male
advertisement

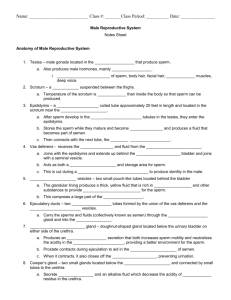
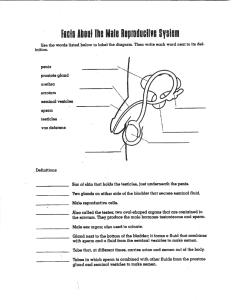
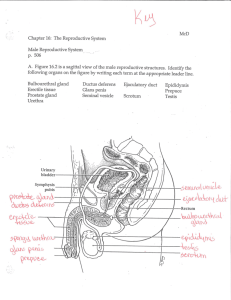
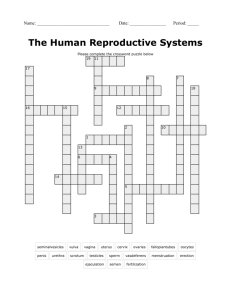
THE MALE REPRODUCTIVE SYSTEM Presented by Breck Peterson What are the male genitals? External Penis Scrotum Testes Internal Epididymis Vas deferens Seminal vesicles Prostate gland Cowper’s glands Urethra Diagram http://kidshealth.org/teen/interactive/mrs_it.html Penis Glans (head) Corona Frenum/frenulum Urethral meatus Shaft Foreskin Corpus spongiosum Corpus cavernosa Scrotum and Testes Form and function: Penis urethral meatus: the opening of the urethra, where urine comes out when you urinate. It's also where pre-ejaculatory fluid and semen come out of the penis. The urethra inside the penis has both a urinary function and a reproductive one The urethral meatus is usually located in the center of the head or glans of the penis, the mushroom or helmet-shaped, somewhat bulbous, section that composes the end of the penis The little ridge that runs all the way around the bottom of the head of the penis is called the corona just below the spot on the underside of the penis where the corona makes a little V shape is the frenum (sometimes called the frenulum) When blood flows into the penis to create an erection, it goes into and fills up two spongy bodies of tissue that run the length of the penis. The corpus cavernosum runs along the top of the penis, and another similar body called the corpus spongiosum runs along the urethra. Form and Function: Scrotum and Testes The scrotum is the little bag of skin lined with muscle that hangs below the penis and contains the testes or testicles. The halves of the scrotum are divided by a wall of muscle. Externally you can see a line, called the raphe, that divides down the center of the scrotum. The scrotum's muscles are used to pull the testes closer to the body in order to protect or warm them The testes produce testosterone, the so-called "male" hormone, and they also produce sperm, which are formed in the testes and move into the epididymis to mature. The epididymis is a small organ that sits on top of the testicle. It is made up of a little bundle of squiggly tubes and is a "holding pen" for sperm. When ejaculation occurs, sperm are moved from the epididymis into the vas deferens, the tubes that take sperm up and out of the scrotum area and into other ducts so they can be ejaculated as a part of semen. Sperm that don't get ejaculated live in the epididymis for around four to six weeks before they die and are reabsorbed into the body. The epididymis and testicle are the two major organs inside the scrotum. They are anchored to the body by what is called the spermatic cord. The spermatic cord is a bundle of nerves and blood vessels that serve the testicle and epidydimis, plus the vas deferens, which is a long tube which carries sperm up and out of the scrotum so that it can be ejaculated. Internal Structures Vas deferens Seminal vesicles Prostate gland Cowper’s glands Urethra the vas deferens is a long tube which carries sperm up and out of the scrotum so that it can be ejaculated. Then it goes up into the body, where it empties into the seminal vesicles. This is the place where sperm get mixed up with some of the other ingredients that make semen. Sperm themselves are only about two to five percent of the volume of the semen that is ejaculated: the rest is other fluids. Those fluids are produced by several different glands: the prostate, the bulbourethral or Cowper's glands, and some fluids produced by the vas deferens and the seminal vesicles themselves, and are added to the semen mixture at various points along the way before the semen is ejaculated. The bulbourethral glands, also called the Cowper's glands, primarily produce a liquid sort of mucus. The prostate gland is a large, chestnut-shaped gland that surrounds a small part of the urethra within the body, below the bladder. It marks the spot where the seminal vesicles empty into the urethra, and is also the point at which fluids from the prostate (approximately 30% of the total volume of semen) get mixed into the semen. The prostate is very sensitive to pressure and touch. The fluid is ejaculated out of the urethra through a series of muscular contractions that begin in the vas deferens and continue all along the path that the sperm and fluid take in order to leave the body. Testosterone Primarily secreted by testicles Male reproduction is also regulated by hypothalamus, pituitary, and adrenal gland Roles Development of male genitalia in fetal stage Maintenance of sex drive Development of male secondary sexual characteristics at puberty (facial hair, deep voice, initiation of sperm production) Testis Tissue Testis Tissue (light micrograph) Annotation Spermatogenesis Occurs in testes in seminiferous tubules http://highered.mcgrawhill.com/sites/0072495855/student_view0/chapter28/animation__spermatogenesi s__quiz_1_.html The transformation of a round spermatid into a spermatozoon represents a complex sequence of events that constitute the process of spermiogenesis. No cell division occurs, but a conventional round cell becomes converted into a spermatozoon with the capacity for motility. The basic steps in this process (Figure 7) are consistent between all species and consist of (a) the formation of the acrosome (b) nuclear changes (c) the development of the flagellum or sperm tail (d) the reorganisation of the cytoplasm and cell organelles and (e) the process of release from the Sertoli cell termed spermiation http://highered.mcgrawhill.com/sites/0072495855/student_view0/chapter28/animation__stages_of_meio sis.html Role of LH, FSH, and Testosterone in Spermatogenesis Testosterone and follicle-stimulating hormone (FSH) are required to obtain full reproductive potential. In the testis, somatic Sertoli cells transduce signals from testosterone and FSH into the production of factors that are required by germ cells as they mature into spermatozoa. Follicle stimulating hormone may initiate the sequestering of testosterone in the testes, but once developed only testosterone is required to maintain spermatogenesis. However, increasing the levels of follicle stimulating hormone will increase the production of spermatozoa by preventing the apoptosis of type A spermatogonia. LH: hormone produced by gonadotroph cells in the anterior pituitary gland. It stimulates Leydig cell production of testosterone.[3] It acts synergistically with FSH. Leydig cells: also known as interstitial cells of Leydig, are found adjacent to the seminiferous tubules in the testicle. They produce testosterone in the presence of luteinizing hormone (LH). Sperm Overview of Testis & Spermatogenesis