JHWS Delivery Plan 1 Work together to address health inequalities
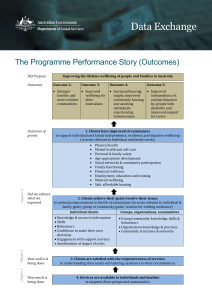
advertisement

Gloucestershire Health and Wellbeing Board Report Title JHWS Working Together to Address Health Inequalities Item for For information decision or information? Sponsor Sarah Scott Author Helen Flitton Organisation GCC Key Issues: The draft Health Inequalities Plan is presented to the Board for comment and discussion. There has been a very positive response from partners however discussions are ongoing for several of the activities and meetings are planned over the coming two months to ensure that priorities are joined up and activities agreed across partners. Some district level outcomes are included on the obesity, alcohol and older people Delivery Plans and are therefore not included in this plan. Recommendations to Board: The Board is asked to give constructive feedback on the activities included in the plan and the approach in general. Financial/Resource Implications: Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 JHWS Delivery Plan 1 Work together to address health inequalities GHWB Sponsor: Sarah Scott Why is this a priority? Commissioning Lead: Sue Weaver Gloucestershire is one of the healthiest counties in England; overall health outcomes are better than the national average with premature death rates from all causes falling over the last ten years. However, the health and wellbeing of some of our communities is not improving at the same rate as others and large health inequalities exist, with some groups having significantly shorter lives and suffering more illness and disability than others: A man living in Kingsholm has a life expectancy from birth of 73.2 years, 13.9 years shorter than a man living in Churn Valley (Cotswolds) A woman in St Paul’s has a life expectancy of 77.8 years, 13.3 years shorter than a woman in Wotton-under-Edge (Period: 2008 – 2012, www.localhealth.org.uk 2015) The infant mortality rate in the Forest of Dean is 4.3 per 1000 live births, compared to 1.9 per 1000 in Cotswold. Health inequalities are preventable and unjust differences in health status experienced by certain population groups. They arise from social inequalities, themselves the result of unequal distribution of factors influencing health, such as housing, environment, social background, income, employment and education. Around 2% of the county’s population live in areas considered to be amongst the most deprived 10% in the country (UG-JSNA 2015). These areas fall within the urban centres of Gloucester and Cheltenham and are: Podsmead; Matson and Robinswood; St Paul’s; St Mark’s; Kingsholm and Wotton; Westgate 1 and 3 and Hesters Way. Furthermore, 18,300 local children live in poverty (CYPPP 2014 - 2015). Residents living in our most deprived communities are more likely to: experience crime, have a low birth weight baby, leave school with no work, education or training destination, die prematurely, and become dependent on community health and care services. Other factors contributing to health inequalities are: differences in individual behaviours (i.e. smoking, drinking, physical activity and eating habits), rural isolation and poor access to and effective use of healthcare, which contributes to at least 15-20 percent of inequalities-related mortality (NHS England, 2013). There is evidence (from routine health service data) that an inverse care law exists so that those who most need health care are least likely to receive it and those that are in least need of health care use services more (HSJ vol 111, 5760 pp37). Among others who suffer poorer health and wellbeing outcomes are: people from black or minority ethnic communities; people living with a physical or learning disability; the homeless; young offenders and people with mental health problems. For example, people living in England with mental illness die on average 15-20 years earlier than those without, often from preventable causes (Chief Medical Officer, 2014). There is a strong economic case for addressing health inequalities. Inequalities contribute to financial pressure on health and social care and to an 2|P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 estimated annual cost of between £36 billion and £40 billion through lost taxes, welfare payments and costs to the NHS (Marmot Review, 2010). A key message from the Marmot Review (2010) was that focusing solely on the most disadvantaged will not reduce health inequalities enough – actions must be universal, but with a scale and intensity that is proportionate to the level of disadvantage – an approach called ‘proportionate universalism’. By adopting such an approach, and working together with individuals and communities, and with organisations across the system we can help to address these inequalities. What we are going to do: Action to reduce inequalities requires focus across the causes including: the wider determinants (education, employment, financial and environmental), the modifiable risk factors for disease (both primary and secondary prevention) and accessibility and responsiveness of health services. Interventions to achieve short term (less than five years) impacts can have a sizable impact on life expectancy. These include actions to prevent cardiovascular diseases, early identification of cancers and the management of long term conditions. However, these should be combined with other interventions that aim to impact on outcomes in the medium term (from 0 to 10 years), such as lifestyle changes, and an impact on outcomes in the longer term (from 0 to over 10 years), such as education and employment. The actions and interventions identified within this plan are guided by the following principles: Outcomes focused: monitoring our progress in terms of meaningful impact on local people (‘outcomes’) - not just looking at what activities have taken place (‘outputs’) Service user and community voice will inform all that we do and how we do it Needs rather than demand-led: interventions will be focused where there is the greatest capacity to benefit Proportionate Universalism: actions must be universal, but with a scale and intensity that is proportionate to the level of disadvantage All interventions will be informed by evidence of impact and where this is not available will be supported by a sound evaluation Sustainability: building capacity supporting individuals and communities to help themselves and each other and to become more resilient; fostering self-care and independence and improving levels of health literacy Parity of esteem: ensuring we are equally focused on improving mental as well as physical health, and reducing inequalities in both Starting early: Giving every child the best start in life through focusing on pregnancy and the first months and years of life Long-term commitment: A commitment to ‘seeing it through’ – a long term sustained strategic approach, which includes a range of short and medium and long term actions and interventions 3|P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 Focusing on both communities of ‘place’ and communities of ‘interest’: (i.e. people who share common characteristics / challenges). Our actions will include those that are applied across the whole county and others that are district or locality-led. Key Risks and mitigating actions Risk Lack of engagement across the system Mitigating Action Communications and Engagement Strategy to enable stakeholders to stay informed and to track progress. Provider engagement events held on a regular basis. Involvement of partners and stakeholders in development of plans and activities. Board level Sponsors to champion activities amongst their networks. Diminishing resources Maintaining a system overview (through SIG) to ensure coordination of activity and to avoid duplication. Robust performance management to ensure where activity isn’t effective resources are directed elsewhere. Absence of robust data for some outcomes Tba Difficulties in attributing cause and effect to population level outcomes Tba Interdependencies The current and future health and social care needs of the citizens of Gloucestershire, including health inequalities, are assessed in the annually updated ‘Understanding Gloucestershire a Joint Strategic Needs Assessment’ (UG-JSNA) which can be found on the Gloucestershire Inform website: http://www.gloucestershire.gov.uk/inform/understanding The following strategies and plans include specific action to reduce health inequalities and these actions will not be duplicated within this delivery plan: Building Better Lives – an all age, all disability policy which includes actions on employment, reshaping services and new ways of working with some of the most vulnerable service users. Mental Health and Wellbeing Strategy – objectives include: more people will have good mental health; more people with mental health problems will recover; more people with mental health problems will have good physical health and fewer people will suffer avoidable harm. Improving Outcomes for Children, Young People and Families in Gloucestershire: a Strategic Joint Commissioning Framework for Children, Young People and Families - It is increasingly understood, and supported by growing bodies of evidence, that the outcomes achieved by children and young people during their childhood and adolescence impact significantly on life-long outcomes affecting health, wellbeing, employment prospects and 4|P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 life expectancy, to name but a few. This framework takes the principles and benefits of the existing early years framework and develops them into a broader approach across the whole of childhood, adolescence and young adulthood. Early Help and Children and Young People Partnership Plan 2015 – 2018 – focuses on areas where partnership working will really make a difference to the outcomes for our vulnerable children and young people including Looked After Children; children requiring safeguarding; children subject to the effects of poverty and children living in challenging circumstances. Youth Employment and Skills Strategy – the County Council’s commitment to help young people (14 – 24 yrs) to get the information and gain the skills, work experience and abilities they need to make a successful transition into employment. It is also aimed at supporting economic growth by helping businesses to access young people who can develop the skills that they need. Gloucestershire National Dementia Strategy Local Action Plan – objectives include good quality early diagnosis and intervention for all; improving awareness and understanding of dementia; providing training on cultural awareness for health and social care staff and providing good quality information for those diagnosed with dementia. Enabling Active Communities in Gloucestershire – a multi agency framework with the aim of building stronger, more sustainable communities and in turn improving the health and wellbeing of local people, drawing upon, and stimulating the provision of, the diverse range of assets within each local community. Better Care Fund Plan – pooled budget arrangements between the County Council and the Clinical Commissioning Group to try to ensure that people receive better and more integrated care and support. Objectives include flexible primary care provision over 7 days which will be accompanied by greater integration with mental health services, and a closer relationship with pharmacy services; strengthened integrated community teams; parity of esteem; empowering people to direct their care and support, and to receive the care they need in their homes or local community. Growing Older In Gloucestershire Plan – includes four steps to supporting people as they age: active individuals; active communities; getting people back to independence and being there when most needed. Joining Up Your Care – People are provided with support to enable them to take more control of their own health and wellbeing. Those that are particularly vulnerable will benefit from additional support. Gloucestershire Police and Crime Plan - includes trying to ensure older and more vulnerable people are not overlooked; reducing alcohol related crime and disorder; to deliver sensitive, relevant and effective policing to ensure our young people become law-abiding productive members of society. Healthy Individuals Plan – aims to enable people to have the knowledge, skills and confidence to self care and take more control of their health. Considers the social determinants of health – housing, education, employment, physical environment and inequalities. 5|P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 JHWS Delivery Plans 2016 – 2019 - Reducing Alcohol Related Harm; Improving Health and Wellbeing into Older Age and Reducing Obesity - Targeted activity to reduce health inequalities in relation to older people’s health and wellbeing, to alcohol and to reducing obesity will be included in the separate JHWS Delivery Plans. Improving Mental Health is covered under the Mental Health and Wellbeing Strategy. Gloucester City Council, Cheltenham Borough Council and Tewkesbury Borough Council Joint Core Strategy – The Joint Core Strategy (JCS) is a partnership between Gloucester City Council, Cheltenham Borough Council, and Tewkesbury Borough Council, supported by Gloucestershire County Council. The JCS was formed to produce a co-ordinated strategic development plan to show how this area will develop during the period up to 2031. Stroud, Cotswold and Forest of Dean Local Strategies – Strategic development plans to show how the Districts will develop during the period up to 2031. Strategic Economic Plan for Growing Gloucestershire – gfirst LEP Countywide Activity (targeted to need and not in other strategies and plans) Outcome Activity Baseline & target (population level outcome) Performance Measures (intervention or service level outputs and outcomes) Time (completion date) Resource (£ and funding source) Lead (organisation and officer) GCC/ GCS / NHS GCC GCC GCC Ruth Lewis Time to realisation of benefits (1-3yrs; 3-5 yrs; 510+yrs) Improving the wider factors that affect health and wellbeing (‘wider determinants’) Babies and Young Children develop well, are ready for, and transition successfully to, school tbc Parents have the confidence and Parent Support Programme Review is completed and Baseline: 52% of children are judged to have achieved a good level of development, measured at the end of the foundation stage in the final term of the academic year in which a child reaches the age of five The percentage of children achieving a good level of development at the end of reception tbc Tbc Review of parent support programmes is completed Tbc Sarah Hylton and Jane Lloyd Davis to formulate – awaiting decision on final outcome and activity 6|P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 skills to support their child’s healthy development provides evidence for decision making1 Current parent support programmes are reviewed for efficacy and value for money Family Learning Programme in Children’s Centres and provides evidence for decision making by January 2016 Baseline? Target? Improved employment opportunities and retention for young people2; people with disabilities; people with mental health problems and older people Employability Learning using in house delivery team and external providers Baseline: 2014/15? Target? Effectiveness of Family Learning Programme – 3 months and 6 month follow-up tbc Increase the numbers of learners, including Adults with Learning Difficulties and Disabilities, who progress to or re-enter employment, who work for longer, who change their skills set, who embark on a new career or who progress into further training, volunteering or self-employment. Tbc GCC Joanna Jackson; Churchill Audi Sally Lewis, GCC Adult Education Francis Gobey Karl Gluck Measured through the 1 Parent Support Programmes: PHE UCL Institute of Health Equity recommendation (2014). Marmot (2010). The quality of parenting that a child receives is considered the strongest contributory factor in the development of resilient, more confident and emotionally healthy children. The importance of parents (particularly mothers) adopting a healthy lifestyle during and after pregnancy, has a major positive influence over improving the health and life chances of their child (JHWS, 2012) 2 Employment opportunities: Comment on need insert. Employment is key area GHWB agreed to focus on. PHE UCL Institute of Health Equity recommendation (2014). Marmot (2010). 7|P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 adult education progression survey completed 3 months after end of course More homes across the County are healthier and safer to live in. Cat 1 hazards removed as a result of interventions by local authorities (grants/loans/signposting/ enforcement) Baseline: Number of cat 1 hazards across the county (taken from Housing Statistics return for each LA) Number and type of Cat 1 hazards removed Savings to NHS and wider society? Over the period of one (financial) year District council private sector housing teams Gloucester City Council Resource (£ and funding source) Lead organisation (officer) Julie Wight Target: Need to agree a target for Cat 1 hazards removed Helping people to live healthy lifestyles and make healthy choices (‘health improvement’) Outcome Activity Baseline & target (population level outcome) Performance Measures (intervention or service level outputs and outcomes) Time (completion date) Time to realisation of benefits (13yrs; 3-5 yrs; 5-10+yrs) 8|P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 Fewer women will smoke at time of delivery3 Review stop smoking services as part of health behaviour review and retender stop smoking support from January 2017 Low birthweight term babies Review stop smoking services as part of health behaviour review and retender stop smoking support from January January 2017 £ tbc GCC (GCC. PH) (Tracy Marshall) £ tbc GCC (GCC. PH) (Tracy Marshall) £ tbc GCC (GCC. PH) (Tracy Marshall) tbc Smoking status at time of delivery Tracy / Temi to add any significant service improvement activity planned for pregnancgy for 2016 – 2017 i.e action plan that the service is working towards Fewer people with mental health problems smoke4 Targets tbc Targets tbc Smoking rate of people with serious mental illness Tracy / Temi to propose KPI tbc tbc tbc tbc 3 Smoking in pregnancy: Pregnant women who smoke are twice as likely to have a low birth weight baby. Low birth weight is linked to survival in early infancy and health in childhood and adult life. We also know that the numbers of low birth weight babies and sudden unexpected deaths are both higher in low income families (JHWS, 2012). 4 Smoking among people with mental health problems: Increased smoking is responsible for most of the excess mortality of people with severe mental health problems . Two out of every five cigarettes in England are smoked by people with mental health problems.Many wish to stop smoking, and can do so with appropriate support (Department of Health, 2010). 9|P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 2017 Tracy / Temi to add any significant improvment activity planned for 2016 2017 Fewer children aged 15 years smoke Extend delivery of ASSIST across all secondary schools Smoking prevalence age 15 years – regular smokers* (OPS equiv given no national data) tbc Fewer routine and manual workers smoke Review stop smoking services as part of health behaviour review and retender stop smoking support from January 2017 Smoking prevalence routine and manual persons aged 18 tbc Tracy / Temi to propose Tracy / Temi to propose KPI tbc tbc £ tbc GCC (GCC. PH) (Tracy Marshall) £ tbc GCC (GCC. PH) (Tracy Marshall) £ tbc GCC (GCC. PH) (Tracy Marshall) tbc tbc Tracy / Temi to add any significant improvement activity planned for 2016 2017 Fewer people with long term conditions smoke Review stop smoking services as part of health behaviour review and retender stop smoking support from January 2017 tbc tbc Tracy / Temi to add any significant serivce improvment activity planned for 2016 - 2017 10 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 Children in Gloucestershire have improved oral health5 and the gap for high risk groups is reduced Develop a targeted multiagency oral health promotion plan in response to the 2015 oral health needs assessment Percentage of 5-yearold children with decay Hospital admissions: 0-19 y/o for extraction of 1+ decayed primary /permanent teeth Number of key oral health information sessions to parents in pre-schools/ schools located in areas of high need March 2016 £60k p.a. (GCC, PH) GCC Temi Folayan (tbc) Number of toothbrushing packs distributed/supplied Percentage of looked after children who had their teeth checked by a dentist Rates of breastfeeding are improved6 and gap between deprived and affluent areas is reduced Undertake a review of evidence for improving breastfeeding rates among groups least likely to breastfeed and develop multi-agency improvment plan Breastfeeding initiation tbc once plan in place Dec 2015 £47k p.a. (GCC, PH) Breastfeeding prevalence at 6-8 weeks after birth GCC (David Squire) CCG (Helen Ford) 5 Oral Health: Significant preventible local inequalites relating to oral health with poorer outcomes among: children in care; people living in deprived communities; people with diabetes; older people with dementia and those living in residential or nursing care; gypsy and Irish travellers and children and adults with disabilites . Significant impact on health and wellbeing including school absence; mental health and wellbeing; quality of diet. Strong evidence for oral health promotion (PHE, 2014; NICE,2014 ). The NHS in England spending £3.4 billion per year on dental care. 6 Breastfeeding: UG-JSNA (2015) – breastfeeding rates static and significant inequalties persist – evidence that breasfed babies are at lower risk of gastroenteritis; respiratory infections; sudden infant death syndrome; obesity; type 1 &2 diabetes and allergies and subsequently less likely to be a cost to the NHS (Unicef UK 2015) 11 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 Improved nutrition among pregnant women and young children from deprived or vulnerable communities Healthy Start review7 Improved health outcomes for people with mental health problems Placeholder for action around improving health outcomes for people with mental health problems. Uptake of Healthy Start Review completed Oct 2015 tbc GCC (Sue Weaver) tbc tbc tbc tbc Tbc GCC Sue Weaver Actions to be identified and agreed as part of Mental Health and Wellbeing Strategy subgroup 3 plan. Subgroup meets on the 8th October Improved health outcomes for people with a learning disability Placeholder for action around improving health outcomes for people with learning disabilities. tbc tbc tbc tbc Tbc CCG Martin Ayres Actions to be identified by the HAG following 7 Healthy Start: Marmot Review (2010). Investing in giving children the best start in life and tackling child poverty is essential to reducing health inequalities and is a cost effective way of improving longer-term health outcomes and reducing pressure on health and social care services. 12 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 workshop on 7th Sept Improved health outcomes for people with a physical disability Placeholder for action around improving health outcomes for people with physical disabilities. tbc tbc tbc tbc Tbc ?? Resource (£ and funding source) Lead (organisation and officer) Time to realisation of benefits (1-3yrs; 3-5 yrs; 510+yrs) GCC Public Health: Teresa SalamiAdeti 1-3 years To be discussed with Lead Commissioner (?Chris Haynes) Protecting the population’s health from major incidents and other threat (‘health protection’) Outcome Improved uptake of Childhood immunisations Activity Targeted action in the five lowest performing GP practices in each Locality Focus MMR 2nd Dose & Hib/Men C Baseline & target (population level outcome) Performance Measures (intervention or service level outputs and outcomes) Q4 14/15 MMR uptake 95%< Hib/MenC Uptake 95%< Time (completion date) Elizabeth Luckett, NHS England South Birthday Card scheme with 5 worst performing practices Text messaging reminder service focus on 5 worst 13 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 performing practices Targeted support for worst performing practices through facilitator practice visits. Improved cervical screening coverage Cervical Screening Pilot targeting Polish women under 30ys. Q4 14/15 Cervical screening 80%< Targeted work with practises (GP list cleansing for specific population) Improved sexual health outcomes in vulnerable communities (as identified in SHNA) GCC Public Health: Teresa SalamiAdeti 1-3 years Elizabeth Luckett, NHS England South Breast Screening Campaign targeting women under 60 commencing in October Q4 14/15 Breast screening coverage <75% Health Equity Assessment (Sexual Health) Tbc Tbc GCC Public Health: Teresa SalamiAdeti Participatory Needs Assessment Reducing the numbers of people living with preventible ill-health and dying prematurely (‘healthcare’) 14 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 Outcome Reduce differences in under 75 mortality rate from all cardiovascular diseases Activity Review performance of new NHS HealthChecks at end of Q1 2015-16 Pilot outreach NHS Health Checks Review commissioning of NHS HealthChecks Baseline & target (population level outcome) Performance Measures (intervention or service level outputs and outcomes) Time Take up of the NHS Health Check programme (cumulative percentage of those offered) Tbc – PHE ambition is 66% uptake Take up of the NHS Health Check programme (cumulative percentage of those eligible) Resource (£ and funding source) Lead (organisation and officer) Mar 2016 £ (GCC, PH) GCC, PH (Sue Weaver), CCG (Matt Pearce) Mar 2017 Via Primary Care Offer 2016/17 Hannah Layton (CCG) (completion date) Time to realisation of benefits (1-3yrs; 3-5 yrs; 510+yrs) Set local targets by age, gender, deprivation and ethnicity?? Uptake by age, gender, deprivation and ethnicity) Improving the management of high blood pressure in the community Case finding for patients with hypertension via opportunistic checks, or NHS Health Checks or methodical review of caseload People from the most deprived areas are 30% more likely than the least- Implement a GP education programme improving skills of HCP’s in effective management of difficult hypertension in a. Estimated total prevalence (diagnosed and undiagnosed) 2011 25.8% Number of recorded patients with hypertension against expected prevalence by practice 2-3 years b. Recorded prevalence (diagnosed)13.8% 2012/13 15 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 deprived to have high blood pressure, and the condition disproportionate ly affects some ethnic groups including black Africans and Caribbean’s primary care Improving the management of Atrial Fibrillation in the community to prevent stroke Improved anticoagulant therapy for individuals with Atrial Fibrillation Number of recorded patients with Atrial Fibrillation 11,688 (1.9%) c. Number of recorded patients with Atrial Fibrilation against expected prevalence by practice Mar 2016 Via Primary Care Offer 2015/16 and joint education project with the Academic Health Science Network Hannah Layton (CCG) 1-5 years with ongoing benefits Mar 2017 Current investment in Expert Patient Programme £60k CCG Matt Pearce 1-3 years Incidence of Ischaemic Stroke Promoting effective self management (of condition) People with long-term conditions disproportionate ly live in deprived areas and have access to fewer resources of all Ensure self management services are sufficently targetting areas of high heallth needs Take-up of Expert Patient Programme and specialist self management services 70% of EEP participants are from IMD deciles 1-4 16 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 kinds. Reduction in the number of people in Gloucestershire with nondiabetic hyperglycaemia Implement an evidencebased diabetes prevention programme as part of NHS England’s National Diabetes Prevention Programme (subject to successful bid) Number of participants taking up intervention Mar 2017 Funded by NHSE Sue Weaver (GCC) /Matt Pearce (CCG) 1-3 years Number of homeless people admitted to GHT Referrrals to Time to Heal March 2016 CCG funded CCG 1-3 years Reduced length of stay Baseline data 13/14 125 individuals seen by Homeless Healthcare team Reduced readmissions Seeking to establish 3+2 year contract with closer alignment to GCC housing strategy Recorded pre diabetes 59,111 (estimated via HSE data) People are at increased risk of developing Type 2 diabetes. They are also at increased risk of other cardiovascular conditions Improve outcomes for patient groups who have trouble accessing the health service in a traditional manner i.e. homeless people admitted to hospital Estimated number of people aged 16 and over who have nondiabetic hyperglycaemia by local authority. Establish a clear pathway from hospital to safe discharge supported by community services Reduced self-discharge Referrals to other services Debbie Clark £££’s Helen Vaughan Referrals to Time to Heal 14/15 of 155 individuals The life 17 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 expectancy of a street homeless person is 42 years compared with 74 for men and 79 for women Health care services are accessible to all individuals irrespective of gender, race, disability, age, sexual orientation, religion or belief Equality is embedded throughout health care commissioning through the implementation of the CCG’s Equality and Valuing Diversity Strategy and associated action plan Assessment and grading of performance will be undertaken against the eighteen goals and outcomes of EDS2. Action plan and ongoing monitoring in place Mar 2018 Utilising existing resources Caroline Smith (CCG) 1-3 years Improve equity of access to health care services Undertake analysis to establish the number of unregistered patients in Gloucestershire and explore TBC Number of unregistered patients presenting at A&E Mar 2016 Utilising existing resources Maria Metherall (CCG)?? 1-3 years Develop a patient facing platform (reiteration of Gcare) that provides clear, evidence based and understandable patient Number of website hits Awareness of the web based platform amongst the community particularly in areas of need Mar 2017 TBC Ruth Hallett (CCG) / Matt Pearce (CCG) 1-3years Access to healthcare is a known determinant of health Increase access to services by providing information, advice and guidance on 18 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 available services information Low health literacy is associated with poorer health outcomes Reduction in avoidable variation in care The existence of persistent unwarranted variations in health care contribute to health inequalities Use the principles of system leadership to understand the needs of a local community (i.e. Westgate corridor) and coordinate action around a particular health inequalities issue. Development of a community based approach to understand local variation in an area of high health need TBC Mar 2016 TBC Matt Pearce Becky Parish. Andrew Hughes (CCG) ??? (TBC) 1-3 years Shifting focus from the patients that present most frequently in practices to the wider population that they serve District Level Activity (targeted to need and aligned to priorities identified in the Locality Development Plans 2015 - 2017) Cheltenham – being updated following Locality meeting on 7th September Outcome Activity Baseline & target (population level outcome) Performance Measures (intervention or service level outputs and outcomes) Time (completion date) Resource (£ and funding source) Lead (organisation and officer) Time to realisation of benefits (1-3yrs; 3-5 yrs; 510+yrs) 19 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 e.g. Families are prevented from needing high level support Cheltenham Inspiring Families Project. Cheltenham Borough Council e.g. the harm that alcohol causes individuals and communities in Cheltenham is reduced Cotswolds Outcome Ensure people with health conditions or disabilities can access tailored specialist exercise, helping to manage conditions and Activity Baseline & target (population level outcome) Performance Measures (intervention or service level outputs and outcomes) Time (completion date) Develop and deliver the Active Lifestyles exercise on prescription scheme, including the gym programme and specialist exercise classes (Cardiac Rehab, etc.) Ongoing Explore potential to roll March 2016 Resource (£ and funding source) Lead (organisation and officer) Time to realisation of benefits (1-3yrs; 3-5 yrs; 510+yrs) Part of the CDC leisure contract Will require contribution by schools or external 20 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 reduce obesity out to school sites (Tetbury and Fairford) funding Provide support to those whose mental health is negatively affected by financial worries Support the continued presence of the Citizen’s Advice Bureau in Cirencester, telephone and online support and the roll out of outreach support across the district Ongoing SLA in place between Stroud CAB and CDC Address local health inequalities through communitybased projects Deliver the Health Inequalities Fund supported projects and monitor their impact Ongoing Funded by GCC HIF Performance Measures (intervention or service level outputs and outcomes) Time Resource (£ and funding source) Lead (organisation and officer) New participants through GP referral scheme Dependant on future funding sources £31K health inequalities grants GCC PH FODDC Forest of Dean Outcome Healthier and more active communities in general and targeted to Activity Delivery of GP referral schemes to include; Weight management, cardiac rehabilitation, respiratory rehabilitation, Baseline & target (population level outcome) (completion date) Time to realisation of benefits (1-3yrs; 3-5 yrs; 510+yrs) Tess Tremlett Gary Deighton 21 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 areas of greatest need. (Use of Maiden and JSNA info) falls prevention, back care, Parkrun, health walks, health classes, buddy scheme and health promotion New management of 5 leisure centres across the FoD district Volunteers Baseline and target data needed Consessionary rates available for leisure members on a means tested benefit Freedom Leisure (Andy Barge – FODDC) Free swimming for the over 75s and the under 8s Measured by uptake? To improve the health and wellbeing outcomes for people for whom "wellbeing" services are most likely to address their needs Social Prescription Pathway To keep GP surgeries and patients informed about healthy living options Healthy living project 94 in year 2014/15 Numbers referred and the difference/impact made Will you set a target for this? How will you measure difference/impact made? Sept 2016 £47K FODDC CCG (Prime Ministers Challenge funding) Tess Tremlett Gary Deighton £5K Locality Exec group 22 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 To provide advice, support and advocacy for those of greatest need To reduce social isolation and support people in their own homes for as long as possible Service level agreements with VCS orgs: CAB Each contract has performance indicators that are reported against in their quarterly monitoring report. Age Concern FoD (to deliver a hot meal service at home and provide befriending support) 31 March 2016 FODDC budgets; FODDC Tess Tremlett £86,275K p/a All SLAs are reviewed annually and are subject to budget approval in February £7,641 p/a Artspace To support people of all ages and abilities to access ‘arts’ activities especially for those on low income To support young people especially those in most need of support To provide transport for those who do not have their own access to £9,731 p/a Provision of youth cafes/drop-in centres at Cinderford, Lydney and Newent £13,592 p/a FODDC Malcolm Vine Work with G3 – supported housing for young people The Community Transport project Lottery targets and set milestones October 2018 £310K FODDC Big Lottery Lena Maller 23 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 transport Communities in the Forest of Dean are dementia friendly. Community information and awareness raising sessions Facilities, public spaces and houses are ‘dementia’ friendly New affordable housing developments and housing with care Prevention of homelessness FoDDC has a statutory duty to assist those who find themselves homeless Reducing the number of deaths during winter Good quality affordable Housing to those on low incomes Enabling older people to Baseline: 2014/15 delivery Number of attendees: Target: To at least match previous years performance Warm and well partnership Number of sessions: Reviewed annually against FODDC corporate priorities and budget FODDC budgets FODDC Lena Maller FODDC Malcom Vine FODDC Budgets FODDC Malcom Vine FODDC Malcom Vine Ensure that alternative accommodation is available for families and young people so that B&B is avoided Safe at Home scheme and the disabled facilities grants Community Alarm service; Linkline service in the Forest and Careline FODDC Deb 24 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 remain living safely in their own homes and to enable older and frail people to leave hospital and return to their own homes. service in the Cotswolds. Hughes Gloucester City Outcome e.g. Residents of Westgate Ward have improved quality of life Activity Baseline & target (population level outcome) Performance Measures (intervention or service level outputs and outcomes) Time (completion date) Resource (£ and funding source) Gloucester City ‘Our Place’ project Lead (organisation and officer) Time to realisation of benefits (1-3yrs; 3-5 yrs; 510+yrs) Gloucester City Community Partnership Stroud Outcome Improved Physical and Mental Activity Cardiac Rehab Classes Baseline & target (population level outcome) Performance Measures (intervention or service level outputs and outcomes) Time Take up of Classes Number of clients attending the classes March 2016 Needs refining + (completion date) Resource (£ and funding source) Lead (organisation and officer) Internal Funding & Stroud District Council Time to realisation of benefits (1-3yrs; 3-5 yrs; 510+yrs) What is the 25 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 figures for baseline and targets Wellbeing Promoting the Health & Wellbeing of our community Improved Physical and Mental Wellbeing Respiratory Rehab Classes Take up of Classes Number of clients attending the classes period for which this is being measured – the plan doesn’t start until April 2016? class fees Hannah Drew March 2016 Internal Funding & class fees Stroud District Council Hannah Drew Promoting the Health & Wellbeing of our community Residents in Stroud District on low incomes can improve their housing conditions and as a result prevent ill health and improve their wellbeing Healthy Homes Loan for low income households where a category one hazard* exisits. 33% of owner occupiers live in a property with a category one hazard * defects in a home that threaten the health and safety of the occupants may be eligible Uptake of loan by individual home owners Ensuring occupants are living in safe, Mandatory Licensing Number of Mobile Homes, Caravan Sites, Houses in Multiple Occupation (HMO) Number of essential repairs* to homeowner’s properties in the Stroud District. Budget timescale??? ??? SDC £15,000 per property Stroud DC Jon Beckett £200,000?? Number of homes inspected by an Environmental Health Officer to ensure SDC Stroud DC Jon Beckett 26 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 healthy homes Promote and Improve Energy Efficiency in the Home to reduce cold related illness which can lead to excess winter death Ensuring occupants are living in safe, healthy homes through improving housing conditions in the private rented sector Advice on saving energy, renewable technologies and financial assistance via the Severn Wye energy advice line Target 2050 loans of up to a maximum of £10,000 for energy efficiency improvements in the home. Advice to landlords, tenants and agents on property letting standards especially overcrowding and housing conditions and fire safety. licensed and inspected standards are met and the home is safe with adequate facilites 15.7% of households in Stroud living in fuel poverty Number of households in fuel poverty reduced Reduction in the Excess Winter Death rate Number of properties solid wall properties insulated SDC Stroud DC NHS Jon Beckett GCC SWEA Number of properties connected to the gas main. 42% of occupiers in the private rented sector live in a home with a category one hazard . Number of properties with energy efficiency improvements made Number of category one hazards removed from private rented properties SDC Stroud DC Jon Beckett Number of properties accredited on Fit to Rent scheme Landlord training days Fit to Rent Property Accrediation Scheme Enforcement or poor housing condtions to ensure property improvements are made where category one hazards are found 27 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 Tewkesbury Outcome Improving knowledge of, and links to VCS for all public sector partners To support, encourage and enable the voluntary sector to increase participation in healthy lifestyles Activity Baseline & target (population level outcome) Performance Measures (intervention or service level outputs and outcomes) Time Resource (£ and funding source) Lead (organisation and officer) Developing Social Prescribing as core business For Tewkesbury CCG: people accessing support via SP Number of cases managed, reduction in visits to GP December 2016 Tewkesbury: £5kpa Tewkesbury CCG (Jeremy Welch) Local Area/Asset Coordination Roll out LAC to all areas of the borough to support Place Programme Mapping/directory of services and assets October 2016 Core ASC budget ASC: Margy Fowler Increase number of volunteer sports/activity coaches New groups established and increase in participation Numbers trained/qualified March 2017 HIF budget to be agreed TBC (Neil Meynell) (completion date) Time to realisation of benefits (1-3yrs; 3-5 yrs; 510+yrs) Active People Survey Operational Oversight for Delivery Plan: 28 | P a g e Joint Health and Wellbeing Strategy Delivery Plan 2016 - 2019 GHWB Strategy Implementation Group (SIG): The Strategy Implementation Group (SIG) will oversee the delivery of the Health Inequalities Plan. The group meets once or twice between each Health and Wellbeing Board meeting and membership consists of: Director of Public Health (Chair) CCG representative x2 Adult Social Services representative Children’s and Families representative Public Health representative x 2 Healthwatch representative VCS Alliance representative Districts’ representative x 2 PCC representative Head of Performance and Need, GCC Delivery Plan Commissioning Leads x4 Others by invitation 29 | P a g e