and productivity. Environmental Medicine The branch of medical science devoted to the prevention and management of adverse health outcomes from exposure to chemical or physical agents in the home and community or their effect on the environment. The U.S. Workforce • U.S. Population, 270.4 million • U.S. Workforce, 137.2 million • Persons employed, 131.1 million • Employee to population ratio, 48.5% • Male workforce, 55% • Female workforce, 45% Source: US Bureau of Labor Statistics 1999 Non-Fatal Occupational Injuries 8,000,000 per year Overexertion 27.7% Contact with objects 27% Falls 16.2% Exposure to toxics 4.6% Repetitive motion 4.1% Transportation accidents 4% Slips/trips 3.1% Assault 0.9% Fires/explosions 0.2% Source: Bureau of Labor Statistics 1999 All other 11.9% Occupational Illness 429,800 Per Year Disorders associated with repeated trauma 64.3% Skin diseases, disorders, 13.4% Respiratory conditions due to toxic agents, 4.7% Disorders due to physical agents, 3.8% Poisoning, 1.1% Dust diseases of the lungs, 0.6% All other occupational diseases, 11.7% Source: Bureau of Labor Statistics 1999 The OEM Physician Workforce AMA estimates 10,000 physicians who do some occupational medicine 2,400 Board-certified occupational medicine physicians since 1955 1,500 - 1,800 are actually in practice National need - 5,000 Bureau of Health Professions needs estimate - 4,830 Institute of Medicine needs estimate - 3,100 - 5,50 Institute of Medicine’s Report Safe Work in the 21st Century Recommended an increase in the supply of physicians and other practitioners who have the skills to evaluate, treat and prevent ill health in the workplace OEM Sites of Practice Physician’s office OEM clinic Multi-specialty clinic Industrial site Corporation headquarters Academic institution Governmental agencies – Public health service – Veteran’s Administration – Military – Department of Labor – Centers for Disease Control and Prevention The Occupational Medicine Residency Program Year 1: The clinical year (internship) Year 2: The academic year (M.P.H., M.S. or equivalent) Biostatistics and epidemiology Health services organization and administration Environmental and occupational health Social and behavioral influences on health Industrial hygiene Ergonomics Industrial toxicology Occupational diseases Year 3: The practicum year (study with industry) The Practicum Year Didactic education and topics of occupational medicine importance Participate in data gathering and analysis Four months or more engaged in supervised practice within the world of work Clinical care of workers Management responsibilities in planning, administration and supervision of occupational medicine programs Characteristics of the Occupational and Environmental Medical Specialty • Broad scope of practice • Variety of practice settings • Treatment of individual workers • Population-based preventive medicine • Resource for regulations and policies Challenges Facing Occupational and Environmental Medicine • Effective use of health care resources • Compliance with government rules and regulations • Technological advancement and shifting work force demographics • Social, ethical and moral attitudes • Global industrial development and its impact on the work force An exciting, challenging career awaits the occupational and environmental medicine physician in the 21st century Aerospace Medicine Aerospace Medicine Definition The specialty area of Preventive Medicine that deals with the clinical and preventive medical requirements of man in atmospheric flight and space The Flight Surgeon Initially this was driven by a need for qualified military pilots to fly planes in war The Flight Surgeon’s Role Main function was to first develop and then apply physical qualifications for flight duty Driven by high losses of life due to physically unqualified pilots History After World War II the technological advances were applied to the airline industry. Increases in aircrew led to increases in civilian aviation medicine. History In the 1960’s advances were made to meet the challenge of manned flight beyond the earth’s atmosphere. . .Aviation Medicine evolved to Aerospace Medicine Aerospace Medical Issues Related to the Requirements of Flight and Space Trapped air Sinus block Ear block Decompression sickness Effects of acceleration forces Spatial Disorientation Zero Gravity Motion Sickness Cardiovascular Neurovestibular Musculoskeletal Psychiatric How to Become a Flight Surgeon Initially one must first be a physician – – Medical School Internship Then must decide if you want to… – Do a residency in Aerospace Medicine » » – – Civilian Military Or attend a short course that will permit you to do flight medicine in the military Or be an Aviation Medical Examiner as a civilian Short Courses Military – – – Air Force, Navy, and Army offer courses that range from 6 weeks to 6 months that prepare you to be a field flight surgeon. (Most of the actual learning in this occurs on-the-job) Emphasis is on being a member of the aircrew so that you can interact with aircrew in their environment Requires that the physician meet same physical standards that the aircrew must meet and participate in regular flying duties Civilian FAA offers training programs for the position of Aviation Medical Examiner (AME) through seminars throughout the US and through formal on-site training at the Civil Aviation Medicine Institute (CAMI) in Oklahoma City. Qualifies the physician to perform Class 2 examinations. Residency in Aerospace Medicine Offered both by the military (Navy and Air Force) and by two civilian universities: » » University of Texas Medical Branch (UTMB) at Galveston Wright State University in Dayton, Ohio A year of ACGME-accredited clinical training is required for admission to the residency. Each residency program includes an initial year of training to obtain a masters degree in public health and a practicum year covering the physiologic, environmental and clinical aspects of Aerospace Medicine. Board Certification in Aerospace Medicine After completing a residency in aerospace medicine and Qualifying for and passing the American Board of Preventive Medicine Examination, Board certification can be achieved in the specialty of Aerospace Medicine. Aerospace Medicine There are many problems with the abnormal environment encountered in aviation and space. The flight surgeon is just one of many highly trained individuals working to minimize the effects of these adverse effects so that man can continue to have mastery over the air and space. American Board of Preventive Medicine Incorporated in 1948 Authorized by American Board of Medical Specialties 1949 First Certificate Awarded in 1949 Certificates Issued 1949 - 2001 General Certificates • • • • • Aerospace (1953-2001) Occupational (1955-2001) Public Health/General Preventive (1983-2001) Public Health (1949-1982) General Preventive (1960-1982) 1266 3026 1623 1866 547 Subspecialty Certificates • • • Undersea Medicine (1993) Medical Toxicology(1995-2000) Undersea and Hyperbaric Medicine (2001) TOTAL (1949-2001) 10 23 78 8439 Why Board Certification Provide assurance to the public Physician specialist certified by a Member Board of ABMS has successfully completed – – An approved educational program and evaluation process An examination designed to assess Knowledge, skills and experience required to provide quality patient care WHAT ARE THE REQUIREMENTS Medical School Graduate Current Unrestricted License(s) Clinical Year of Training (PGY-1) Academic Year (MPH or equivalent) Practicum Year Currency of Practice Practice (Alternative and Special Pathways) Alternative Pathway to Certification Available only for medical school graduates prior to January 1, 1984 Must document training and experience Academic: – Four Core Courses » Biostat., Epi., Admin./Mgmt., Env. Health Practice Experience Combined IM/PM Training Programs Guidelines approved by both boards in January 1993 Update to Guidelines in preparation At least four years formal training Three programs approved by both boards Must be accredited by both residency review committees Requirements for practicum experience Continuity of care requirements Potential for similar combined training with other specialties Medical Toxicology Joint effort with Emergency Medicine & Pediatrics Approved by ABMS in 1992 Subboard established in 1992 Actions approved by Parent Boards Undersea and Hyperbaric Medicine Undersea Medicine – Approved by ABMS in 1989 – First examination given in 1992 – Name change to Undersea & Hyperbaric Medicine approved March 18, 1999 – Exam open to other ABMS diplomates – Exam given annually starting in November 1999 Re-certification Requirements GENERAL – Certificates Issued in and after 1998 are Time-Limited to 10 years – Valid ABPM Specialty Certificate – Unrestricted License in U.S. or Canada – Application: Requirements of ABPM consistent with ABMS Re-certification Requirements SPECIFIC - Maintenance of Certification (ABMS) - Professional Standing - Lifelong Learning & Self-Assessment - Cognitive Expertise (Examination) - Practice Performance Assessment ABPM WWW Home Page What is Available? – – – – Application Forms Information Book Frequently Asked Questions & Answers Study Guide & Exam Content Outlines http://www.abprevmed.org American Board of Preventive Medicine 330 South Wells Street Chicago, IL 60606 Tel: 303-939-ABPM [2276] Fax: 312-939-2218 Residency Program History Linkages ACGME Status Academic Year Format Practicum Year Resources American Board of Preventive Medicine www.abprevmed.org American College of Occupational and Environmental Medicine www.acoem.org Aerospace Medical Association www.asma.org American College of Preventive Medicine www.acpm.org American Public Health Association www.apha.org Association of Teachers of Preventive Medicine www.atpm.org Resources (con’t) HRSA/Bureau of Health Professionals www.bhpr.hrsa.gov Association of Schools of Public Health www.asph.org Association of Preventive Medicine Residents www.acpm.org/apmr/htm Accreditation Council for Graduate Medical Education www.acgme.org American Medical Association Fellowship and Residency Interactive Electronic Database www.ama-assn.org/cgi-bin/freida/freida.cgi Sources of Information American College of Preventive Medicine American College of Occupational and Environmental Medicine Aerospace Medical Association “Preventive Medicine and Public Health Workforce Trends: Threats and Solutions”, a presented at Prevention 2000 by Dorothy S. Lane, M.D., M.P.H. CDC’s Ten Great Public Health Achievements – United States 1900-1999 www.cdc.gov/epo/mmwr/preview/mmwrhtml/0005679 6.htm Acknowledgements Thanks to the members of the ABPM Client Services and External Relations Committee for their support and assistance with this presentation. Thanks to Ms. Yolanda Rodriguez and Mr. Michael Moskowitz, staff of the Boston University Occupational Health Center for their administrative assistance.