Higher Human Biology unit 2 section 1 REPRODUCTION
advertisement

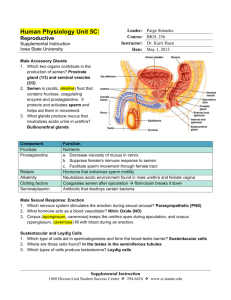
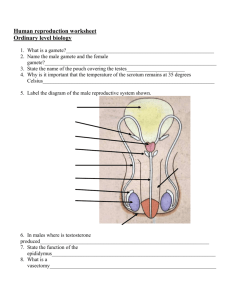
Physiology and health Unit 2 • 1 Reproduction • (a) (i)The structure and function of reproductive organs and gametes and their role in fertilisation. • Gamete production in the testes. The roles of seminiferous tubules, interstitial cells, testosterone, prostate gland and seminal vesicles. Gamete production in the ovaries to include maturation of ova and the development of a follicle. Site of fertilisation in the oviduct and zygote formation. • (ii) Testes produce sperm in the seminiferous tubules and testosterone in the interstitial cells. The prostate gland and seminal vesicles secrete fluids that maintain the mobility and viability of the sperm. • The ovaries contain immature ova in various stages of development. Each ovum is surrounded by a follicle that protects the developing ovum and secretes hormones. Mature ova are released into the oviduct where they may be fertilised by sperm to form a zygote. • Reproductive Organs and Hormones MALE REPRODUCTIVE SYSTEM BLADDER URETER SEMINAL VESICLE PUBIC BONE PROSTATE GLAND RECTUM URETHRA ERECTILE TISSUE COWPER’S GLAND VAS DEFERENS PENIS EPIDIDYMIS TESTIS SCROTUM TESTES SEMINIFEROUS TUBULE INTERSTITIAL CELLS Male reproductive system • Gametes (sex cells) are produced from germline cells. • In males, sperm are produced in seminiferous tubules found in the testes. The surrounding interstitial cells produce the male hormone testosterone which stimulates sperm production. • The prostate gland and seminal vesicles secrete fluids that maintain the mobility and provide nutrients for the sperm. FEMALE REPRODUCTIVE SYSTEM OVIDUCT ENDOMETRIUM OVARY CERVIX UTERUS VAGINA THE OVARIES GRAAFIAN FOLLICLE Female reproductive system • The ovaries contain immature ova in various stages of development. Each ovum is surrounded by a follicle that protects the developing ovum and secretes hormones. Mature ova found inside Graafian follicles are released into the oviduct where they may be fertilised by sperm to form a zygote. • b) Hormonal control of reproduction. • (i) Hormonal onset of puberty. • Pituitary gland releases follicle stimulating hormone (FSH),luteinising hormone (LH) or interstitial cell stimulating hormone (ICSH) via the hypothalamus Hormonal Control Hormones – recap! • Hormones are chemical messengers produced by cells that bind to receptors on the plasma membrane of other cells or enter other cells and alter the metabolic function of these cells. • In response to a signal from the brain, hormones are secreted directly into the blood by the glands that produce and store them to travel to a specific target organ. These glands make up what is known as the endocrine system. Hormonal Onset of Puberty • At puberty the hypothalamus secretes a releaser hormone that targets the pituitary gland • The pituitary gland is stimulated to release: • follicle stimulating hormone (FSH) • Luteinising hormone (LH) in women • Or interstitial cell stimulating hormone (ICSH) in men • These hormones control the onset of puberty Hormonal onset of puberty • At puberty, the hypothalamus starts to produce a releaser hormone. This stimulates the pituitary gland to start releasing: • Male: 1. Follicle Stimulating Hormone (FSH) Interstitial Cell Stimulating Hormone • Female: 1. FSH 2. Luteinising Hormone (LH) 2. (ICSH) • (ii) Hormonal control of sperm production. • FSH promotes sperm production and ICSH stimulates the production of testosterone Gametes are produced from germline cells. Hormones control the onset of puberty, sperm production and the menstrual cycle. • The pituitary gland is stimulated to release follicle stimulating hormone (FSH) and luteinising hormone (LH)/interstitial cell stimulating hormone (ICSH) by a releaser hormone produced in the hypothalamus. Hormonal Control of Sperm Production Male Hormones • FSH (follicles stimulating hormones) promotes spermatogenesis in seminiferous tubules • ICSH (Interstitial cellstimulating hormone) stimulates interstitial cells to produce male hormones (eg testosterone) • Testosterone also stimulates sperm production and activates the prostate gland and seminal vesicles NEGATIVE FEEDBACK CONTROL • High levels of testosterone have an inhibitory effect on the pituitary gland • Inhibits secretion of FSH and ICSH • Thus, levels of testosterone fall • Inhibitory effect on pituitary ceases • FSH and ICSH secretion increases • Levels of testosterone increase Hormonal control of sperm production • FSH promotes sperm production. • ICSH stimulates the production of testosterone which stimulates sperm production. • Together, FSH and ICSH exhibit negative feedback control on the pituitary gland. REMEMBER…. •F •I •T •F •L •O •P • (iii) Hormonal control of the menstrual cycle. Development of a follicle and the endometrium in the uterus. • Roles of FSH, LH, oestrogen and progesterone in the menstrual cycle. Development of a follicle, the corpus luteum and the endometrium. Follicular and luteal phases. Blastocyst implantation. Negative feedback control through pituitary gland, FSH and progesterone, leading to menstruation. Hormonal Control of the Menstrual Cycle ABPI schools • Hormones and the menstrual cycle: • http://www.abpischools.org.uk/page/modules/hormones/horm4.cfm ?coSiteNavigation_allTopic=1 Abpi schools • Hormones drag and drop exercise • http://www.abpischools.org.uk/page/modules/hormones/horm2.cfm ?coSiteNavigation_allTopic=1 MENSTRUAL CYCLE • Takes on average 28 days • Menstruation is day 1 to 5 of the cycle • Endometrium then starts to repair • Ovulation day 14 • Endometrium thick and spongy • Menstruation in absence of fertilised egg Hormonal control of the female menstrual cycle • The menstrual cycle takes approximately 28 days. • The first day of menstruation where the old endometrium (uterus lining) is shed (this lasts approximately 5 days) is regarded as day one of the cycle. Menstrual Cycle – day 1-14 LH FSH OESTROGEN PROGESTERONE Hormonal control of the female menstrual cycle • The first 14 days are called the follicular phase. FSH stimulates the development of a follicle in the ovary and also stimulates the production of another hormone- oestrogen - by the follicle. • The levels of oestrogen gradually build up. This stimulates proliferation of the endometrium, preparing it for implantation. It also makes mucus produced by the cervix much thinner, making it easier for sperm to penetrate. • Peak levels of oestrogen on day 14 stimulate a surge in the secretion of LH which triggers ovulation. Menstrual Cycle – day 15- 28 FERTILISATION Hormonal control of the female menstrual cycle • Days 14 – 28 are called the luteal phase. Once the egg has been released, the surrounding follicle develops into a corpus luteum and secretes progesterone which promotes further development and vascularisation (formation of blood vessels) of the endometrium, preparing it for implantation of the blastocyst (developing embryo) in the endometrium if fertilisation has occurred. • High levels of ovarian hormones (oestrogen and progesterone, produced by the ovary) exhibit a negative feedback effect on the pituitary hormones ( FSH and LH) thus reducing their release and preventing further follicles from developing in the ovary and being released. • If there is no pregnancy, a decrease in LH which maintains the corpus luteum leads to degeneration of the corpus luteum. It then stops producing progesterone which then leads to the endometrium being shed during menstruation. • (c) The biology of controlling fertility. • Infertility treatments and contraception are based on the biology of fertility. Risks and ethics associated with fertility treatments. • (i) Fertile periods. • Cyclical fertility in females leading to a fertile period. Continuous fertility in males. Calculation of fertile periods and their use. • (ii) Treatments for infertility. • Stimulating ovulation. Ovulation stimulated by drugs that prevent the negative feedback effect of oestrogen on FSH secretion. • Artificial insemination. Several samples of semen are collected over a period of time. If a partner is sterile a donor may be used. • Intra-cytoplasmic sperm injection (ICSI). • If mature sperm are defective or very low in number ICSI can be used — the head of the sperm is drawn into a needle and injected directly into the egg to achieve fertilisation. • In vitro fertilisation (IVF). • Surgical removal of eggs from ovaries after hormone stimulation. Incubation of zygotes and uterine implantation. Pre-implantation genetic screening to identify genetic disorders and chromosome abnormalities. • • Biology of Fertility Control Menstrual Cycle – day 15- 28 Fertility • Females exhibit cyclical fertility, with a fertile period for the few days surrounding ovulation and then otherwise infertile. At ovulation, body temperature increases by approx 0.5°C so the fertile period can be calculated. • Males exhibit continuous fertility – their levels of fertility do not change.