MENTAL HEALTH & Substance Abuse Concurrent Disorders SWRK
advertisement

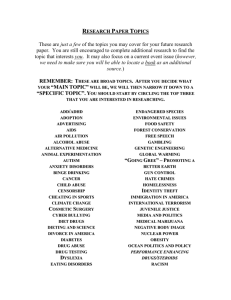
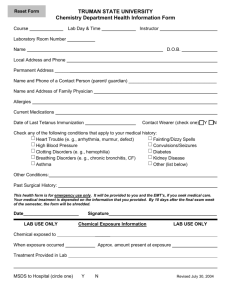
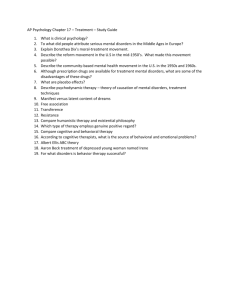
MENTAL HEALTH & Substance Abuse Concurrent Disorders SWRK 2083 Keith Cameron, M.A., M.B.A. Agenda Week 1 Introduction Course Outline & Administrative Issues Introduction to Concurrent Disorders Definition of Key Term Clinical Complexity Class practical exercises Introduction Keith Cameron, M.A., M.B.A. Contact Information Kcameron75@gmail.com No contact at the College Web site: http://www.cameke.pbworks.com It is your responsibility to access the web-site for power point presentations They will be posted by the end of the day on the Tuesday prior to class I will not be bringing copies to class Other information may be posted that is FYI only but may be beneficial in assignments or the test Course Outline EVALUATION SYSTEM: Week 3 – Multiple Choice Quiz (20%) Week 4 – Small Group Work – 3 maximum (30%) Week 7 – Final Multiple Choice (40%) Attendance (10%) Open book and work in pairs Those that have been granted job status will be prorated out of 90 Religious holidays. It is the student’s responsibility to discuss this issue with your professor at least one week before the holiday. Students registered with Disability Services are required to supply confirming documentation to the professor and inform him/her of any plans to write tests in private It is your responsibility to read and understand the course outline. Ask if you are not sure Course Outline – Cont’d ASSIGNMENT POLICY: PLS. READ CAREFULLY! Group work is submitted at the end of class. If 1 assignment is missed You must contact the professor at the latest ( no documentation is required) by email If you have contacted the professor, only then will be eligible for a make up after the final test on week 7 If you miss a second assignment: on the day of the assignment You must contact the professor on the day of the assignment and must provide documentation within one week to access any accommodation Groups will consist of 3 members Each member is to participate in written response Members are expected to participate equally and remain until the work is completed. Groups who sign in a missing group participant will be liable for sanctions as a whole ( i.e. 0 on that assignment) To view George Brown College policies go to www.gbrownc.on.ca/policies General Comments Please ask questions If you don’t know others also don’t know It is your right to have explanations and clarifications Very often there are not right and wrong answers I would request that any backbench talking be done outside the class This is disturbing to me and the rest of the class I will not talk above other people Turn cell phones off Because I say it doesn’t mean it is right If there is an emergency call awaiting let me know Keep assignments including scantrons in case of a discrepancy in marks. No marks will changed without this back-up support A Few Pointers Readings Reading package available at College Note that when you first open “Health Canada” document it is in Roman numerals – keep scrolling down until you get to the page numbers Note page number on the document will not correspond to the scroll down pages on the left Mental Illness..................S. Abuse: How we define them Context of Behaviour Social Deviance Persistence of maladaptive behaviours Subjective distress Severity Impact on functioning Tolerance Withdrawal symptoms Need more, same effect Persistent drive for substance, or failure to cut back Time spent getting it Reduce social/work activities Use despite health/social problems Some Themes for the Course Complexity Assessing Concurrent Disorders (CD) What came first? What do we treat first Causes of CD What came first? What do we treat? Treatment Numerous MH disorders combined with different disorders Age/demographics What went wrong in childhood? Focus Mood + Alcohol Anxiety + Alcohol Psychosis & Cannabis Definition What is your understanding of the term Concurrent Disorders What it is not! What do We Mean by Concurrent Disorders? At least one mental health disorder as defined by DSM-IV Plus substance abuse or dependence as defined by DSM-IV Multi combinations and variations, including multi-morbidity Across drugs Across mental disorders Demographics/cultural groups Abuse vs. Dependence Substance abuse is a pattern of drug, alcohol or other substance use that creates many adverse results from its continual use. The characteristics of abuse are a failure to carry out obligations at home or work, continual use under circumstances that present a hazard (such as driving a car), and legal problems such as arrests. Use of the drug is persistent despite personal problems caused by the effects of the substance on self or others. Substance dependence has been defined medically as a group of behavioural and physiological symptoms that indicate the continual, compulsive use of a substance in self-administered doses despite the problems related to the use of this substance. Sometimes increased amounts are needed to achieve the desired effect or level of intoxication. Consequently the patient's tolerance for the drug increases. Withdrawal is a physiological and psychological change that occurs when the body's concentration of the substance declines in a person who has been a heavy user. Definition in Canada (Similar in the USA) “A combination of mental/emotional/psychiatric problems with the abuse of alcohol and/or other psychoactive drugs…any combination of mental health and substance use disorders, as defined in DSM IV.” (Cooper & Calderwood in readings) In definition, the DSM–IV is used as the tool for diagnosis (Axis 1 & 2) Some Terms CAMI: chemically abusing – mentally ill MICA: Mentally ill – chemically abusing SAMI: Substance abusing – mentally ill Co-occurring (the US) ‘Double-jeopardy’ What is a Dual Disorder?? Not Dual Disorders People with MH + Substance abuse may have more than 2 disorders Dual Disorders In Canada, refers to Developmental Delay & a Mental Health issue Concurrent Disorders In Canada, captures complexity of substance abuse with mh Prevalence Data From Journal of American Medical Association Large overlap: between substance use and mental health disorders Most clients who actually seek treatment have a concurrent disorder Some Stats 50% of seriously mentally ill affected by substance abuse 90% of mentally ill smoke heavily 77% of those treated for alcohol-related disorders have experienced at least one other psychiatric disorder in their lifetimes. Some Specifics Schizophrenia 47% also have a substance abuse disorder, which is 4x the risk of the general population Bipolar Disorder 61% also had a substance abuse disorder which is 5x the risk of the general population Specific Risks Compared to general population the lifetime risk for developing alcohol dependence is: 21 times higher for Antisocial Personality 6 timers higher for those with Mania 4x higher for those with schizophrenia 2x higher for those with panic disorder, major depression, & OCD Most Common Combinations Specifically Mood Disorder plus Alcohol Anxiety Disorder plus Alcohol Five Most Common Groupings (Health Canada) 4. Substance Disorders Substance Substance Substance 5. Other Substance Use & MH 1. 2. 3. Use + Mood & Anxiety Use + Severe & Persistent MH Use & Personality Disorders Use + Eating Disorders Key to Practitioners Only a minority of substance abusers and those with mental health problems reach out for help….but… “…those in the general population with concurrent disorders present the highest probability of seeking treatment.” Kessler Key--- US Study: Respondents with alcohol use disorders were five times as likely to see help when they also had a mental health problem. “Those who seek help are the most severe cases in the general population…and are more often readmitted to treatment.” Article: “Multiple Identities, Multiple Barriers”: U. Chandraseskera “Intersectionality:” ‘The experience of living with multiple stigmatized identities, facing multiple layers of discrimination.’ Complexity = Multiple Identities Each with its own unique issues… S Abuse M Illness Class New Canadian Gender LGBTQ People of Color Consequences of Having a Concurrent Disorder Statistically, clients have a greater propensity for violence, medication non-compliance, and failure to respond to treatment…compared with clients with substance abuse only or mental illness only “These consumers are in and out of hospitals and treatment programs without lasting success.” (NAMI) Treatment takes longer to work Consequences -- ‘Downward Drift’: Mental illness lands clients in poor housing, in neighborhoods where drug use prevails…inability to form social relationships, isolation can lead to joining the drug sub-culture Consequences -- Leads to homelessness or jail: Half of the mentally ill homeless have substance abuse problems 31% a concurrent disorder 16% of prison inmates have concurrent disorders Leads to overall poorer physical health and greater chance of relapse “these consumers are in and out of hospital and treatment programs without lasting success.” (Nami) Services lack integration “Often only one of the disorders is identified. If both are recognized, the individual may bounce back and forth between services, or be refused service by one of them….Fragmented and uncoordinated services create a service gap for persons with co-occurring disorders.” (NAMI) Why CD Clients Quit Treatment Enter treatment in crisis or chronic state Therapeutic alliance tougher to establish Treatment streams not integrated (one disorder recognized) Clients need longer-term treatment that many agencies do not offer Pattern of failed relationships, abuse: attachment issues Double Stigma Is it better to be drug user or a mental health consumer? Mental Health Becoming less stigmatized More education Better outcomes Addictions Still seen as a moral failure Judged more harshly Internalized Stigma Addiction: harsh judgment by our culture creates more durable internal stigma Beliefs: I’m a loser, I’m a bad person, I don’t deserve help, I don’t deserve love 1+1 = more than 2 Substances make MH problems worse Substances mimic or hide MH problems Substances used to relieve MH symptoms (Self-medication) Substances can make MH meds less effective Substances can lead to clients forgetting to take MH meds Relapse with one triggers symptoms of other problem Consequences for Treatment Overall, poor outcomes: chronic course Poor physical health High relapse rates ‘Recidivism’ So: clients more likely to seek help, and also to quit help Treatment “Co-existing mental disorders increase the probability of abandoning treatment prematurely.” WHY? How Many Concurrent Combinations Are There? Bio-Psycho Social Model Review A framework that incorporates the NATURE vs. NURTURE controversy Examines the positive strengths of the consumer Recognizes the biological predisposition of mental illnesses & addictions Recognizes the negative and positive elements in the environment Organizes information in a way that can be communicated and include the consumer in decision making Recognizes the importance of the consumer in the treatment process Group Assignment As a group list your experience the last time you drank a lot of alcohol? Biological/Psychological/Social-Spiritual + Behavioural Biological Psychological Social Behavioural List Features of Depression Consider such things as thinking, judgment, inherited vulnerability, depressed CNS, memory, social functioning, mood Biological Psychological Social Behavioural Alcohol Abuse vs. Depression How do we distinguish depression and alcohol abuse? Does alcohol abuse mask depression? Which came first? Does one cause the other? Are they both hereditary or environmental? Common pathway Assessment is challenging Add Other Factors That May Affect Assessment and Treatment